Abstract
Purpose
Vitamin D inadequacy is a global health concern in athletes as well as the general population. Whilst the role of vitamin D in skeletal health is well defined, there remains uncertainty over whether vitamin D supplementation has an added benefit beyond bone health.
Methods
This randomised placebo-controlled trial in healthy male and female Gaelic footballers (n = 42) investigated the effect of vitamin D3 supplementation [3000 IU (75 µg) daily for 12 weeks, via an oral spray solution] on VO2 max which was the primary outcome measure. Secondary outcomes included skeletal muscle and lung function.
Results
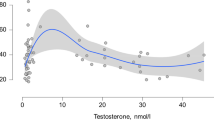
Supplementation significantly increased total 25-hydroxyvitamin D concentrations compared to the placebo group (mean ± SD change from baseline, 36.31 ± 32.34 vs. 6.11 ± 23.93 nmol/L, respectively; P = 0.006). At baseline, 50 and 22 % of footballers presented with vitamin D insufficiency (31–49 nmol/L) and deficiency (<30 nmol/L), respectively. Total 25-hydroxyvitamin D concentration did not significantly correlate with any measure of physical performance. Analysis of covariance (ANCOVA) models demonstrated that vitamin D supplementation over 12 weeks had no significant effect on VO2 max (P = 0.375), vertical jump height (P = 0.797), left and right handgrip strength (P = 0.146 and P = 0.266, respectively), forced vital capacity (P = 0.573) or forced expiratory volume at 1 s (P = 0.665), after adjusting for confounders. The high prevalence of vitamin D inadequacy observed in this cohort of collegiate Gaelic footballers supports the need for vitamin D supplementation during wintertime to avoid being at risk of poor bone health.
Conclusions
Twelve-week daily supplementation with 3000 IU (75 µg) vitamin D3 successfully resolved deficiency but did not have any significant effect on VO2 max, skeletal muscle or lung function.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vitamin D insufficiency and deficiency can be defined as a total serum 25-hydroxyvitamin D (25[OH]D) concentration below 50 and 30 nmol/L, respectively [1]. Such low total 25(OH)D concentrations are widespread, and a growing number of studies around the globe have identified this health concern in athletes [2–5]. Vitamin D and its metabolites are renowned for their pivotal role in establishing musculoskeletal health during childhood and adolescence and in hindering the development of skeletal pathology [6]. In addition, a growing body of evidence has demonstrated the importance of vitamin D beyond bone health on immune, cardiopulmonary and skeletal muscle function [7].
Biologically inactive total 25(OH)D is comprised of 25(OH)D2 and 25(OH)D3, compounds that are both formed following hepatic hydroxylation of vitamin D2 (ergocalciferol) and vitamin D3 (cholecalciferol) [8]. Ergocalciferol is derived from fungi exposed to ultraviolet B radiation (UVB) [9]. In humans, cholecalciferol is produced following exposure of cutaneous cells to UVB at a wavelength of 290–315 nm and is also present in oily fish, eggs and liver [10]. Calcitriol (1,25-dihydroxyvitamin D (1,25[OH]2D) is formed subsequent to renal hydroxylation of 25(OH)D, and it is this hormonally active compound that has been implicated in numerous processes involving the immune, cardiovascular and respiratory systems [11]. Binding of 1,25[OH]2D to its nuclear receptor (VDR) results in the formation of a VDR-retinoid X receptor (RXR) heterodimer that enables 1,25(OH)2D to act as a transcriptional regulator through binding to response elements located in the DNA of vitamin D target tissues [12].
In observational studies of both athletes and non-athletes, total 25(OH)D concentration has been positively associated with measures of aerobic fitness although findings have not been consistent [13–19]. One such measure is VO2 max, the maximal volume of oxygen utilised, per minute, during exhaustive exercise, which is considered the gold-standard measure of aerobic fitness and is related to distance covered in field games [20]. VO2 max is determined by a range of overriding factors including cardiac output, oxygen transit time and oxygen saturation [21].
A major limitation of existing observational research in this area is its inability to determine causality, and therefore, it is not known whether total 25(OH)D concentration is a cause of increased VO2 max or simply a result of reverse causation, perhaps owing to increased outdoor training time [22]. Despite the paucity of randomised controlled trials investigating this relationship, there is significant evidence of mechanisms by which vitamin D may influence factors that determine VO2 max [23–25]. One such mechanism is the ability of 1,25(OH)2D to suppress mRNA expression of hepcidin, the negative regulator of systemic iron concentration, an action which has been associated with increased expression of ferroportin in hepatocytes and monocytes [24]. Ferroportin is the sole iron export protein in humans and plays a crucial role in maintaining erythropoiesis, a contributory factor to VO2 max [26–28]. Studies in both healthy adults and patients with chronic kidney disease have demonstrated that vitamin D supplementation significantly decreases systemic hepcidin concentrations [24, 25]. Collectively, these findings raise the question as to whether optimising total 25(OH)D concentrations has a beneficial effect on VO2 max in athletes.
The primary aim of the current study was to test whether athletes who received daily vitamin D3 supplementation at 3000 IU (75 µg) demonstrated a significant increase in VO2 max compared to those provided with a placebo. Secondary aims were to determine whether supplementation influenced skeletal muscle and lung function.
Experimental methods
This 12-week parallel group, double-blind, randomised, placebo-controlled trial was conducted at the University of Ulster, Coleraine, at a latitude of 55°N between the months of November 2014 and April 2015. All procedures were approved by the University’s Research Ethics Committee (REC/14/0087), and the study was registered at www.clinicaltrials.gov (NCT02278172) and conducted in accordance with the Declaration of Helsinki. The protocol consisted of a series of appointments to obtain fasted blood samples and other physical measurements before and after a 12-week intervention. Nutritional and exercise intervention studies in athletes and healthy adults have demonstrated that 12 weeks is a suitable duration to observe a meaningful change over time in VO2 max [29–31]. Yet the dose and duration of vitamin D supplementation required to have a significant impact on VO2 max have not been investigated to date.
