Abstract
Background
Reliability of left ventricular function measurements depends on actual biological conditions, repeated registrations and their analyses.
Objective
To investigate test–retest reliability of speckle-tracking-derived strain measurements and its determinants compared to the conventional parameters, such as ejection fraction (EF), LV volumes and mitral annular plane systolic excursion (MAPSE).
Methods
In 30 patients with a wide range of left ventricular function (mean EF 46.4 ± 16.4%, range 14–73%), standard echo views were acquired independently in a blinded fashion by two different echocardiographers in immediate sequence and analyzed off-line by two independent readers, creating 4 data sets per patient. Test–retest reliability of studied parameters was calculated using the smallest detectable change (SDC) and a total, inter-acquisition and inter-reader intra-class correlation coefficient (ICC).
Results
The smallest detectable change normalized to the mean absolute value of the measured parameter (SDCrel) was lowest for MAPSE (10.7%). SDCrel for EF was similar to GLS (14.2 and 14.7%, respectively), while SDCrel for CS was much higher (35.6%). The intra-class correlation coefficient was excellent (> 0.9) for all measures of the left ventricular function. Intra-patient inter-acquisition reliability (ICCacq) was significantly better than inter-reader reliability (ICCread) (0.984 vs. 0.950, p = 0.03) only for EF, while no significant difference was observed for any other LV function parameter. Mean intra-subject standard deviations were significantly correlated to the mean values for CS and LV volumes, but not for the other studied parameters.
Conclusions
In a test–retest setting, both with normal and impaired left ventricular function, the smallest relative detectable change of EF, GLS and MAPSE was similar (11–15%), but was much higher for CS (35%). Surprisingly, reliability of GLS was not superior to that of EF. Acquisition and reader to a similar extent influenced the reliability of measurements of all left ventricular function measures except for ejection fraction, where the reliability was more dependent on the reader than on the acquisition.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Evaluation of left ventricular (LV) function remains a crucial issue in clinical decision-making and risk stratification across different cardiac disorders. Recently introduced speckle-tracking-derived measures of myocardial deformation, mainly the global peak systolic longitudinal strain (GLS), have emerged as a new standard in the assessment of LV function, with the potential of complementing or even replacing ejection fraction (EF) due to the well-recognized examiner-dependency of the latter [1,2,3,4]. GLS has been reported to be superior to EF in the detection of incipient heart failure of different etiologies, for example the cardio toxic effects of cancer therapy [5, 6], aortic stenosis [7] or amyloidosis [8]. Since GLS is a semi-automatically generated parameter, it might be less affected by user input. However, although the image processing is largely performed by machine and software, image acquisition continues to be operator-dependent.
Evaluation of the test–retest reliability in a real-life clinical setting is crucial to distinguish the effects of the disease (biological variability) from the variability of the measurement. The variability of the measurement depends both on acquisition and reading variability and therefore is more complex, but also more realistic than inter-observer or intra-observer variability, which focus on repeated analyses of the same not-repeated registrations. Much more limited data exist on the test–retest reliability of functional left ventricular parameters than on their observer variability.
The purpose of this study was to investigate test–retest reliability of speckle-tracking-derived LV strain measurements (global peak systolic longitudinal strain (GLS) and circumferential strain (CS)) and its determinants in relation to the conventional parameters, such as ejection fraction (EF) calculated from end-diastolic (EDV) and end-systolic volumes (ESV), and mitral annular plane systolic excursion (MAPSE), in a prospective study of patients with a wide range of left ventricular function.
Materials and methods
A total of 30 patients in sinus rhythm with different degrees of LV function impairment were prospectively recruited in the study. All the patients were referred from the Department of Cardiology or outpatient clinic, Uppsala University Hospital, for a routine transthoracic echocardiography for different indications and had acceptable acoustic windows. The rate of recruitment was determined by whether two of the three echo examiners (TB, EMH, FAF) could acquire the data at the scheduled time in a patient fulfilling the above criteria. No other selection criteria were applied. The study was approved by the Regional Ethical Review Board at Uppsala University (Reference number: 2013/487).
