Abstract
Purpose
Higher long-chain polyunsaturated fatty acids (LCP) in infant compared with maternal lipids at delivery is named biomagnification. The decline of infant and maternal docosahexaenoic acid (DHA) status during lactation in Western countries suggests maternal depletion. We investigated whether biomagnification persists at lifelong high fish intakes and whether the latter prevents a postpartum decline of infant and/or maternal DHA status.
Methods
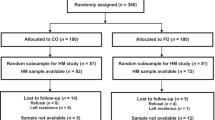
We studied 3 Tanzanian tribes with low (Maasai: 0/week), intermediate (Pare: 2–3/week), and high (Sengerema: 4–5/week) fish intakes. DHA and arachidonic acid (AA) were determined in maternal (m) and infant (i) erythrocytes (RBC) during pregnancy (1st trimester n = 14, 2nd = 103, 3rd = 88), and in mother–infant pairs at delivery (n = 63) and at 3 months postpartum (n = 104).
Results
At delivery, infants of all tribes had similar iRBC-AA which was higher than, and unrelated to, mRBC-AA. Transplacental DHA biomagnification occurred up to 5.6 g% mRBC-DHA; higher mRBC-DHA was associated with “bioattenuation” (i.e., iRBC-DHA < mRBC-DHA). Compared to delivery, mRBC-AA after 3 months was higher, while iRBC-AA was lower. mRBC-DHA after 3 months was lower, while iRBC-DHA was lower (low fish intake), equal (intermediate fish intake), and higher (high fish intake) compared to delivery. We estimated that postpartum iRBC-DHA equilibrium is reached at 5.9 g%, which corresponds to a mRBC-DHA of 6.1 g% throughout pregnancy.
Conclusion
Uniform high iRBC-AA at delivery might indicate the importance of intrauterine infant AA status. Biomagnification reflects low maternal DHA status, and bioattenuation may prevent intrauterine competition of DHA with AA. A mRBC-DHA of about 6 g% during pregnancy predicts maternal–fetal equilibrium at delivery, postnatal iRBC-DHA equilibrium, but is unable to prevent a postnatal mRBC-DHA decline.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The long-chain polyunsaturated fatty acids (LC-PUFA) docosahexaenoic (DHA), eicosapentaenoic (EPA), and arachidonic (AA) acids are structural components of membrane phospholipids [1]. DHA and AA are notably abundant in the central nervous system and play important roles in fetal and infant neurodevelopment [2]. DHA, EPA, and AA are derived either from the diet or from endogenous synthesis from their respective parent essential fatty acids (EFA), linoleic (LA), and alpha-linolenic (ALA) acids. Fatty fish are rich sources of EPA and DHA. Dietary sources of preformed AA are meat, eggs, and poultry [3], while lean and tropical fish are rich sources of AA [4]. It is suggested that LC-PUFA intakes from our Paleolithic diet have been much higher [5–7] than presently observed in the majority of affluent countries [8, 9]. The high AA and DHA contents of our Paleolithic diet may imply that human evolution, and thus also intrauterine development, took place at high maternal intakes of both AA and DHA [5].
Pregnant and lactating women have high LC-PUFA needs [10]. This is notably the case for DHA that becomes synthesized from ALA with difficulty [11]. Both AA and DHA are important during infant development. More AA than DHA accretes in brain in the early intrauterine period, while DHA accretes rapidly from week 30 of pregnancy to 2 years postpartum [12]. The commonly observed higher LC-PUFA in circulating cord plasma lipids as compared to maternal plasma lipids has been coined “biomagnification” [13]. The declines of infant DHA status during lactation and of the maternal DHA status during pregnancy [14] and lactation [15] reflect the low LCPω3 status in many Western countries.
The outcomes of randomized controlled trials aiming at the improvement of neurodevelopment by the supplementation of pregnant women or their infants with fish oil, DHA [16–18], or DHA + AA [19] indicate subtle positive effects at most. This contrasts with the positive relationships between neonatal brain DHA and cognitive and behavioral performance that are noted in the combined human and animal studies [20–22]. Failure to show favorable effects of LC-PUFA might, among many other reasons, relate to the use of too low dosages and the study of Western populations with low fish intakes without stratification based on baseline DHA status [23].
There is substantial evidence that land–water ecosystems have been exploited by our early African ancestors [5, 24, 25], and it is also known that some rural African populations have much higher milk LC-PUFA contents [4, 26] as compared to those living in Western countries. Data on the concurrent maternal and infant LC-PUFA status during pregnancy and lactation in these African populations, however, are currently lacking. In view of this lack of data, we determined the maternal and infant DHA and AA status in 3 traditional rural African populations with different levels of fish intakes. Since a longitudinal study design proved impossible in these populations, we collected data deriving from different women during pregnancy, at delivery and at 3 months postpartum. The selected populations live in Tanzania and have low (Maasai), intermediate (Pare), or high (Sengerema) intakes of freshwater fish. All 3 populations are characterized by the consumption of diets that are constrained in their varieties by the availability of the food in their immediate environment. Red blood cell (RBC) LC-PUFA contents served as proxies for LC-PUFA status [27]. We were particularly interested to see whether “biomagnification” and maternal DHA losses during pregnancy and lactation also occur at lifetime high intakes of fish and at what maternal LC-PUFA status the infant reaches a state of postnatal LC-PUFA equilibrium.
Subjects and methods
Subjects, diet, and cultural circumstances
We selected 3 Tanzanian ethnic tribes with different intakes of local freshwater fish, i.e., the Maasai (no or low fish intake, 0/week), subjects from the Pare Mountains (intermediate fish intake, 2–3/weeks), and subjects from Sengerema (high fish intake, 4–5/weeks). We [4] have previously shown that East African freshwater fish contain high proportions of both DHA and AA and relatively low EPA as compared to European saltwater fish. We experienced that collection of longitudinal data was virtually impossible. Patients’ appointments in the hospital were not scheduled nor were we able to motivate subjects to participate in a longitudinal study.
The selected Maasai were Nilotic pastoralists who live in “bomas” (villages) in the Maasai Steppe nearby Ruvu. Their diet consists mainly of curdled milk and meat. It has recently become replenished with some ugali (corn porridge). Consumption of fish is uncommon, since it is considered inedible. The Pare group was composed of women of the Bantu tribes Pare and Sambaa from the Pare Mountains. Their diet was mainly composed of vegetables, beans, and fruits with ample ugali, rice and chapati (cornwheat pancakes), and some meat or fish. The third population was composed of women from Sengerema (southern shore of Lake Victoria). Apart from the abundant consumption of fish, they also consume ugali, muhogo (cassava root), and plantain (baked banana).