Subjects
Apparently healthy male and female athletes over the age of 18 were considered suitable for inclusion. Exclusion criteria were as follows: not a member of a university sports team; vitamin D supplementation and/or iron supplementation in the 30 days prior to baseline measurements; health concern(s)/physical disabilities identified by the screening questionnaire that would prevent successful completion of the study; consumption of medication(s) known to influence vitamin D metabolism; vegan athletes; sun-bed users; those who had been on a sun holiday in the 30 days prior to baseline measurements; those planning a sun holiday for during the time frame of the study. Gaelic footballers from the university team (n = 72) completed a screening questionnaire in the first instance. A total of 42 Gaelic footballers (n = 18 males and n = 24 females) were deemed eligible for inclusion and provided informed consent before commencing the study.
Supplements and compliance
An independent clinical trials manager used MINIM software [32] to randomise recruited athletes into vitamin D (VD) or placebo (PL) groups, stratified by sex and with an allocation ratio of 1:1. All subjects and researchers were blinded to the allocations until completion of the study and subsequent data analysis. Footballers allocated to the VD group received an oral spray solution providing 3000 IU(75 µg) vitamin D3 per spray, whereas those allocated to the PL group received an oral spray solution that did not contain vitamin D but was identical in appearance, smell, taste and from the same brand (BetterYou Ltd, Barnsley, UK). The dose provided was deemed suitable to raise total 25(OH)D concentrations to within the suggested range for extra-skeletal actions of vitamin D (75–100 nmol/L) [33–35]. The vitamin D3 content of supplements was verified by an independent laboratory using high-performance liquid chromatography (Eurofins Product Testing, Cheshire, UK). Footballers were instructed to administer a single spray, targeting the buccal membrane, on a daily basis throughout the intervention and to return their used spray bottle at their final appointment. Percentage compliance was determined by applying the following equations.
In Eqs. 1 and 2, D is number of days the spray was taken; f refers to the filled weight of the spray bottle, and b is the empty spray bottle weight. e is the weight of the spray bottle upon study completion with s referring to the weight of each spray. In Eq. 2, C is percentage compliance and d represents the number of days on intervention. Filled weights were based upon the manufacturer’s specifications and the average weight of a random sample of 10 oral spray bottles from the supplied batch.
Blood collection and processing
Participants were instructed to fast from 10 pm the night prior to blood sampling, and regular water intake was encouraged. Fasted blood samples were obtained from the antecubital fossa using a 21-gauge butterfly needle and 8 mL serum and 9 mL ethylenediaminetetraacetic acid (EDTA) plasma vacutainer tubes (Greiner Bio-One GmbH, Kremsmunster, Austria). Following inversion, serum samples were allowed to clot for <60 min and plasma samples placed in refrigeration until centrifugation. Tubes were centrifuged at 2200 rpm for 15 min at 4 °C to allow separation of whole blood into its respective components. Following separation, serum and plasma samples were pipetted into 0.5 mL aliquots and stored at −80 °C until further analysis.
Blood analyses
Liquid chromatography-tandem mass spectrometry (LCMS-MS) (API 4000; AB SCIEX) was used to quantify serum 25(OH)D2 and 25(OH)D3 concentrations, using a commercially available assay (Chromsystems Instruments and Chemicals GmbH; MassChrom 25-OH-Vitamin D3/D2). This analysis was undertaken at the Biochemistry Department of St James’ Hospital Dublin, a laboratory that complies with the Vitamin D External Quality Assessment Scheme and use of the National Institute of Standards and Technology 972 vitamin D standard reference material. The respective inter- and intra-assay coefficients of variation were 6.5 and 7.5 %. Plasma intact parathyroid hormone concentrations were measured, in duplicate, using a commercially available enzyme-linked immunosorbent assay (MD Biosciences Inc., Minnesota, USA). Intra and inter-assay coefficients of variation were 6.8 and 6.2 %, respectively. Calcium, albumin and creatinine concentrations were also measured in duplicate and assessed using an ILab 650 clinical biochemistry analyser (Instrumentation Laboratory, Massachusetts, USA). Intra-assay coefficients of variation were 0.65, 0.85 and 1.65 %, respectively. Intact parathyroid hormone and adjusted calcium concentrations were measured in order to ensure there were no adverse effects of the intervention such as hypoparathyroidism or hypercalcaemia [36]. Impaired renal function can lead to deleterious effects on vitamin D metabolism, and therefore, the renal function of athletes’ was evaluated by estimating glomerular filtration rate (eGFR) adjusted for fat-free mass [37, 38]. This was quantified from serum creatinine concentrations using the Modification of Diet in Renal Disease (MDRD) equation [39].
Skeletal muscle function
Average handgrip strength (kg) was measured using a dynamometer assembled at handgrip position 2 as default with shoulder flexion at 0º and elbow and wrist fully extended (Jamar Plus+, Patterson Medical, Warrenville, IL, USA) [40]. Footballers held the device alongside their body and gripped maximally a total of 3 times. Average handgrip strength was calculated for analysis. Vertical jump height (cm) was measured using a calibrated electronic jump mat (FSL Electronics Ltd, Cookstown, UK). Footballers performed a counter-movement jump a total of 3 times, with best recorded jump height used for statistical analysis [41]. A standardised rest period of 10 s was given between repeats of both handgrip and vertical jump tests.
Lung function
Footballers’ lung function was assessed using a calibrated MicroLab portable spirometer (Carefusion Corporation, San Diego, CA, USA). Forced vital capacity (FVC) and forced expiratory volume at 1 s (FEV1) were quantified by exhaling maximally into a 1-way disposable mouthpiece, and a minimum of 3 repeats was performed in order to derive average values.