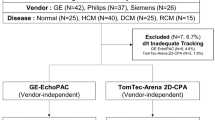
Standard two-dimensional apical four-, three- and two-chamber views, as well as a parasternal mid-papillary short axis view, were acquired independently and in a blinded fashion by two different, experienced echocardiographers in immediate sequence during the same examination, according to the study protocol. Both image sets (acquisition 1 and 2) were analyzed off-line by two independent readers blinded to each other´s results, creating 4 data sets per patient (acquisition 1/reading 1, acquisition 1/reading 2, acquisition 2/reading 1 and acquisition 2/reading 2). In total, 60 acquisitions and 120 analyses were performed; see Fig. 1 for study design. LV end-diastolic volume (EDV), end-systolic volume (ESV) and ejection fraction (EF) were assessed using the biplane Simpson’s method [9]. Mitral annulus plane systolic excursion (MAPSE) was measured by M-mode echocardiography in the apical four chamber view. With the M-mode cursor aligned parallel to the LV walls, the systolic excursion of the mitral annulus was measured from the lowest point at end-diastole to the highest point during systole in the septum and lateral wall, and a mean value was calculated [10].
Study design. Standard echo sequences were acquired independently by two different, echocardiographers. Both image sets (acquisition 1 and 2) were then analyzed by two independent readers creating 4 data sets per patient (acquisition 1/reading 1, acquisition 1/reading 2, acquisition 2/reading 1 and acquisition 2/reading 2). Intra-class Correlation Coefficient (ICC) for single measures was calculated globally for the 4 image sets and then separately for two different acquisitions analyzed by the same reader (inter-acquisition reliability, ICCacq) and two different readers analyzing the same acquisition (inter-reader reliability, ICCread). For estimation of intra-subject variability, the standard deviation of the four measurements of each parameter in each patient was calculated. The mean of these intra-subject standard deviations resulted in the standard error of measurements (SEM) for the whole studied group. The smallest detectable change (SDC) is then calculated as 1.96 × SEM, representing the minimal difference between the measurements that must be overcome to ascertain a true change or difference with a less than 5% chance of error. The smallest relative detectable change (SDCrel) is defined as the ratio of the SDC to the mean value of the measured parameter
All views were obtained at a frame rate of at least 40 frames/s, recording three sequential sinus beats. After choice of the best beat, the endocardial borders were manually traced in the end-diastolic frame for automatic calculation of peak systolic global longitudinal strain (GLS) and circumferential strain (CS), and the resulting region of interest was visually checked for accurate tracking. For GLS calculation, the apical four-, three- and two-chamber views were used, while for CS the mid-ventricular short axis view was traced. We accepted automatic definition of aortic valve closure (AVC) by the software, on the basis of ECG-trigging. Echocardiographic images were acquired with a GE Vivid E9 Ultrasound system. According to recommendations from the American Society of Echocardiography and the European Association of Cardiovascular Imaging we excluded images with suboptimal tracking of the endocardium in more than two segments in one single view or if frame rate was below 40 Hz. Figure 2 presents an example of GLS measurements performed in one of the study patients.
Statistical analysis
For sample size calculation, we assumed that intra-class correlation coefficients (ICC) would be 0.9 and required that the margin of error of a 95% confidence interval (CI) for ICC should be 0.07, i.e., the CI should be the estimated ICC ± 0.07. These conditions indicated a sample size of 30 patients.
Categorical variables were presented as the number of patients and percentages. Continuous variables were presented as mean ± standard deviation (SD). From 2 acquisitions (acquisition 1 and 2) and 2 readings (reading 1 and 2) a total of 4 data values per patient were obtained.
Reliability of measurements was measured in two ways (see Fig. 1):
-
1.
Smallest detectable change (SDC) The square root of the intra-subject variability, which is the standard deviation of the four measurements within patients (standard error of measurements, SEM), was calculated. The SDC was then calculated as 1.96 × SEM, representing the minimal difference between the measurements that must be overcome to ascertain a true change or difference with a less than 5% chance of error. To enable comparison between parameters, the relative smallest detectable change (SDCrel) was defined as the ratio of the SDC to the mean value of the measured parameter.
-
2.
Intra-class correlation coefficient (ICC) for single measures. The ICC is defined as the ratio of the variance between subjects to the total variability which is the sum of between-subject and intra-subject variability. These variance components were estimated in a one-way analysis of variance model with patient as factor. We used Cicchetti’s guidelines for interpretation of ICC values [11].