The ethnicity/tribe of each of the study groups was considered to be homogeneous. Most women were of low socioeconomical background. Their incomes were derived from pastoralism (Maasai), agriculture (Pare), or fisheries (Sengerema). The studied populations neither had possibilities nor interest in changing their cultural habits, including their diets. Local hospital staff members and interviews with the participants confirmed that neither pregnancy nor lactation is associated with any change in dietary habits or the prohibition of certain foods (F. Peters, R. S. Kuipers, F. A. J. Muskiet, unpublished data). Their dietary compositions were therefore likely to be representative for the lifetime dietary habits of each of the ethnical groups.
Women were included if they were apparently healthy and well nourished and had delivered an apparently healthy child at term (37–42 weeks, by estimate). Use of tobacco and alcohol is almost nonexistent in these populations, especially among women. Anthropometric data and a questionnaire on fish intake were obtained from the medical records or by interviews in Kiswahili. Besides the measurement of fundal heights, reliable data on gestational age were not always available, since some women had no recollection of their last menstrual period. Devices for echo imaging were either not available or not operational. All women gave their informed consent. The study was approved by the National Institute for Medical Research in Dar-es-Salaam (NIMR/HQIR.8a/Vol. IX/145, dated June 16, 2003 and NIMR/HQ/R.8a/Vol. IX/800, dated April 8, 2009) and was in agreement with the Declaration of Helsinki 1975 as revised in 2000.
Samples and analyses
We collected about 4 mL EDTA-anticoagulated venous blood of the mothers during pregnancy and at delivery and about 4 mL EDTA-cord blood at delivery (BD Vacutainer, Plymouth, UK). At 3 months postpartum, about 4 mL EDTA-anticoagulated venous blood of the mothers was collected. About 250 μL EDTA-anticoagulated blood (250 μL pediatric MiniCollect K3EDTA-tubes; Greiner Bio-one, Kremsmünster, Austria) was taken by heel prick from the 3-months-old infants. The samples were stored at 4 °C in the dark and processed within 2 h after collection. RBC were isolated by centrifugation and washed three times with 0.9% NaCl. After washing, 200 μL of the RBC suspension (mothers) or the entire RBC suspension (infants) was transferred to a Teflon-sealable Sovirel tube containing 2 mL of methanol-6 mol/L HCl (5:1 v/v), 1 mg butylated hydroxytoluene (antioxidant), and 50 μg 17:0. All samples were transported at ambient temperature to the University Medical Center Groningen (The Netherlands) for fatty acid analysis. Within 9 months after collection, the methanol–HCl conserved samples were transmethylated by heating at 90 °C for 4 h. Subsequent analysis of fatty acid methyl esters was performed, by capillary gas chromatography/flame ionization detection according to previously described procedures [28]. Fatty acid compositions were expressed in g% (g/100g).
Statistics
Statistical analyses were performed with SPSS version 16.0 (SPSS Inc, Chicago, IL). Within-tribe differences of mothers and infants at delivery were compared with corresponding data at 3 months postpartum by use of the Mann–Whitney U test. Mother–infant pair differences were tested with a Wilcoxon two-related samples test. In both instances, p < 0.05 was considered significant. Between-group differences were studied with the aid of the Kruskal–Wallis test, followed by the analyses with Mann–Whitney U test (nonparametric) at p < 0.05. Corrections were made for type-1 errors (Bonferroni correction). Equations were derived from linear regression analysis. We used the coefficient of determination (R 2) to estimate the extent to which a given variable was explained by another.
Results
Study groups
Pregnant women
We included 205 different pregnant women. Of these, 14 women were included in their 1st trimester of pregnancy (defined as 1–13 weeks; 3 Maasai, 4 Pare, and 7 Sengerema), 103 women in the 2nd trimester (14–27 weeks; 14 Maasai, 47 Pare, and 42 Sengerema), and 88 women in the 3rd trimester (28 weeks delivery; 16 Maasai, 41 Pare, and 31 Sengerema). Table 1 shows the characteristics of all pregnant women. There were no between-trimester differences in the general characteristics for each of the tribes. From the data of different trimesters, only body weight is shown. The Pare (p < 0.005) and Sengerema (p < 0.001) women in the 2nd and 3rd trimesters were heavier than the Maasai women and had a higher BMI during pregnancy compared to the Maasai (p < 0.001). The number of previous pregnancies was lower in Pare women, compared with Maasai (p = 0.003) and Sengerema (p = 0.003) women. The, for the current study, most relevant between-tribe difference was in fish intake. Fish consumption increased in the order Sengerema > Pare > Maasai.
Mother–infant pairs at delivery and at 3 months postpartum
We included 73 mother–infant pairs at delivery (8 Maasai, 31 Pare, and 34 Sengerema) and 110 different mother–infant pairs (9 Maasai, 40 Pare, and 61 Sengerema) after 3 months of exclusive breastfeeding. Their characteristics are also shown in Table 1. There were no between-tribe differences for the mothers at delivery or at 3 months postpartum, except for a lower BMI at delivery (p = 0.001) and higher length (p = 0.015) of the Maasai mothers compared to Pare mothers. Also in these groups, fish consumption occurred in the order Sengerema > Pare > Maasai at delivery and at 3 months postpartum.
Erythrocyte AA and DHA
RBC-FA data were available from all 205 women during pregnancy. At delivery, we studied different subjects. RBCs were available of 6 Maasai, 27 Pare, and 34 Sengerema women and 8 Maasai, 29 Pare, and 36 Sengerema infants. At 3 months postpartum, we included a group of different subjects including 9 Maasai, 38 Pare, and 60 Sengerema women and 8 Maasai, 38 Pare, and 61 Sengerema infants. Drop-out was due to failure to obtain consent for both mother and infant, early discharge (only at delivery), and logistical and analytical imperfections (delivery and 3 months postpartum).