Maximal oxygen consumption
Footballers refrained from heavy training/competition for at least 24 h prior to exercise testing, in order to control for last-bout effects. Pre- and post-intervention, subjects completed an incremental exercise test that was designed to elicit a VO2 max response within the capabilities of the treadmill (MERC-C, WOODWAY GmbH, Germany). Gas analysis was performed using a metabolic cart that has been shown to give reliable measurements (Metalyzer 3B, CORTEX Biophysik GmbH, Germany) with calibrations for ambient conditions, analyser volume and concentrations of oxygen and carbon dioxide performed on a daily basis, prior to testing [42]. Footballers wore an FT1 heart rate monitor (Polar Electro Ltd, Warwick, UK) and face mask with triple V insert. Following a standardised warm-up at 5 km/h (1 % incline), the test began at a running speed of 8 km/h (1 % incline) and speed increased by 1 km/h every minute until a running speed of 17 km/h was attained. At this point, running speed remained constant; however, incline increased by 1 % each minute until VO2 max was achieved. The test was terminated upon volitional exhaustion or if any two of the following criteria were met: respiratory exchange ratio >1.15; oxygen plateau observed (i.e. no increase in oxygen consumption despite an increase in workload); heart rate ±10 bpm of age-predicted maximum (208 − 0.7 × age) [43]. Achievement of VO2 max was further verified by determining post-exercise lactate concentrations, using a Lactate Pro device as per the manufacturers’ recommendations (Arkray Inc, Kyoto, Japan). Peak lactate concentrations are reached between 3 and 8 min post-exercise [44]; therefore, at 5 min, following cessation of the VO2 max test, a 6-µL capillary blood sample was obtained for lactate analysis. The lactate response to exercise may also vary according to age and sex. To account for this a blood lactate concentration >9 mmol/L in males and >7 mmol/L in females was considered as evidence of significant anaerobic metabolism [45].
Body composition
Footballers’ height and weight were measured using a stadiometer and calibrated scales. Fat mass (FM) and fat-free mass (FFM) were measured by whole-body densitometry pre- and post-intervention (BOD POD, Life Measurement Inc, Concord, CA). The validity of this method has been reported extensively elsewhere [46]. Footballers were asked to refrain from heavy physical activity for 24 h, and testing was performed following an overnight fast. Body mass was calculated using a calibrated electronic scale. Body volume was determined by air displacement plethysmography, corrected for predicted thoracic gas volume. The plethysmography chamber was calibrated using a 49.385-L cylinder as per manufacturers’ instructions. Percentage fat mass (%FM) was calculated using the Siri equation [47]. Footballers wore tight-fitting clothing (i.e. swimsuit or compression garment with silicone swimming cap), to ensure an accurate measurement of body volume, and were instructed to sit upright and remain still throughout the test. A minimum of two measurements was taken per athlete. FM and FFM (kg) were adjusted for athlete’s height (m2) and presented as fat mass index (FMI) and fat-free mass index (FFMI) (kg/m2) [48].
Dietary assessment
In order to estimate dietary vitamin D intake, footballers completed a validated food frequency questionnaire (FFQ) [49]. These data were collected on a single occasion due to the negligible contribution of dietary sources to total 25(OH)D concentration and the low intake of such foods in the Western diet [50, 51], despite a growing range of vitamin D-fortified products. Researchers asked players a series of questions relating to their consumption of food items known to contain vitamin D, with a photographic food atlas used to estimate portion sizes [52].
Physical activity
The validated Recent Physical Activity Questionnaire (RPAQ), capable of assessing physical activity for the previous 4 weeks, was completed pre- and post-intervention to control for a change in moderate-vigorous physical activity during the study [53]. Participants completed RPAQ questionnaires during appointments, and the researcher present queried any ambiguous responses prior to data entry.
Statistical analysis
An a priori power calculation with a two-sided 5 % significance level and power at 95 % determined that 35 athletes were required to observe a statistically significant 3.5 mL/kg/min increase in VO2 max (G Power version 3.1) [54]. The final number of recruited athletes (n = 42) took into account an estimated dropout rate of 20 %. All statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS) with significance set at P < 0.05 throughout (IBM SPSS Statistics for Windows, version 21.0, IBM Corp, Armonk, NY). In accordance with the Consolidated Standards of Reporting Trials (CONSORT) guidelines, analyses were conducted using the intention-to-treat (ITT) principle thereby including all athletes randomised at baseline (n = 42) [55]. Missing data for physical and biochemical measures were deemed to be missing completely at random, owing to injury or illness unrelated to the intervention, justifying the use of multiple imputation. The Shapiro–Wilk test was used to determine whether data followed a normal distribution and skewed variables were transformed, using the logarithmic function, to attain a normal distribution prior to multiple imputation and further analysis. Transformations were applied to total 25(OH)D, creatinine and PTH concentrations as well as age and change in moderate-vigorous physical activity and FFMI. Multiple imputations consisted of 40 imputed data sets with pooled data used for subsequent analysis [56]. Imputed data are outlined in Fig. 1. Descriptive statistics were used to present participant characteristics at baseline. An independent t test or a Chi-square test was utilised to test for differences between VD and PL groups at baseline. ANCOVA models were used to assess the effect of intervention on VO2 max and secondary outcome measures. Prognostic covariates were selected a priori for each model based upon evidence of a significant interaction between the covariate and dependent variable in question [57–60]. Reliability of repeated skeletal muscle function tests was assessed by pooling pre- and post-intervention data in order to determine the standard error of measurement (SEM) and intra-class correlation coefficient (ICC) [61]. These analyses were performed using the reliability test function in SPSS and SEM calculated by applying Cronbach’s α to following equation. \({\text{SEM}} = {\text{SD}}\sqrt {(1 {-} r_{xx}^{2} )}\) where SEM is standard error of measurement, SD refers to the standard deviation of test scores, and r xx refers to Cronbach’s α as the reliability measure of test scores [62].