In order to separate and quantify the impact of acquisition and reading on the reproducibility of measurements, the ICC was calculated separately for two different acquisitions analyzed by the same reader (inter-acquisition reliability, ICCacq) and two different readers analyzing the same acquisition (inter-reader reliability, ICCread); see Fig. 1. The difference between ICCacq and ICCread for all the analyzed parameters was calculated and presented with 95% confidence interval and p value, assessed with jackknife technique.
Furthermore, the mean intra-subject difference between acquisition 1 and 2 after averaging of reading 1 and 2, and the mean difference between reading 1 and 2 after averaging of acquisition 1 and 2, were calculated for all studied parameters, to visualize the effect of acquisition and reading, respectively. Again, the relative mean intra-subject differences were calculated separately for acquisition and reading, by dividing the absolute mean intra-subject difference by the mean value of the respective parameter within the patient, and expressed as percent of the mean within the subject.
For all analyses, two-sided p values < 0.05 were defined as statistically significant. Statistical analyses were performed using SAS Software 9.4. (SAS Institute, Cary, NC, USA) and IBM SPSS version 24 (SPSS, IBM Corporation, Armonk, NY, USA).
Results
Mean age of the study population was 60.6 ± 18.9 years and 63.3% (n = 19) of the patients were males. For baseline characteristics see Table 1. Mean EF was 46.4 ± 16.4%, ranged between 17 and 71% and was impaired (below 52% in males and below 54% in females) in 60% (n = 18) of the patients. For mean values of the studied parameters in total and in separate data sets see Table 2.
The relative smallest detectable change among the conventional echo parameters was lowest for MAPSE (10.7%). Among strain parameters, the relative smallest detectable change was much smaller for GLS than for CS (14.7 and 35.6%, respectively), but similar to the SDCrel observed for volume-derived EF (14.2%). The intra-class correlation coefficient was excellent for all measures of the left ventricular function. For ICCs, their 95% CI, intra-subject SDs and smallest detectable changes, see Table 3.
Intra-patient inter-acquisition reliability (ICCacq) was significantly better than inter-reader reliability (ICCread) only for EF, while no significant difference between those components of test–retest reliability was observed for any other LV function parameter, see Table 4.
Mean intra-subject relative difference (expressed as percent of the mean within the subject) between acquisition 1 and 2 after averaging of reading 1 and 2 for each acquisition (acquisition-effect) and the mean difference between reading 1 and 2 after averaging of acquisition 1 and 2 for each reading (reading-effect) for strain parameters, volume-derived LV function measurements and MAPSE in relation to the mean value of respective parameter within the patient are presented in Fig. 3.
Bland–Altman plots showing the mean intra-subject relative difference (expressed as percent of the mean within the subject) between acquisition 1 and 2 after averaging of reading 1 and 2 for each acquisition (acquisition-effect) and the mean difference between reading 1 and 2 after averaging of acquisition 1 and 2 for each reading (reading-effect) for GLS (a), CS (b), EF (c), EDV (d), ESV (e) and MAPSE (f) versus the mean value of the respective parameter within the patient. Colored lines indicate bias and limits of agreement (1.96 × SD)
With the exception of LV volumes, mean intra-subject standard deviations of EF, MAPSE and GLS did not correlate with their absolute values, indicating that the calculated smallest detectable changes could be shown to be independent (homoscedastic) of LV function impairment level; see Fig. 4.
Correlation between mean intra-subject standard deviations of LV function parameters and their absolute values, indicating that the calculated smallest detectable changes are independent (homoscedastic) of LV function impairment level when assessed by GLS, CS, EF and MAPSE. Intra-subject standard deviations significantly correlated with absolute values of LV volumes
Discussion
In the present study, systematically evaluating components of test–retest reliability in a wide range of left ventricular functions and in a true test–retest clinical setting, we found a reasonable reproducibility for both GLS and conventional measures of left ventricular function. The smallest detectable change of GLS, EF and MAPSE ranged between 11–15% and was not dependent on the grade of LV function impairment. Importantly, GLS measurement did not show higher test–retest reliability than EF. Circumferential strain showed much poorer reproducibility. Repeated recordings had an equal impact on reliability of measurements as repeated readings for all the parameters except for ejection fraction, for which the variability was more dependent on the reader than on the acquisition.