Between- and within-tribe RBC-AA differences and mother–infant RBC-AA relation
Figure 1a (left panel) shows the apparent maternal and infant RBC-AA courses from the first trimester to 3 months postpartum. For convenience, data points are connected with dotted lines, but it should be noted that they are derived from different study groups. Visual inspection of the apparent courses of maternal RBC-AA during pregnancy did not reveal consistent changes. Maternal RBC-AA seemed to decrease in Pare (intermediate fish), but appeared constant in Maasai (low fish) and Sengerema (high fish) mothers. We analyzed between-tribe maternal RBC-AA differences at delivery. RBC-AA of Maasai women was higher than RBC-AA of Pare (p = 0.005) and Sengerema (p < 0.001), whereas Pare and Sengerema women did not show differences. The RBC-AA of the infants showed no between-tribe differences at delivery.
Apparent courses of red blood cell (RBC) arachidonic acid (AA, panel A) and docosahexaenoic acid (DHA, panel B) from the first trimester of pregnancy up to 3 months postpartum for Maasai (low fish), Pare (intermediate fish), and Sengerema (high fish) women and infants. Data represent means ± 2SEM in g/100 g (g%) fatty acids. They are derived from different maternal subgroups at the 1st, 2nd, and 3rd trimester and different mother–infant pairs at delivery and 3 months postpartum. Maternal and infant data are represented by closed and open symbols, respectively. PP, postpartum + significantly (sign) different from Maasai, pilcrow sign different from Pare, yen sign different from Sengerema, closed circle sign different from delivery, infinity sign different from mother
Within-tribe analysis of RBC-AA showed that in Maasai, Pare, and Sengerema mothers, RBC-AA at delivery was lower than at 3 months postpartum (p ≤ 0.001). In Maasai infants, there were no differences in RBC-AA between delivery and 3 months postpartum, whereas in Pare and Sengerema infants, RBC-AA was significantly higher at delivery as compared to 3 months postpartum (p ≤ 0.001). In all tribes, we found that at delivery, infant RBC-AA was significantly higher compared to maternal RBC-AA (Maasai p = 0.028, Pare p < 0.001, and Sengerema p < 0.001), but there was no relationship between infant RBC-AA and maternal RBC-AA (Fig. 2a).
Relationships between maternal and infant red blood cell (RBC) contents of AA (panel A) and DHA (panel B) at delivery for Maasai (low fish) (n = 6), Pare (intermediate fish) (n = 24), and the Sengerema (high fish) (n = 33) women and infants. Dotted lines indicate y = x for “equal AA or DHA sharing.” Maternal versus infant RBC-AA at delivery is insignificant. At delivery, maternal RBC-DHA equals infant RBC-DHA at 5.6 g%
Taken together, maternal RBC-AA was consistently lower at delivery compared to 3 months postpartum. Infant RBC-AA contents were similar at delivery and consistently higher than maternal RBC-AA. Thus, biomagnification of AA during pregnancy occurred, irrespective of maternal AA status (Figs. 1a, 2a). After 3 months of exclusive breastfeeding, infant RBC-AA was lower compared to delivery in Pare (intermediate fish) and Sengerema (high fish). This decline did not reach significance for the Maasai (low fish), probably because of low numbers.
Between- and within-tribe RBC-DHA differences and mother–infant RBC-DHA relation
Figure 1b (right panel) shows the apparent courses of maternal and infant RBC-DHA contents from the first trimester to 3 months postpartum. Visual inspection of maternal RBC-DHA during pregnancy revealed a trend of higher RBC-DHA in late pregnancy of the Pare and the Maasai, but not the women in Sengerema. Analysis of the between-tribe maternal and infant RBC-DHA differences showed that at delivery, RBC-DHA in Sengerema (high fish) women was higher compared to Pare (intermediate fish) and Maasai (low fish) at p ≤ 0.001, whereas Pare and Maasai women showed no differences.
Within-tribe RBC-DHA differences showed that in all tribes, maternal DHA at delivery was higher than at 3 months postpartum (Maasai p = 0.003; Pare and Sengerema p ≤ 0.001). In the infants, Maasai had higher RBC-DHA at delivery compared to 3 months postpartum (p = 0.039); Pare did not show a significant difference between delivery and 3 months postpartum, while Sengerema infants showed a lower RBC-DHA at delivery compared to 3 months postpartum (p = 0.027).
At delivery, the analysis of mother–infant pairs differences revealed that Maasai (low fish) (p = 0.245) and Pare (intermediate fish) (p = 0.091) infants, although insignificant, tended to have higher RBC-DHA than their mothers, while (in contrast) the RBC-DHA of the Sengerema (high fish) infants was lower (p = 0.029) compared to their mothers. The relationship between maternal and infant RBC-DHA at delivery is shown in Fig. 2b. For this analysis, we selected data of complete mother–infant pairs (6 Maasai, 24 Pare, and 33 Sengerema). At low maternal DHA status, infants usually had higher RBC-DHA than their mothers (biomagnification), but in contrast, at high maternal DHA status, infant RBC-DHA was generally lower (“bioattenuation”). Figure 2b indicates that equal RBC-DHA in mothers and infants at delivery was reached at a maternal RBC-DHA of 5.6 g%.
Although our data are not longitudinal, it appeared that at low maternal RBC-DHA, infant RBC-DHA decreased from delivery until 3 months postpartum, whereas at high maternal DHA status, infant RBC-DHA increased from delivery until 3 months postpartum. We subsequently calculated the maternal DHA status at which the infant appeared to be in a state of postpartum DHA equilibrium. In other words, we estimated the maternal RBC-DHA status from which the infant showed no changes in RBC-DHA from delivery to 3 months postpartum. Figure 3 shows the relationship between infant RBC-DHA at delivery and at 3 months postpartum for the Maasai, Pare, and Sengerema. Only mean values for each of the tribes could be used, since we did not study the same infants at delivery and at 3 months postpartum. Figure 3 indicates that a postpartum infant RBC-DHA equilibrium was reached at an infant RBC-DHA of 5.9 g% at delivery. In turn, this infant RBC-DHA corresponds with a maternal RBC-DHA of 6.1 g% at delivery (by inserting 5.9 into equation of Fig. 2b). The number of included Maasai was low. Exclusion of their data did, however, not change the equation in Fig. 3.