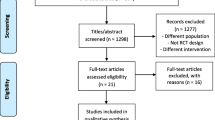
CONSORT flow diagram. A total of 72 Gaelic footballers were assessed for eligibility with 30 excluded due to not meeting the inclusion criteria (n = 7) or no longer wishing to participate (n = 23). Remaining Gaelic footballers (n = 42) were randomised to receive an oral spray solution containing either 3000 IU of vitamin D3 (n = 22) or placebo (n = 20). A total of 7 athletes were lost to follow-up owing to illness (n = 1) unrelated to the intervention, sun holiday (n = 1) or no longer wishing to participate (n = 5). A total of 35 athletes completed the study per protocol (vitamin D treatment group n = 18 and placebo n = 17). All footballers randomised at baseline were included in the final analysis (n = 42)
Results
A total of 7 footballers were absent to follow-up (n = 5 VD and n = 2 PL) due to sun holidays or illness unrelated to the intervention. Use of ITT did not change the outcome of the study when compared with per protocol analysis. There was no significant difference in the ratio of male to female subjects between groups (males n = 12 and females n = 10 VD; males n = 6 and females n = 14 PL) P = 0.857. The participant flow throughout the study is summarised in Fig. 1. Footballers’ biochemical and physical characteristics at baseline and week 12 are provided in Table 1. The average rate of compliance to the intervention was 95 %. At baseline, 50 and 22 % of athletes presented with vitamin D insufficiency (31–49 nmol/L) and deficiency (<30 nmol/L), respectively. The effect of the intervention on outcome measures at week 12, after adjusting for covariates, is detailed in Table 2. Supplementation significantly increased total 25(OH)D concentrations in the VD group compared to PL group, P = 0.006, and resolved vitamin D deficiency in all athletes allocated to VD. There was no correlation between total 25(OH)D and measures of physical performance at either time point, P > 0.05. Furthermore, supplementation with vitamin D3 did not significantly increase VO2 max compared to the PL group, P = 0.375. Vitamin D3 supplementation did not significantly increase vertical jump height when compared to the PL group, P = 0.797, and also had no significant effect on left or right handgrip strength, P = 0.146 and P = 0.266, respectively. SEM and ICC results for vertical jump height (SEM = 1.51, r = 0.95), left and right handgrip strength (SEM = 2.06, r = 0.96 and SEM = 2.34, r = 0.95, respectively) indicated a strong internal consistency across repeated skeletal muscle function tests. Supplementation with vitamin D3 did not have a significant effect upon either measure of footballers lung function compared to those allocated to PL, FVC P = 0.573 and FEV1 P = 0.665. There were no adverse health effects to supplementation demonstrated by normal adjusted calcium and PTH concentrations at week 12.
Discussion
This is not only the largest investigation of vitamin D supplementation on VO2 max in athletes to date but also the first randomised controlled trial to successfully optimise vitamin D status using an oral spray solution. In this study, over half of the total cohort presented with vitamin D insufficiency or deficiency at baseline (50 and 22 %, respectively). Such findings corroborate existing literature [3, 5], reiterating that athletes are a population that may be at risk of poor bone health, owing to total 25(OH)D concentrations below 50 nmol/L [63, 64]. Our previous research identified this health concern in elite Gaelic footballers, a finding now corroborated in those competing at the collegiate level [3]. Twelve-week vitamin D3 supplementation using a 3000 IU (75 µg) oral spray solution resolved vitamin D deficiency and increased mean total serum 25(OH)D concentrations to over 80 nmol/L. Conversely, those allocated to the PL treatment group remained at potential risk of poor bone health with a mean total 25(OH)D concentration below 50 nmol/L at week twelve [65]. In contrast, Storlie et al. [66] reported no significant change in total 25(OH)D concentrations over 12 weeks in athletes supplemented daily with a 1000 IU (25 µg) vitamin D3 oral spray compared to placebo, supporting 3000 IU (75 µg) as an effective wintertime dosage. There is ongoing debate over what constitutes an optimal total 25(OH)D concentration for athletes. Some speculate that higher total 25(OH)D concentrations in excess of 100 nmol/L may be necessary to trigger the purported extra-skeletal benefits of vitamin D in athletes [67, 68], though there is currently a lack of strong evidence for a benefit of maintaining total 25(OH)D concentrations above this threshold [35]. Furthermore, toxicity manifests itself as hypercalcaemia and increased bone resorption at vitamin D supplementation doses exceeding 10,000 IU/day (250 µg) or a total 25(OH)D concentration ≈750 nmol/L [69]. Indeed, there was a significant change in FMI over the 12-week intervention period. FMI increased in the VD group but declined in the PL group. Although in-season, this finding may be explained by differences in the footballers’ individual training and conditioning programmes during the winter months in the absence of scheduled training sessions at the university.
Mechanistic studies support the concept that vitamin D may influence VO2 max through direct and indirect actions on iron metabolism [24, 25]. Nevertheless, studies investigating the potential link between total 25(OH)D concentration and VO2 max in vivo have yielded equivocal findings to date with many failing to account for important covariates such as PTH concentrations and participation in moderate-vigorous physical activity [13, 15, 70–75]. Moreover, universal criteria for VO2 max have not been firmly established and therefore this may contribute to variation in study outcomes. Total 25(OH)D concentration was not associated with VO2 max at either time point in the current study, a finding that is supported by Fitzgerald et al. 2014 and research conducted in healthy adults [14, 16]. In contrast, at a latitude of 35°N, Koundourakis and colleagues reported positive bivariate correlations between total 25(OH)D concentration and the VO2 max of elite footballers, before and after a tapering period spanning the months of June and July [17]. During this time, there was a small yet significant decrease in athlete’s VO2 max despite a concomitant increase in total 25(OH)D concentrations, likely owing to a reduced training load. Such findings indicate that vitamin D does not play a supportive role in determining VO2 max in athletes, a concept that is substantiated by findings of the current study. Supplementation did not significantly increase VO2 max compared to the PL group despite increasing total 25(OH)D concentration by 77 %, a finding that has also been shown by others [76]. This contrasts with some randomised controlled trials of patients with cardiorespiratory pathology, although findings have not been consistent [77, 78]. Established primary determinants of VO2 max include cardiac output and oxygen diffusion capacity [21], and a possible explanation for the disparity between athletes and patients may be that athletes have a smaller ability to improve VO2 max, owing to significant cardiovascular adaptations to aerobic training including enhanced cardiac output and capillary density [79]. It is plausible that such adaptations may outweigh any potential benefit of vitamin D supplementation on VO2 max when compared to patients with diminished cardiac output and/or oxygen diffusion capacity.