Reproducibility of measurements is pivotal for the clinical application of cardiac imaging, but has received much less attention than accuracy. Measurement data from cardiac imaging, including echocardiography, no matter how accurate, are only meaningful when we can be confident that they are reproducible in other examiners’ hands. However, such measurements inherently and inevitably have considerable measurement variability, which stems from differences in acquisition, in data processing, and in data interpretation, besides the possibility of biological variability of the “true” data, e.g., due to changes in heart rate, blood pressure, or cardiac function itself.
An important component of measurement variability is test–retest reliability (also called reproducibility, repeatability, or robustness), which describes variability of separately acquired and interpreted echocardiographic measurements of the same patient, independent of “true” underlying biological variability. This is the typical clinical scenario for example for follow-up examinations or re-examinations of referred patients. The amount of test–retest reliability must be known in order to decide, with confidence, whether a recorded difference in functional parameters represents a “true” change in cardiac function or just reflects measurement variability.
Echocardiographic measurements of left ventricular function, in particular left ventricular ejection fraction, have been known to involve substantial measurement variability. However, the vast majority of reported “inter-observer” and “intra-observer” variabilities reflect only the variability between different observers reading the same dataset, or of one observer reading the same dataset repeatedly. True test–retest reliability is clinically more meaningful, because it reflects more closely the reality of healthcare, but such data are comparatively scarce.
Reliability of conventional echo parameters of LV function
Variability of conventional echo parameters in a test–retest setting was studied by Otterstad et al. [12], who identified repeated acquisitions as the major component of variability of left ventricular volumes and mass, followed by variability between different readers (inter-observer variability), or between serial readings of the same examination (intra-observer variability). Coefficients of variation due to repeated registrations were 11.6, 7.5 and 12.2% for EDV, ESV and EF, respectively. The smallest detectable change taking into account variation from different readers and repeated readings by the same reader was 16.3, 20.0 and 18.1%, respectively, corresponding with our observations.
Similar test–retest reliability data from early 2D echocardiography were reported by Gordon et al. [13], who showed that the smallest intra-subject detectable change was 15% for EDV, 25% for ESV and 10% for EF. The follow-up acquisitions were however not performed on the same day, so that biologic variability was a possible confounding factor.
Thavendiranathan et al. studied 56 females undergoing chemotherapy at 2 different time points assuming unchanged LV function between measurements evaluated by GLS. The authors reported the smallest detectable change (calculated analogously to our study as 2 × standard error of measurements) of absolute 13% for EF, 59 ml for EDV and 29 ml for ESV [14], which is almost two times higher than in our study. This can probably be explained by expected biological variability between the acquisitions.
Speckle-tracking-derived strain analysis
Less reproducibility data than for volume-based measurements are available for longitudinal strain measurements including GLS. Although intra-observer and inter-observer variability of measurements performed on the same dataset has been assessed in many studies, few data on a true test–retest reliability exist, and these data are largely from patients with normal or near normal left ventricular function [15,16,17,18].
Farsalinos et al. in the largest to date study designed for head-to-head comparison of GLS measurements among seven different vendors, examined a group of 62 volunteers with normal/near normal LV systolic function (average EF 60%) [18]. During the same day the participants were scanned twice by the same echocardiographer and once by another one and the exams were subsequently read, contrary to our study, by the same single physician. Inter-observer relative mean error (mean difference of GLS between acquisitions in percent of mean of absolute measurements), was in average 6.9% for GLS and 10.1% for EF. The parameter “relative mean error” used in Farsalinos’ study analytically corresponds to half the value of the relative SDC (SDCrel) reported in our study, and the results are similar in case of GLS (SDCrel 14.7%, equivalent to “relative mean error” of 7.4% for our study vs. 6.9% in Farsalinos’ study), while the variability of EF is lower (SDCrel 14.2%) in our study, equivalent to “relative mean error” of 7.1% for our study vs. 10.1% in Farsalinos’ study.