Relationship between the mean red blood cell (RBC) docosahexaenoic acid (DHA) at delivery and at 3 months postpartum for the Maasai, Pare, and Sengerema infants, respectively. Data represent means ± 2SEM in g/100 g (g%) fatty acids. Infant RBC-DHA at delivery equals infant RBC-DHA at 3 months postpartum at 5.9 g%
Taken together, maternal RBC-DHA contents at both high and low DHA status were lower after 3 months of exclusive lactation, compared with delivery. Biomagnification of DHA seems to occur up to a maternal RBC-DHA of 5.6 g% at delivery, and from this turning point, DHA becomes “bioattenuated.” Postpartum infant RBC-DHA equilibrium was reached at an infant RBC-DHA of about 5.9 g% at delivery, corresponding to a maternal RBC-DHA of 6.1 g% during pregnancy and at delivery. For all practical reasons, we conclude that biomagnification takes place up to a maternal RBC-DHA status of about 6 g%, and that also infant postnatal RBC-DHA equilibrium is reached at about 6 g%.
Discussion
We determined the RBC-AA and DHA contents of pregnant Tanzanian women and of mother–infant pairs at delivery and at 3 months postpartum. The mothers had stable dietary intakes characterized by low (Maasai), intermediate (Pare), and high (Sengerema) consumption of freshwater fish. Our main findings are that biomagnification of AA occurs irrespective of maternal AA status. In contrast to maternal RBC-AA, infant RBC-AA at delivery was remarkably uniform and also after 3 months exclusive lactation, although to a lesser extent. There was no relationship between maternal and infant RBC-AA. From delivery to 3 months postpartum, maternal RBC-AA increased, while infant RBC-AA decreased. Maternal and infant RBC-DHA were higher in the sequence Sengerema (high fish) > Pare (intermediate fish) > Maasai (low fish). In contrast to RBC-AA, maternal and infant RBC-DHA were intimately related. Biomagnification of DHA occurred up to a maternal RBC-DHA of 5.6 g% at delivery; from this turning point, DHA became “bioattenuated”. From delivery to 3 months postpartum, maternal RBC-DHA decreased, while infant RBC-DHA decreased in Maasai (low fish), remained constant in Pare (intermediate fish), and increased in Sengerema (high fish). Postpartum infant RBC-DHA equilibrium was reached at an infant RBC-DHA of about 5.9 g% at delivery, corresponding to a maternal RBC-DHA of 6.1 g% during pregnancy and at delivery.
Arachidonic acid (AA)
The higher RBC-AA contents in Maasai (low fish), compared to Pare (intermediate fish) and Sengerema (high fish) mothers (Fig. 1a), are likely to be caused by their higher intakes of AA from meat and their low intakes of DHA from fish. Biomagnification [13] of AA is consistent with data from many others studying plasma PL [14, 29] or RBC [30–32]. Higher infant compared to maternal RBC-AA at delivery was previously found by us in Dominica [33] and by others in the Netherlands [32], and the data of those 2 studies fitted well within those of the present study (Dominica: mean maternal RBC-AA 12.4 g%, infant 16.6 g%; Netherlands: mean maternal RBC-AA 10.0 g%, infant 14.2 g% AA). The uniformly high infant RBC-AA at delivery occurred despite between-tribe differences in maternal RBC-AA and DHA (Fig. 1a, b), and in the absence of a relationship between maternal and infant RBC-AA (Fig. 2a).
Although we observed no consistent changes in maternal RBC-AA during pregnancy, maternal RBC-AA was consistently higher after 3 months of exclusive lactation as compared to delivery, which coincided with a drop of infant RBC-AA. The decreasing maternal AA status during pregnancy found by Al et al. [14] and the well-known postnatal drop of infant RBC-AA [34] suggests that the fetus accretes AA at the expense of maternal AA status. However, no clear relationship between maternal and infant RBC-AA could be demonstrated in our data, which may question the causality of these opposing changes. The increasing maternal AA status after delivery may derive from the discontinued utilization of AA by the placenta or discontinued AA transport to the fetus [35, 36]. Secondly, the postpartum increasing maternal AA status may result from decreasing maternal adipose tissue lipolysis and decreasing de novo lipogenesis (DNL), secondary to the changing hormonal milieu after delivery, notably the restoration of the state of diminished insulin sensitivity/compensatory hyperinsulinemia in the end of pregnancy. Discontinuation of the influx of these sources of saturated fatty acids (SAFA), monosaturated fatty acids (MUFA), and PUFA (i.e., notably linoleic acid) leads to less dilution of LCP [35, 36]. The decrease in infant RBC-AA may have been caused by postpartum changing infant RBC-PL species [37] and the interrupted transplacental AA transport [35, 36]. It can additionally be explained by a lower conversion of LA to AA, since the infant’s capacity to synthesize LC-PUFA decreases drastically after delivery [38]. This lower conversion might result from lower activities of the delta-5 and delta-6 desaturase enzymes, secondary to the changing hormonal milieu after delivery. Finally, LA intakes correlate inversely with RBC-AA [39]. Consequently, the high LA content of human milk (Kuipers, unpublished) and the ensuing postnatal surge in the infant LA status [35] suggest that the infant’s RBC-AA decrease may also be a result of the high LA intake from breast milk. At 3 months of age, infant RBC-AA in Pare (intermediate fish) and Sengerema (high fish) was comparable to that of their mothers, indicating a rapid postnatal adaptation of RBC-AA to adult levels. Taken together, AA biomagnification seems to aim at a uniform, high infant AA status during pregnancy, most likely to sustain neurodevelopment and infant growth [40].
Docosahexaenoic acid (DHA)
As expected [41], maternal DHA status, and thereby infant RBC-DHA status, appeared highly sensitive to maternal fish intake. The virtually constant maternal RBC-DHA levels during pregnancy are in accordance with earlier data for plasma PL [14, 42].