The in vitro mechanisms by which vitamin D, specifically 1,25(OH)2D, may impact upon the skeletal muscle function of athletes have been reviewed extensively elsewhere, although less is known about the effects of vitamin D supplementation on skeletal muscle function in vivo [7, 80]. Indeed, the effects of vitamin D supplementation on skeletal muscle function in athletes have been investigated before, albeit without taking into account change in physical activity or body composition, confounders that determine skeletal muscle function and may therefore mask a null effect of treatment [81, 82]. Total 25(OH)D concentration was not associated with any measure of skeletal muscle function in the current study, and supplementation did not significantly increase vertical jump height or handgrip strength when compared to PL, corroborating findings from a recent randomised controlled trial conducted in adolescent swimmers [83]. These results demonstrate that vitamin D3 supplementation does not enhance skeletal muscle function in younger adults after taking into account change in FMI, FFMI and moderate-vigorous physical activity, despite increasing total 25(OH)D concentrations to over 80 nmol/L. This contrasts with large studies of elderly patients that have identified a beneficial effect of vitamin D and calcium supplementation on skeletal muscle function and risk of falls [84–86]. Aside from differences in the supplementation regime it is possible to speculate, based on the results of the current study and existing literature, that vitamin D3 supplementation only benefits skeletal muscle in those with diminished function, explaining why no ergogenic effect was observed in this cohort of trained footballers. Another consideration is that the time taken for supplementation to increase total 25(OH)D concentrations to over 50 nmol/L, within the 12-week intervention, is not known. Therefore, it is possible that supplementation only increased total 25(OH)D concentrations to above 50 nmol/L late in the intervention, leaving little time for a measurable effect on skeletal muscle function parameters.
Emerging research also posits that total 25(OH)D concentrations may be related to lung function, especially in those with airway disease [87–89]. Potential mechanisms include enhanced innate immunity and downregulation of the T helper 1 cell response, resulting in less airway inflammation and a consequent improvement in overall airway function [90]. Nevertheless, this study did not observe an association between total 25(OH)D concentration and measures of lung function at either time point and, in adjusted analyses, supplementation with vitamin D3 did not significantly impact upon FEV1 or FVC when compared to PL. In unadjusted analyses, there was a significant decrease in FVC over time in the VD group compared to those allocated to PL yet this was not the case in adjusted analyses indicating that the intervention did not have an adverse effect. These findings suggest that the response to vitamin D3 supplementation, in terms of benefits on lung function parameters, may differ between healthy individuals and those with airway disease although larger studies, adjusting for lung function specific confounders are required.
To our knowledge this is the first study to investigate the effects of vitamin D3 supplementation on VO2 max in athletes that has adjusted for key component covariates. Strengths of the study include a gender balance of athletes, accurate recording of compliance, independently verifying the vitamin D3 content of supplements and being adequately powered to detect any potential significant change in VO2 max. Due to the heterogeneous athlete population it is not known whether our findings translate to non-Caucasian athletes or those from endurance or strength-based disciplines. The VO2 max test used in the current study was not validated. Future studies in this area are encouraged to utilise a validated protocol. The sample size for this study was specific to the primary outcome measure, VO2 max. Further research with larger sample sizes may therefore be required in order to categorically rule out a beneficial effect of vitamin D supplementation on skeletal muscle and lung function in athletes. Future studies may also wish to consider stratifying by weight as well as sex to prevent differences between treatment groups at baseline.
In conclusion, this study observed a high prevalence of vitamin D insufficiency and deficiency in collegiate Gaelic footballers during wintertime and such individuals should consider vitamin D supplementation to avoid being at risk of poor bone health. Twelve-week daily supplementation with a 3000 IU (75 µg) vitamin D3 oral spray solution is an appropriate method, dose and duration to resolve deficiency and increase total 25(OH)D concentrations to over 80 nmol/L. However, vitamin D supplementation, at the dose provided here for 12 weeks, did not have any beneficial effect on VO2 max, skeletal muscle or lung function in this cohort of Gaelic footballers.