Kleijn et al. studied test–retest reliability of both volumetric parameters of LV function and 3 different global strain components, using three-dimensional speckle-tracking echocardiography. In a group of 50 patients with normal or mildly impaired EF, ICC for volume-based parameters was good (0.85 for EF), but only moderate for global strain parameters, however poorer for GLS than for GCS (0.66 and 0.85, respectively) [2]. Calculated absolute SDC for EF was 11% and 5.7% for GLS, almost twice poorer for EF and more than threefold poorer for GLS in our 2D study. The differences can be explained by poorer both spatial and temporal resolution of 3D echo, which makes the use of speckle-tracking-derived deformation parameters limited clinically.
Barbier et al. reported test–retest reliability of strain and volume-based LV function parameters, when the same operator in random order read two image sets recorded during the same examination (not a real test–retest situation) in 40 patients with normal/near normal EF (average EF 52%). The variability of global longitudinal strain was slightly lower for GLS than for EF (coefficient of variation of 5.4% and 6.8%, respectively), which is in the range of our results (calculated from our results the coefficient of variation would be 7.3% and 7.2%, respectively). Interestingly, the measurement variability was higher in the lower range of EF, which is in contrast to our study showing no association between grade of measurement variability and LV impairment [1].
Thorstensen et al., in a group of 10 healthy individuals, evaluated impact of repeated recordings (within 30 min) (inter-observer reproducibility) and analyses (inter-analyzer reproducibility) on variability of LV function parameters [15]. Reported coefficients of repeatability, calculated as 2 x mean intra-subject SD, corresponding with the SDC in current study, were in similar range for EF (7% vs. 6.6% in current study) and GLS (2 strain% vs. 1.7 strain%), and slightly higher for MAPSE (1.6 mm vs. 1.1 mm in current study). They reported an equal impact of repeated acquisitions and readings on the measurement variability of EF and GLS, while for MAPSE repeated acquisitions showed slightly higher impact on measurement variability comparing with repeated readings (mean error of 4% vs. 3%, respectively). Contrary, in the current study only the variability of EF measurements was more dependent on the reader than on acquisition, while both these components to a similar extent influenced the variability of all other measurements of left ventricular function.
Study limitations
Firstly, variability of left ventricular function parameters is strongly influenced by the image quality. In the current study, we included patients with satisfactory quality of the images and with sinus rhythm, therefore the study population is selected. Secondly, the current study was performed using one manufacturer and software. Although only minor, significant inter-manufacturer differences have been described [18, 19], which in practice further compound the problem of test–retest reliability if echo machines or software from different manufacturers are used in different examinations. Thirdly, given the recently disputed accuracy and variability of segmental longitudinal strain [20, 21], as well as a limited size of the study group and its purpose to compare reliability of global systolic function parameters, we address only GLS measurements.
Conclusion
In a test–retest setting, both with normal and impaired left ventricular function, the smallest relative detectable change of EF, GLS and MAPSE was similar (11–15%), but was much higher for CS (35%). Surprisingly, reliability of GLS was not superior to that of EF. Acquisition and reader to a similar extent influenced the variability of measurements of all left ventricular function measures except for ejection fraction, where variability was more dependent on the reader than on the acquisition.
References
Barbier P, Mirea O, Cefalù C, Maltagliati A, Savioli G, Guglielmo M (2015) Reliability and feasibility of longitudinal AFI global and segmental strain compared with 2D left ventricular volumes and ejection fraction: intra- and inter-operator, test–retest, and inter-cycle reproducibility. Eur Heart J Cardiovasc Imaging 16:642–652
Kleijn SA, Aly MF, Terwee CB, van Rossum AC, Kamp O (2012) Reliability of left ventricular volumes and function measurements using three-dimensional speckle tracking echocardiography. Eur Heart J Cardiovasc Imaging 13:159–168