At delivery, infant RBC-DHA appeared higher than maternal RBC-DHA, but this “‘biomagnification” occurred only up to about 5.6 g% maternal RBC-DHA. Beyond this point of maternal–fetal equilibrium, infant RBC-DHA was mostly lower than maternal RBC-DHA, suggesting “bioattenuation”, rather than biomagnification (Fig. 2b). The mean RBC-DHA data for a Dutch population [32] (with low fish intakes) and a Dominican population [33] (Caribbean Sea; with local high fish intakes) are consistent with the switch from biomagnification to bioattenuation at a higher maternal RBC-DHA status (Dominica: mean maternal RBC-DHA 7.6 g%, infants 6.5 g%; Netherlands: mean maternal 3.9 g%, infants 4.7 g%). In other words, biomagnification might be confined to populations with low maternal DHA status, such as typically encountered in most Western countries, but also the currently studied Pare (intermediate fish) and Maasai (no fish), who, in contrast to the high fish consuming Sengerema women, exhibited tendencies of increasing RBC-DHA during pregnancy (Fig. 1b). Increasing amounts of DHA in the maternal circulation during pregnancy [43, 44] might derive from an insulin-induced augmented elongation/desaturation of ALA in the maternal liver, secondary to the state of reduced insulin sensitivity/compensatory hyperinsulinism that is characteristic for the third trimester [35]. This maternal DHA increase is unlikely to occur at high fish intakes such as in the women from Sengerema, because of the negative feedback of dietary DHA on delta-5 and delta-6 desaturase activity (Fig. 1b). The DHA increase in the maternal circulation might be a driving force in biomagnification that is further supported by selective transport to the fetal circulation [45]. Fetal albumin has been regarded as a major contributor to LCP biomagnification because of its ability to bind placentally transferred free LC-PUFA, while fetal albumin concentrations at term are also 10–20% higher, and albumin’s free fatty acid saturation is four times lower, in the fetal circulation compared to the maternal circulation. A role of the uniquely present alpha fetoprotein (AFP) with similar free fatty acid loading capacity in the fetal circulation was dismissed because of its 1,000 times lower concentration compared to albumin in the fetus [46]. AFP, however, has high preference for AA and DHA and is preferentially to albumin taken up by immature tissues, suggesting that, rather than concentrations, notably fluxes of LC-PUFA trapping proteins might be important for biomagnification. Another suggested mechanism for the trapping of LC-PUFA is the incorporation of free LC-PUFA from the fetal circulation into phospholipids in the liver or other organs [46].
Higher maternal compared to infant RBC-DHA contents were previously noted after daily supplementation of pregnant women from 20 weeks of gestation until delivery with a high fish oil supplement containing 2.24 g DHA and 1.12 g EPA [47]. In this study, a maternal–fetal equilibrium was found at an RBC-DHA of 8.87 g%, named “saturation point”. A possible explanation for the equilibrium at higher maternal RBC-DHA than the current about 6 g% is that fish oil was supplemented during the 3rd trimester of pregnancy, which is characterized by reduced insulin sensitivity and continuous adipose tissue mobilization [48]. Therefore, the supplemental DHA might have been abundantly available for incorporation into circulating lipids, and to a lesser extent to adipose tissue stores, which might have resulted in an overestimation of the genuine whole body DHA status during this non-steady state condition characterized by preferential nutrient transfer to the rapidly growing infant. In our study, circulating DHA derived from lifelong stable fish intakes that probably caused a steady state DHA supply of the infant from both the diet and adipose tissue stores.
Data from our populations with stable high intakes of fish suggest that DHA bioattenuation aims at the inhibition of abundant transplacental passage, possibly to prevent undesired competition of DHA with AA in competition-sensitive fetal organs. Consistent with this notion, we have shown that at high DHA status, DHA seems to lower AA, at least in postnatal RBC, but that in umbilical vessels, DHA does not seem to exceed certain levels, possibly to avoid competition with AA [49]. Prevention of DHA competition with AA in the fetal period seems important, since fetal AA is implicated in development and growth [10, 50].
The consistent decrease in maternal RBC-DHA during lactation suggests that a lactating woman loses large quantities of DHA to her infant via the milk. This postpartum mother-to-infant DHA “surge” [51] may represent a genuine form of “postnatal DHA biomagnification”, since it clearly occurs at the expense of the mother. This surge coincides with a more rapid postnatal accretion of DHA in the infant brain compared with AA [52] and may therefore illustrate the increasing importance of DHA for retinal and neurodevelopment [52, 53] after delivery.
The mother-to-infant DHA surge via the milk seemed unable to prevent a RBC-DHA drop in the Maasai (low fish) infants, prevented a decrease in the Pare (intermediate fish) infants, but did enable a postpartum RBC-DHA increase in the infants of the Sengerema (high fish) women (Fig. 1b). A state of postpartum infant DHA equilibrium might therefore be reached at lifelong DHA intakes that are somewhat below the intakes by the Sengerema (high fish) women, who reported to eat fish 4–5 times/week on average. Using the joint data of all mothers and infants, we estimated that mothers with an RBC-DHA status of about 6 g% in early pregnancy will exhibit an RBC-DHA of about 6 g% at delivery and will give birth to infants with about 6 g% RBC-DHA. Whether this maternal RBC-DHA of 6 g% constitutes an appropriate target for the DHA status of the mother is questionable, since a maternal RBC-DHA of 6 g% is unable to prevent a drop in maternal RBC-DHA during lactation. We [51] recently showed that maternal postpartum DHA equilibrium is reached at a maternal RBC-DHA content of 8 g% DHA, which is even higher than the mean DHA status of the pregnant women in Sengerema and coincides with an increase in infant RBC-DHA from 7 g% at delivery to adult levels of 8 g% at 3 months.
We recently estimated that our hunter-gatherer ancestors living in a water–land ecosystem had daily intakes of gram amounts of AA, EPA, and DHA [5], which are substantially higher than the current daily intakes of about 200 mg AA and 275 mg DHA (men) from a typically Western diet [8, 54]. There is also good evidence showing that daily intakes above the recommended 450 mg DHA + EPA might be beneficial for the lowering of heart rate, blood pressure, and triglycerides and to reach maximum antithrombotic effects [55]. It has been proposed that optimal protection from cardiovascular disease occurs from 8 g% RBC EPA + DHA [56, 57], while an RBC-DHA of 7 g% [i.e., RBC-(EPA + DHA) ≥ 8 g%], as found in healthy subjects in Japan, might be an appropriate target to minimize major depressive disorders and bipolar depression [56]. The above-mentioned maternal postpartum equilibrium of 8 g% [51] is in line with these suggested targets for adequate DHA status and also the observation that antagonism between EPA + DHA and AA occurs at RBC-(EPA + DHA) contents above 8 g% [49].