References
IOM (Institute of Medicine) (2011) Dietary reference intakes for calcium and vitamin D. The National Academies Press, Washington
Holick M, Chen T (2008) Vitamin D deficiency: a worldwide problem with health consequences. Am J Clin Nutr 87(4):1080S–1086S
Magee PJ, Pourshahidi LK, Wallace JMW, Cleary J, Conway J, Harney E et al (2013) Vitamin D status and supplementation in elite Irish athletes. Int J Sport Nutr Exerc Metab 23(5):441–448
Villacis D, Yi A, Jahn R, Kephart C, Charlton T, Gamradt S et al (2014) Prevalence of abnormal vitamin D levels among division I NCAA athletes. Sports Health 6(4):640–647
Farrokhyar F, Tabasinejad R, Dao D, Peterson D, Ayeni O, Hadioonzadeh R et al (2015) Prevalence of vitamin D inadequacy in athletes: a systematic-review and meta-analysis. Sports Med 45(3):365–378
Christodoulou S, Goula T, Ververidis A, Drosos G (2013) Vitamin D and bone disease. Biomed Res Int 396541:1–6
Todd JJ, Pourshahidi LK, McSorley EM, Madigan SM, Magee PJ (2015) Vitamin D: recent advances and implications for athletes. Sports Med 45(2):213–219
Webb AR (2006) Who, what, where and when-influences on cutaneous vitamin D synthesis. Prog Biophys Mol Biol 92(1):17–25
Stephensen CB, Zerofsky M, Burnett DJ, Lin YP, Hammock BD, Hall LM et al (2012) Ergocalciferol from mushrooms or supplements consumed with a standard meal increases 25-hydroxyergocalciferol but decreases 25-hydroxycholecalciferol in the serum of healthy adults. J Nutr 142(7):1246–1252
Chen TC, Chimeh F, Lu Z, Mathieu J, Person KS, Zhang A et al (2007) Factors that influence the cutaneous synthesis and dietary sources of vitamin D. Arch Biochem Biophys 460(2):213–217
Aranow C (2011) Vitamin D and the immune system. J Invest Med 59(6):881–886
Haussler M, Haussler C, Jurutka P, Thompson P, Hsieh J, Remus L et al (1997) The vitamin D hormone and its nuclear receptor: molecular actions and disease states. J Endocrinol 154:S57–S73
Farrell S, Cleaver J, Willis B (2011) Cardiorespiratory fitness, adiposity, and serum 25-dihydroxyvitamin D levels in men. Med Sci Sports Exerc 43(2):266–271
Fitzgerald J, Peterson B, Warpeha J, Wilson P, Rhodes G, Ingraham S (2014) Vitamin D status and V[combining dot above]O2peak during a skate treadmill graded exercise test in competitive ice hockey players. J Strength Cond Res 28(11):3200–3205
Forney LA, Earnest CP, Henagan TM, Johnson LE, Castleberry TJ, Stewart LK (2014) Vitamin D status, body composition, and fitness measures in college-aged students. J Strength Cond Res 28(3):814–824
Gregory SM, Parker BA, Capizzi JA, Grimaldi AS, Clarkson PM, Moeckel-Cole S et al (2013) Changes in vitamin D are not associated with changes in cardiorespiratory fitness. Clin Med Res 2(4):68–72
Koundourakis N, Androulakis N, Malliaraki N, Margioris A (2014) Vitamin D and exercise performance in professional soccer players. PLoS One 1(7):e101659
Fitzgerald JS, Peterson BJ, Warpeha JM, Johnson SC, Ingraham SJ (2015) Association between Vitamin D Status and maximal-intensity exercise performance in junior and collegiate hockey players. J Strength Cond Res 29(9):13–21
Dahlquist DT, Dieter BP, Koehle MS (2015) Plausible ergogenic effects of vitamin D on athletic performance and recovery. J Int Soc Sports Nutr 12(33):1–12
Helgerud J, Engen L, Wisloff U, Hoff J (2001) Aerobic endurance training improves soccer performance. Med Sci Sports Exerc 33(11):1925–1931
Bassett D, Howley E (2000) Limiting factors for maximum oxygen uptake and determinants of endurance performance. Med Sci Sports Exerc 31(1):70–84
Autier P, Boniol M, Pizot C, Mullie P (2014) Vitamin D status and ill health: a systematic review. Lancet Diabetes Endocrinol 2(1):76–89
Toxqui L, Pérez-Granados AM, Blanco-Rojo R, Wright I, González-Vizcayno C, Vaquero MP (2013) Effects of an iron or iron and vitamin D-fortified flavored skim milk on iron metabolism: a randomized controlled double-blind trial in iron-deficient women. J Am Coll Nutr 32(5):312–320
Bacchetta J, Zaritsky JJ, Sea JL, Chun RF, Lisse TS, Zavala K et al (2014) Suppression of iron-regulatory hepcidin by vitamin D. J Am Soc Nephrol 25(3):564–572
Zughaier SM, Alvarez JA, Sloan JH, Konrad RJ, Tangpricha V (2014) The role of vitamin D in regulating the iron-hepcidin-ferroportin axis in monocytes. J Clin Transl Endocrinol 1(1):19–25
Nemeth E, Ganz T (2006) Regulation of iron metabolism by hepcidin. Annu Rev Nutr 26:323–342
Ganz T, Nemeth E (2012) Hepcidin and iron homeostasis. Biochim Biophys Acta 1823(9):1434–1443
Rossi E (2005) Hepcidin: the iron regulatory hormone. Clin Biochem Rev 26(3):47–49
Ghiasvand R, Askari G, Malekzadeh J, Hajishafiee M, Daneshvar P, Akbari F et al (2012) Effects of six weeks of β-alanine administration on VO2 max, time to exhaustion and lactate concentrations in physical education students. Int J Prev Med 3(8):559–563
Durkalec-Michalski K, Jeszka J (2015) The efficacy of a β-hydroxy-β-methylbutyrate supplementation on physical capacity, body composition and biochemical markers in elite rowers: a randomised, double-blind, placebo-controlled crossover study. J Int Soc Sports Nutr 12:31
Wolpern AE, Burgos DJ, Janot JM, Dalleck LC (2015) Is a threshold-based model a superior method to the relative percent concept for establishing individual exercise intensity? a randomized controlled trial. BMC Sports Sci Med Rehabil 7(16):1–9
Minim: Allocation by minimisation in clinical trials [homepage on the Internet]. 14th Mar 2013. Available from: https://www-users.york.ac.uk/~mb55/guide/minim.htm
Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP et al (2011) Evaluation, treatment, and prevention of vitamin D deficiency: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 96(7):1911–1930
Cannell JJ, Hollis BW, Zasloff M, Heaney RP (2008) Diagnosis and treatment of vitamin D deficiency. Expert Opin Pharmacother 9(1):107–118
Bischoff-Ferrari HA, Giovannucci E, Willett WC, Dietrich T, Dawson-Hughes B (2006) Estimation of optimal serum concentrations of 25-hydroxyvitamin D for multiple health outcomes. Am J Clin Nutr 84(1):18–28
Lips P (2006) Vitamin D physiology. Prog Biophys Mol Biol 92(1):4–8
McNeely MDD (2005) The estimated glomerular filtration rate: linchpin of the chronic kidney disease guidelines. BCM J 2005(47):287–291
Al-Badr W, Martin KJ (2008) Vitamin D and kidney disease. CJASN 3(5):1555–1560
Stevens LA, Coresh J, Feldman HI, Greene T, Lash JP, Nelson RG et al (2007) Evaluation of the modification of diet in renal disease study equation in a large diverse population. J Am Soc Nephrol 18(10):2749–2757
Trampisch US, Franke J, Jedamzik N, Hinrichs T, Platen P (2012) Optimal Jamar dynamometer handle position to assess maximal isometric hand grip strength in epidemiological studies. J Hand Surg 37(11):2368–2373
Linthorne N (2001) Analysis of standing vertical jumps using a force platform. Am J Phys 69(11):1198–1204
Meyer T, Georg T, Becker C, Kindermann W (2001) Reliability of gas exchange measurements from two different spiroergometry systems. Int J Sports Med 22(8):593–597
Tanaka H, Monahan KD, Seals DR (2001) Age-predicted maximal heart rate revisited. J Am Coll Cardiol 37(1):153–156
Goodwin M, Harris J, Hernández A, Gladden L (2007) Blood lactate measurements and analysis during exercise: a guide for clinicians. J Diabetes Sci Technol 1(4):558–569
Edvardsen E, Hem E, Anderssen SA (2014) End criteria for reaching maximal oxygen uptake must be strict and adjusted to sex and age: a cross-sectional study. PLoS One 9(1):e85276
Fields DA, Goran MI, McCrory MA (2002) Body-composition assessment via air-displacement plethysmography in adults and children: a review. Am J Clin Nutr 75(3):453–467
Siri W (1961) Body composition from fluid spaces and density: analysis of methods. In: Brozek J, Henschel A (eds) Techniques for measuring body composition. National Academy of Sciences, Washington, pp 223–244
Cole TJ, Fewtrell MS, Prentice A (2008) The fallacy of using percentage body fat as a measure of adiposity. Am J Clin Nutr 87(6):1959–1960
Weir RR, Carson EL, Mulhern MS, Laird E, Healy M, Pourshahidi LK (2015) Validation of a food frequency questionnaire to determine vitamin D intakes using the method of triads. J Hum Nutr Diet 29(2):255–261
Spiro A, Buttriss J (2014) Vitamin D: an overview of vitamin D status and intake in Europe. Nutr Bull 39(4):322–350
Calvo MS, Whiting SJ, Barton CN (2005) Vitamin D intake: a global perspective of current status. J Nutr 135:310–316
Nelson M, Atkinson M, Meyer J (1997) A photographic atlas of food portion sizes. MAFF Publications, London
Besson H, Brage S, Jakes R, Ekelund U, Wareham N (2010) Estimating physical activity energy expenditure, sedentary time, and physical activity intensity by self-report in adults. Am J Clin Nutr 91(1):106–114
Cregg CJ, Kelly D, O’Connor PL, Daly P, Moyna NM (2013) In: Effects of high intensity interval training and high volume endurance training on maximal aerobic capacity, speed and power in club-level Gaelic football players. May 28–June 1; Indianapolis, Indiana. American College of Sports Medicine 60th annual meeting and 4th world congress on exercise is medicine
Moher D, Hopewell S, Schulz KF, Montori V, Gøtzsche PC, Devereaux PJ et al (2010) CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. BMJ 340:C869
Graham JW, Olchowski AE (2007) Gilreath TD (2007) How many imputations are really needed? some practical clarifications of multiple imputation theory. Prev Sci 8:206–213
Kahan B, Jairath V, Doré C, Morris T (2014) The risks and rewards of covariate adjustment in randomized trials: an assessment of 12 outcomes from 8 studies. Trials 15:139
Goran M, Fields DA, Hunter GR, Herd SL, Weinsier RL (2000) Total body fat does not influence maximal aerobic capacity. Int J Obes Relat Metab Disord 24(7):841–848
Jones RL, Nzekwu MM (2006) The effects of body mass index on lung volumes. Chest 130(3):827–833
Gormley SE, Swain DP, High R, Spina RJ, Dowling EA, Kotipalli US et al (2008) Effect of intensity of aerobic training on VO2 max. Med Sci Sports Exerc 40(7):1336–1343
Bruton A, Conway JH, Holgate ST (2000) Reliability: what is it, and how is it measured? Physiotherapy 86(2):94–99
Tighe J, McManus IC, Dewhurst NG, Chis L, Mucklow J (2010) The standard error of measurement is a more appropriate measure of quality for postgraduate medical assessments than is reliability: an analysis of MRCP(UK) examinations. BMC Med Educ 10(40):1–9
Laird E, Ward M, McSorley E, Strain JJ, Wallace J (2010) Vitamin D and bone health: potential mechanisms. Nutrients 2(7):693–724
Holick MF (2004) Sunlight and vitamin D for bone health and prevention of autoimmune diseases, cancers, and cardiovascular disease. Am J Clin Nutr 80(6S):1678–1688
Thacher TD, Clarke BL (2011) Vitamin D insufficiency. Mayo Clin Proc 86(1):50–60
Storlie DM, Pritchett K, Pritchett R, Cashman C (2011) 12-week vitamin D supplementation trial does not significantly influence seasonal 25(OH)D status in male collegiate athletes. Int J Health Nutr 2(2):8–13