Huttin O, Marie PY, Benichou M, Bozec E, Lemoine S, Mandry D et al (2016) Temporal deformation pattern in acute and late phases of ST-elevation myocardial infarction: incremental value of longitudinal post-systolic strain to assess myocardial viability. Clin Res Cardiol 105:815–826
Tschöpe C, Birner C, Böhm M, Bruder O, Frantz S, Luchner A et al (2018) Heart failure with preserved ejection fraction: current management and future strategies: expert opinion on the behalf of the Nucleus of the “Heart Failure Working Group” of the German Society of Cardiology (DKG). Clin Res Cardiol 107:1–19
Negishi K, Negishi T, Hare JL, Haluska BA, Plana JC, Marwick TH (2013) Independent and incremental value of deformation indices for prediction of trastuzumab-induced cardiotoxicity. J Am Soc Echocardiogr 26:493–498
Tilemann LM, Heckmann MB, Katus HA, Lehmann LH, Müller OJ (2018) Cardio-oncology: conflicting priorities of anticancer treatment and cardiovascular outcome. Clin Res Cardiol 107:271–280
Buckert D, Cieslik M, Tibi R, Radermacher M, Rasche V, Bernhardt P et al (2018) Longitudinal strain assessed by cardiac magnetic resonance correlates to hemodynamic findings in patients with severe aortic stenosis and predicts positive remodeling after transcatheter aortic valve replacement. Clin Res Cardiol 107:20–29
Siepen FAD, Bauer R, Voss A, Hein S, Aurich M, Riffel J et al (2018) Predictors of survival stratification in patients with wild-type cardiac amyloidosis. Clin Res Cardiol 107:158–169
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 28:1–39
Hu K, Liu D, Niemann M, Herrmann S, Gaudron PD, Ertl G et al (2013) Methods for assessment of left ventricular systolic function in technically difficult patients with poor imaging quality. J Am Soc Echocardiogr 26:105–113
Cicchetti DV (1994) Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assess 6:284–290
Otterstad JE, Froeland G, St John Sutton M, Holme I (1997) Accuracy and reproducibility of biplane two-dimensional echocardiographic measurements of left ventricular dimensions and function. Eur Heart J 18:507–513
Gordon EP, Schnittger I, Fitzgerald PJ, Williams P, Popp RL (1983) Reproducibility of left ventricular volumes by two-dimensional echocardiography. J Am Coll Cardiol 2:506–513
Thavendiranathan P, Grant AD, Negishi T, Plana JC, Popović ZB, Marwick TH (2013) Reproducibility of echocardiographic techniques for sequential assessment of left ventricular ejection fraction and volumes: application to patients undergoing cancer chemotherapy. J Am Coll Cardiol 61:77–84
Thorstensen A, Dalen H, Amundsen BH, Aase SA, Stoylen A (2010) Reproducibility in echocardiographic assessment of the left ventricular global and regional function, the HUNT study. Eur J Echocardiogr 11:149–156
Cheng S, Larson MG, McCabe EL, Osypiuk E, Lehman BT, Stanchev P et al (2013) Reproducibility of speckle-tracking-based strain measures of left ventricular function in a community-based study. J Am Soc Echocardiogr 26:1258–1266
Koneru S, Collier P, Goldberg A, Sanghi V, Grimm R, Rodriguez L et al (2016) Temporal variability of global longitudinal strain in stable patients undergoing chemotherapy with trastuzumab. Am J Cardiol 118:930–935
Farsalinos KE, Daraban AM, Ünlü S, Thomas JD, Badano LP, Voigt JU (2015) Head-to-head comparison of global longitudinal strain measurements among nine different vendors: the EACVI/ASE inter-vendor comparison study. J Am Soc Echocardiogr 28:1171–1181
Negishi K, Negishi T, Haluska BA, Hare JL, Plana JC, Marwick TH (2014) Use of speckle strain to assess left ventricular responses to cardiotoxic chemotherapy and cardioprotection. Eur Heart J Cardiovasc Imaging 15:324–331
Mirea O, Pagourelias ED, Duchenne J, Bogaert J, Thomas JD, Badano LP, Voigt JU, EACVI-ASE-Industry Standardization Task Force (2018) Intervendor differences in the accuracy of detecting regional functional abnormalities: a report from the EACVI-ASE strain standardization task force. JACC Cardiovasc Imaging 11:25–34
Mirea O, Pagourelias ED, Duchenne J, Bogaert J, Thomas JD, Badano LP, Voigt JU, EACVI-ASE-Industry Standardization Task Force (2018) Variability and reproducibility of segmental longitudinal strain measurement: a report from the EACVI-ASE strain standardization task force. JACC Cardiovasc Imaging 11:15–24
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares that there is no competing interest.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Baron, T., Berglund, L., Hedin, EM. et al. Test–retest reliability of new and conventional echocardiographic parameters of left ventricular systolic function. Clin Res Cardiol 108, 355–365 (2019). https://doi.org/10.1007/s00392-018-1363-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-018-1363-7