Pregnant women in Western countries with low intakes of fish have RBC-DHA contents well below 8 g%. For example, non-supplemented Dutch pregnant women had RBC-DHA contents of 4.41 g% at 36 weeks [19], while after 12 weeks of exclusive lactation, their infants had an RBC-DHA content of 4.73 g%. Supplementation of 220 mg DHA or 220 mg DHA + 220 mg AA during pregnancy resulted in a maternal RBC-DHA contents of 5.51 and 5.57 g% at 36 weeks gestation, respectively [19], while their exclusively breastfed infants had RBC-DHA of 5.50 and 4.95 g%, respectively, at 12 weeks postpartum. The mean daily intake of EPA + DHA by Dutch women amounted to 84 mg in 2003 [58]. In another study, daily supplementation of 1.3 g DHA during 3 months of lactation resulted in a maternal RBC-DHA of 7.9 g% [59] that coincided with an infant RBC-DHA content of 9.1 g% [60]. Taken together, these data suggest that the presently advised intake of 200–300 mg DHA daily during pregnancy and lactation [61] will be insufficient to reach the maternal RBC-DHA target of 6 g% (i.e., postpartum infant equilibrium) and will be even more insufficient to reach the target of 8 g% RBC-DHA (i.e., postpartum maternal equilibrium and infant increase) [51].
Limitations
It should be noted that, because of local constraints, the data for each tribe were derived from different subgroups that were studied at various occasions during pregnancy and lactation. We interpreted differences between these subgroups in terms of longitudinal changes, as based on between-group statistical differences. This reasoning seems justified because of their stable dietary intakes. In addition, the courses of RBC-AA and DHA during pregnancy and lactation were comparable with those of Dutch women, as determined in plasma PL [14]. Another limitation might be the use of RBC-LCP data as proxies for whole body LCP status. Their use is supported by animal experiments [62], and therefore, RBC-AA and DHA contents are nowadays widely regarded as reliable parameters for LCP status [27]. There are, however, few data at very high DHA intakes on the efficiency of DHA incorporation in the various compartments (e.g., brain), and it may be expected that each of these compartments will ultimately become “saturated” to reach compartment-specific DHA saturation levels, as e.g., suggested by the DHA contents of umbilical arteries and veins [49]. The difficulty to include women in their first trimester of pregnancy resulted into a small sample size. Few women attend to local hospitals in early pregnancy. Because of the low numbers, we refrained from statistical analyses of these data. Also, the DHA status during pregnancy was previously shown to be influenced by the number of previous pregnancies [63]. However, in the present study, we found no significant DHA status differences in women with 1, 2, or multiple previous pregnancies (data not shown). Finally, the LC-PUFA status of the various tribes might be influenced by genetic variants (e.g., FADS 1 and FADS2 polymorphism), but these were not taken into account in the present study.
Conclusions
From the present data from populations with lifelong stable dietary habits, we conclude that infant AA status at delivery is uniform, high, and unrelated to maternal AA status, which might indicate the importance of fetal AA for growth and brain development. DHA status of mother and infant is on the other hand intimately related and strongly dependent on the DHA intake from fish. Beyond a maternal steady state RBC-DHA of about 6 g%, biomagnification turns into bioattenuation, which may aim at the prevention of DHA competition with AA in infant organs that are sensitive to DHA versus AA competition. A maternal RBC-DHA of about 6 g% from early pregnancy up to delivery predicts an infant RBC-DHA of about 6 g% at delivery, which will not change during subsequent exclusive breastfeeding. Infant equilibrium, however, coincides with maternal DHA losses during lactation. The mother-to-infant DHA surge during lactation may represent the genuine form of biomagnification. Bioattenuation, rather than biomagnification, might be the physiological standard for humans, because of our ancestry from the land–water ecosystem and since studies on the prevention of cardiovascular disease and depression indicate optimal RBC-DHA contents above 7 g%. It is important to stress that all of the present data derive from populations with stable dietary habits and may not be applicable to the state of non-equilibrium that is typical for the so far conducted short-term supplementation studies with DHA and AA during pregnancy and lactation.
References
Serhan CN, Chiang N (2008) Endogenous pro-resolving and anti-inflammatory lipid mediators: a new pharmacologic genus. Br J Pharmacol 153(Suppl 1):S200–S215
Innis SM (2009) Omega-3 Fatty acids and neural development to 2 years of age: do we know enough for dietary recommendations? J Pediatr Gastroenterol Nutr 48(Suppl 1):S16–S24
Calder PC (2007) Dietary arachidonic acid: harmful, harmless or helpful? Br J Nutr 98:451–453
Kuipers RS, Fokkema MR, Smit EN, van der Meulen J, Boersma ER, Muskiet FA (2005) High contents of both docosahexaenoic and arachidonic acids in milk of women consuming fish from lake Kitangiri (Tanzania): targets for infant formulae close to our ancient diet? Prostaglandins Leukot Essent Fatty Acids 72:279–288
Kuipers RS, Luxwolda MF, Dijck-Brouwer DA, Eaton SB, Crawford MA, Cordain L et al (2010) Estimated macronutrient and fatty acid intakes from an East African Paleolithic diet. Br J Nutr 104:1666–1687
Cordain L, Eaton SB, Sebastian A, Mann N, Lindeberg S, Watkins BA et al (2005) Origins and evolution of the Western diet: health implications for the 21st century. Am J Clin Nutr 81:341–354
Simopoulos AP (2006) Evolutionary aspects of diet, the omega-6/omega-3 ratio and genetic variation: nutritional implications for chronic diseases. Biomed Pharmacother 60:502–507
Astorg P, Arnault N, Czernichow S, Noisette N, Galan P, Hercberg S (2004) Dietary intakes and food sources of n-6 and n-3 PUFA in French adult men and women. Lipids 39:527–535