Close GL, Fraser WD (2012) Vitamin D supplementation for athletes: too much of a good thing? Sport Exerc Sci 33:24–25
Heaney RP (2011) Assessing vitamin D status. Curr Opin Clin Nutr Metab Care 14(5):440–444
Jones G (2008) Pharmacokinetics of vitamin D toxicity. Am J Clin Nutr 88(2):582S–586S
Silverberg SJ (2007) Vitamin D deficiency and primary hyperparathyroidism. J Bone Miner Res 22(S2):100–104
Aadahl M, Kjaer M, Kristensen JH, Mollerup B, Jørgensen T (2007) Self-reported physical activity compared with maximal oxygen uptake in adults. Eur J Cardiovasc Prev Rehabil 14(3):422–428
Farrell SW, Willis BL, Willis B (2012) Cardiorespiratory fitness, adiposity, and serum 25-dihydroxyvitamin D levels in women: the cooper center longitudinal study. J Womens Health (Larchmt) 21(1):80–86
Mowry DA, Costello MM, Heelan KA (2009) Association among cardiorespiratory fitness, body fat, and bone marker measurements in healthy young females. J Am Osteopath Assoc 109(10):534–539
Valtueña J, Gracia-Marco L, Huybrechts I, Breidenassel C, Ferrari M, Gottrand F et al (2013) Cardiorespiratory fitness in males, and upper limbs muscular strength in females, are positively related with 25-hydroxyvitamin D plasma concentrations in European adolescents: the HELENA study. QJM 106(9):809–821
Jastrzębski Z (2015) Effect of vitamin D supplementation on the level of physical fitness and blood parameters of rowers during the 8-week high intensity training. Facicula Educaţie Fizică şi Sport 2:57–67
Scholten SD, Sergeev IN, Song Q, Birger CB (2015) Effects of vitamin D and quercetin, alone and in combination, on cardiorespiratory fitness and muscle function in physically active male adults. Open Access J Sports Med 24(6):229–239
Boxer RS, Kenny AM, Schmotzer BJ, Vest M, Fiutem JJ, Piña IL (2013) A randomized controlled trial of high dose vitamin D3 in patients with heart failure. JACC Heart Fail 1(1):84–90
Hornikx M, Van Remoortel H, Lehouck A, Mathieu C, Maes K, Gayan-Ramirez G, et al (2012) Vitamin D supplementation during rehabilitation in COPD: a secondary analysis of a randomized trial. Respir Res 13(84):1–9
Blomqvist CG, Saltin B (1983) Cardiovascular adaptations to physical training. Annu Rev Physiol 45:169–189
Girgis CM, Clifton-Bligh RJ, Hamrick MW, Holick MF, Gunton JE (2013) The roles of vitamin D in skeletal muscle: form, function, and metabolism. Endocr Rev 34(1):33–83
Close GL, Leckey J, Patterson M, Bradley W, Owens DJ, Fraser WD et al (2013) The effects of vitamin D(3) supplementation on serum total 25[OH]D concentration and physical performance: a randomised dose-response study. Br J Sports Med 47(11):692–696
Close GL, Russell J, Cobley JN, Owens DJ, Wilson G, Gregson W et al (2013) Assessment of vitamin D concentration in non-supplemented professional athletes and healthy adults during the winter months in the UK: implications for skeletal muscle function. J Sports Sci 31(4):344–353
Dubnov-Raz G, Livne N, Raz R, Cohen AH, Constantini NW (2015) Vitamin D Supplementation and physical performance in adolescent swimmers. Int J Sport Nutr Exerc Metab 25(4):317–325
Bischoff HA, Stähelin HB, Dick W, Akos R, Knecht M, Salis C et al (2003) Effects of vitamin D and calcium supplementation on falls: a randomized controlled trial. J Bone Miner Res 18(2):343–351
Pfeifer M, Begerow B, Minne HW, Suppan K, Fahrleitner-Pammer A, Dobnig H (2009) Effects of a long-term vitamin D and calcium supplementation on falls and parameters of muscle function in community-dwelling older individuals. Osteoporos Int 20(2):315–322
Houston DK, Tooze JA, Demons JL, Davis BL, Shertzer-Skinner R, Kearsley LB, et al (2015) Delivery of a Vitamin D intervention in homebound older adults using a meals-on-wheels program: a pilot study. J Am Geriatr Soc 63(9):1861–1867
Black PN, Scragg R (2005) Relationship between serum 25-hydroxyvitamin D and pulmonary function in the third national health and nutrition examination survey. Chest 128(6):3792–3798
Li F, Peng M, Jiang L, Sun Q, Zhang K, Lian F et al (2011) Vitamin D deficiency is associated with decreased lung function in Chinese adults with asthma. Respiration 81(6):469–475
Jung JY, Kim YS, Kim SK, Kim HY, Oh YM, Lee SM et al (2015) Relationship of vitamin D status with lung function and exercise capacity in COPD. Respirology 20(5):782–789
Hughes DA, Norton R (2009) Vitamin D and respiratory health. Clin Exp Immunol 158(1):20–25
Acknowledgments
The authors would like to thank the Department for Employment and Learning for supporting this research and BetterYou Ltd for gifting the oral spray solutions. The authors would like to thank Aaron Ballantyne and Dr Julie Sittlington for their advice and support with VO2 max testing and all athletes involved in the study. PM was the principle investigator. JT, EMcS, LKP, PM and SM conceived of the study design. JT was responsible for data collection and performed statistical analysis. MH and EL were responsible for vitamin D analyses. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no financial or personal conflicts of interest to declare in relation to this article.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Todd, J.J., McSorley, E.M., Pourshahidi, L.K. et al. Vitamin D3 supplementation using an oral spray solution resolves deficiency but has no effect on VO2 max in Gaelic footballers: results from a randomised, double-blind, placebo-controlled trial. Eur J Nutr 56, 1577–1587 (2017). https://doi.org/10.1007/s00394-016-1202-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-016-1202-4