Ramsden CE, Faurot KR, Carrera-Bastos P, Cordain L, De Lorgeril M, Sperling LS (2009) Dietary fat quality and coronary heart disease prevention: a unified theory based on evolutionary, historical, global, and modern perspectives. Curr Treat Options Cardiovasc Med 11:289–301
Hornstra G (2000) Essential fatty acids in mothers and their neonates. Am J Clin Nutr 71:1262S–1269S
Burdge GC, Wootton SA (2002) Conversion of alpha-linolenic acid to eicosapentaenoic, docosapentaenoic and docosahexaenoic acids in young women. Br J Nutr 88:411–420
Martinez M (1992) Tissue levels of polyunsaturated fatty acids during early human development. J Pediatr 120:S129–S138
Crawford MA, Hassam AG, Williams G, Whitehouse WL (1976) Essential fatty-acids and fetal brain growth. Lancet 1:452–453
Al MD, van Houwelingen AC, Kester AD, Hasaart TH, de Jong AE, Hornstra G (1995) Maternal essential fatty acid patterns during normal pregnancy and their relationship to the neonatal essential fatty acid status. Br J Nutr 74:55–68
Otto SJ, van Houwelingen AC, Badart-Smook A, Hornstra G (2001) Comparison of the peripartum and postpartum phospholipid polyunsaturated fatty acid profiles of lactating and nonlactating women. Am J Clin Nutr 73:1074–1079
Decsi T (2009) Effects of supplementing LCPUFA to the diet of pregnant women: data from RCT. Adv Exp Med Biol 646:65–69
Simmer K, Patole SK, Rao SC (2008) Longchain polyunsaturated fatty acid supplementation in infants born at term. Cochrane Database Syst Rev 23(1):CD000376
Simmer K, Schulzke SM, Patole S (2008) Longchain polyunsaturated fatty acid supplementation in preterm infants. Cochrane Database Syst Rev 23(1):CD000375
van Goor SA, Schaafsma A, Erwich JJ, Dijck-Brouwer DA, Muskiet FA (2010) Mildly abnormal general movement quality in infants is associated with higher Mead acid and lower arachidonic acid and shows a U-shaped relation with the DHA/AA ratio. Prostaglandins Leukot Essent Fatty Acids 82:15–20
McCann JC, Ames BN (2005) Is docosahexaenoic acid, an n-3 long-chain polyunsaturated fatty acid, required for development of normal brain function? An overview of evidence from cognitive and behavioral tests in humans and animals. Am J Clin Nutr 82:281–295
Makrides M, Neumann MA, Byard RW, Simmer K, Gibson RA (1994) Fatty acid composition of brain, retina, and erythrocytes in breast- and formula-fed infants. Am J Clin Nutr 60:189–194
Birch EE, Carlson SE, Hoffman DR, Fitzgerald-Gustafson KM, Fu VL, Drover JR et al (2010) The DIAMOND (DHA intake and measurement of neural development) study: a double-masked, randomized controlled clinical trial of the maturation of infant visual acuity as a function of the dietary level of docosahexaenoic acid. Am J Clin Nutr 91:848–859
Simopoulos AP (2009) Evolutionary aspects of the dietary omega-6:omega-3 fatty acid ratio: medical implications. World Rev Nutr Diet 100:1–21
Broadhurst CL, Cunnane SC, Crawford MA (1998) Rift Valley lake fish and shellfish provided brain-specific nutrition for early Homo. Br J Nutr 79:3–21
Braun DR, Harris JW, Levin NE, McCoy JT, Herries AI, Bamford MK et al (2010) Early hominin diet included diverse terrestrial and aquatic animals 1.95 Ma in East Turkana, Kenya. Proc Natl Acad Sci USA 107:10002–10007
Kuipers RS, Smit EN, van der Meulen J, Janneke Dijck-Brouwer DA, Rudy Boersma E, Muskiet FA (2007) Milk in the island of Chole (Tanzania) is high in lauric, myristic, arachidonic and docosahexaenoic acids, and low in linoleic acid reconstructed diet of infants born to our ancestors living in tropical coastal regions. Prostaglandins Leukot Essent Fatty Acids 76:221–233
Hodson L, Skeaff CM, Fielding BA (2008) Fatty acid composition of adipose tissue and blood in humans and its use as a biomarker of dietary intake. Prog Lipid Res 47:348–380
Muskiet FA, van Doormaal JJ, Martini IA, Wolthers BG, van der Slik W (1983) Capillary gas chromatographic profiling of total long-chain fatty acids and cholesterol in biological materials. J Chromatogr 278:231–244
Elias SL, Innis SM (2001) Infant plasma trans, n-6, and n-3 fatty acids and conjugated linoleic acids are related to maternal plasma fatty acids, length of gestation, and birth weight and length. Am J Clin Nutr 73:807–814
Crawford MA, Golfetto I, Ghebremeskel K, Min Y, Moodley T, Poston L et al (2003) The potential role for arachidonic and docosahexaenoic acids in protection against some central nervous system injuries in preterm infants. Lipids 38:303–315
Montgomery C, Speake BK, Cameron A, Sattar N, Weaver LT (2003) Maternal docosahexaenoic acid supplementation and fetal accretion. Br J Nutr 90:135–145
Vlaardingerbroek H, Hornstra G (2004) Essential fatty acids in erythrocyte phospholipids during pregnancy and at delivery in mothers and their neonates: comparison with plasma phospholipids. Prostaglandins Leukot Essent Fatty Acids 71:363–374
van Beusekom CM, Nijeboer HJ, van der Veere CN, Luteyn AJ, Offringa PJ, Muskiet FA et al (1993) Indicators of long chain polyunsaturated fatty acid status of exclusively breastfed infants at delivery and after 20–22 days. Early Hum Dev 32:207–218
Makrides M, Simmer K, Neumann M, Gibson R (1995) Changes in the polyunsaturated fatty acids of breast milk from mothers of full-term infants over 30 wk of lactation. Am J Clin Nutr 61:1231–1233
Kuipers RS, Luxwolda MF, Sango WS, Kwesigabo G, Velzing-Aarts FV, Dijck-Brouwer DA et al (2011) Postpartum changes in maternal and infant erythrocyte fatty acids are likely to be driven by restoring insulin sensitivity and DHA status. Med Hypotheses 76:794–801
Kuipers RS, Luxwolda MF, Sango WS, Kwesigabo G, Dijck-Brouwer DA, Muskiet FA (2011) Postdelivery changes in maternal and infant erythrocyte fatty acids in 3 populations differing in fresh water fish intakes. Prostaglandins Leukot Essent Fatty acids (in press)
Neerhout RC (1968) Erythrocyte lipids in the neonate. Pediatr Res 2:172–178
Carnielli VP, Simonato M, Verlato G, Luijendijk I, De Curtis M, Sauer PJ et al (2007) Synthesis of long-chain polyunsaturated fatty acids in preterm newborns fed formula with long-chain polyunsaturated fatty acids. Am J Clin Nutr 86:1323–1330
Friesen RW, Innis SM (2010) Linoleic acid is associated with lower long-chain n-6 and n-3 fatty acids in red blood cell lipids of Canadian pregnant women. Am J Clin Nutr 91:23–31
Carlson SE, Werkman SH, Peeples JM, Cooke RJ, Tolley EA (1993) Arachidonic acid status correlates with first year growth in preterm infants. Proc Natl Acad Sci USA 90:1073–1077
Innis SM (2008) Dietary omega 3 fatty acids and the developing brain. Brain Res 1237:35–43
Otto SJ, Houwelingen AC, Antal M, Manninen A, Godfrey K, Lopez-Jaramillo P et al (1997) Maternal and neonatal essential fatty acid status in phospholipids: an international comparative study. Eur J Clin Nutr 51:232–242
Haggarty P (2004) Effect of placental function on fatty acid requirements during pregnancy. Eur J Clin Nutr 58:1559–1570
Postle AD, Al MD, Burdge GC, Hornstra G (1995) The composition of individual molecular species of plasma phosphatidylcholine in human pregnancy. Early Hum Dev 43:47–58
Larque E, Demmelmair H, Berger B, Hasbargen U, Koletzko B (2003) In vivo investigation of the placental transfer of (13)C-labeled fatty acids in humans. J Lipid Res 44:49–55
Haggarty P (2010) Fatty acid supply to the human fetus. Annu Rev Nutr 30:237–255
Dunstan JA, Mori TA, Barden A, Beilin LJ, Holt PG, Calder PC et al (2004) Effects of n-3 polyunsaturated fatty acid supplementation in pregnancy on maternal and fetal erythrocyte fatty acid composition. Eur J Clin Nutr 58:429–437
Hadden DR, McLaughlin C (2009) Normal and abnormal maternal metabolism during pregnancy. Semin Fetal Neonatal Med 14:66–71
Luxwolda MF, Kuipers RS, Smit EN, Velzing-Aarts FV, Janneke Dijck-Brouwer DA, Muskiet FA (2011) The relation between the omega-3 index and arachidonic acid is bell shaped: Synergistic at low EPA + DHA status and antagonistic at high EPA + DHA status. Prostaglandins Leukot Essent Fatty Acids
Woltil HA, van Beusekom CM, Schaafsma A, Muskiet FA, Okken A (1998) Long-chain polyunsaturated fatty acid status and early growth of low birth weight infants. Eur J Pediatr 157:146–152
Kuipers RS, Luxwolda MF, Sango WS, Kwesigabo G, Dijck-Brouwer DA, Muskiet FA (2011) Maternal DHA equilibrium during pregnancy and lactation is reached at an erythrocyte DHA content of 8 g/100 g fatty acids. J Nutr 141:418–427
Martinez M, Mougan I (1998) Fatty acid composition of human brain phospholipids during normal development. J Neurochem 71:2528–2533
Carlson SE, Cooke RJ, Rhodes PG, Peeples JM, Werkman SH, Tolley EA (1991) Long-term feeding of formulas high in linolenic acid and marine oil to very low birth weight infants: phospholipid fatty acids. Pediatr Res 30:404–412
Zhou L, Nilsson A (2001) Sources of eicosanoid precursor fatty acid pools in tissues. J Lipid Res 42:1521–1542
Mozaffarian D, Rimm EB (2006) Fish intake, contaminants, and human health: evaluating the risks and the benefits. JAMA 296:1885–1899
McNamara RK (2009) Evaluation of docosahexaenoic acid deficiency as a preventable risk factor for recurrent affective disorders: current status, future directions, and dietary recommendations. Prostaglandins Leukot Essent Fatty Acids 81:223–231
Harris WS, Von Schacky C (2004) The Omega-3 Index: a new risk factor for death from coronary heart disease? Prev Med 39:212–220
Kruizinga AG, Westenbrink S, van Bosch LMC, Jansen MCJF (2007) Results of the national food consumption survey, research 7451, VCP 2003. http://www.voorlichtingmvo.nl/gfx/file/TNO-onderzoek_V7451.pdf. Accessed 14 March 2007
Makrides M, Neumann MA, Gibson RA (1996) Effect of maternal docosahexaenoic acid (DHA) supplementation on breast milk composition. Eur J Clin Nutr 50:352–357
Gibson RA, Neumann MA, Makrides M (1997) Effect of increasing breast milk docosahexaenoic acid on plasma and erythrocyte phospholipid fatty acids and neural indices of exclusively breast fed infants. Eur J Clin Nutr 51:578–584
Guesnet P, Alessandri JM (2011) Docosahexaenoic acid (DHA) and the developing central nervous system (CNS)—Implications for dietary recommendations. Biochimie 93:7–12
van Goor SA, Dijck-Brouwer DA, Fokkema MR, van der Iest TH, Muskiet FA (2008) Maternal and fetal brain contents of docosahexaenoic acid (DHA) and arachidonic acid (AA) at various essential fatty acid (EFA), DHA and AA dietary intakes during pregnancy in mice. Prostaglandins Leukot Essent Fatty Acids 78:159–169
Al MD, van Houwelingen AC, Hornstra G (1997) Relation between birth order and the maternal and neonatal docosahexaenoic acid status. Eur J Clin Nutr 51:548–553
Acknowledgments
We thank NIMR Tanzania for their correspondence and help in the writing of our proposal for ethical clearance. We further thank em. Prof. E.R. Boersma, Prof. J. J. M. van Roosmalen, Prof. S. Massawe, Prof. A. Massawe, Prof. G. V. Mann, J. van der Meulen, P. Gunneweg, P. Schwerzel, R. Shaffer, Dr. J. Changalucha, Drs. C. van Rij, Sr. M. J. Voeten, J. Lugalla, G. Msafiri, N. Mchomvu, S. Mazzuki, rafiki Martini, and all other staff, doctors, and nurses from the local hospitals in Tanzania for their help in our project. We thank Dr. M. R. Heiner-Fokkema, Dr. M. Volmer, I. A. Martini, H. Velvis, and M. Velvis for their statistical and technical assistance and the VSB Foundation and FrieslandCampina (Dr. A. Schaafsma) for their financial support. There are no conflicts of interest.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Additional information
Martine F. Luxwolda and Remko S. Kuipers contributed equally to this paper.
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Luxwolda, M.F., Kuipers, R.S., Sango, W.S. et al. A maternal erythrocyte DHA content of approximately 6 g% is the DHA status at which intrauterine DHA biomagnifications turns into bioattenuation and postnatal infant DHA equilibrium is reached. Eur J Nutr 51, 665–675 (2012). https://doi.org/10.1007/s00394-011-0245-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-011-0245-9