Abstract
Background
Transcatheter aortic valve implantation (TAVI) is a standard therapy for aortic valve stenosis in patients at intermediate-to-high surgical risk. Previously, TAVI at our site was performed by a minimalist heart team (MHT), comprised of two interventional cardiologists, echocardiography staff and two cardiac catheterization laboratory nurses. After revision of German Federal Joint Committee (G-BA) guidelines in September 2015, the presence of an extended heart team (EHT; including a full cardiac surgical team) became mandatory throughout the TAVI procedure. We aimed to evaluate the impact of the EHT on clinical and economical outcomes.
Methods
Data was retrospectively extracted from the medical records of patients receiving an Edwards SAPIEN 3 valve at the University Hospital Tübingen, Germany, between 2014 and 2017 and matched with cost data from the national invoice system of hospitals (InEK). For comparison, patients were grouped according to whether they underwent TAVI with or without the EHT.
Results
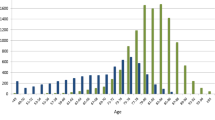
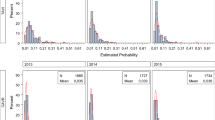
Overall, data for 341 patients (MHT 233; EHT 118) were analysed. Baseline characteristics were largely similar between groups (mean age 81.0 years; 54.5% female), though EHT patients had a lower mean logEuroSCORE (17.5% vs. 19.8%; p = 0.011) and more prior PCI/stenting (39.0% vs. 26.9%; p = 0.022). The rate of immediate procedural death (1.7%) was comparable between groups, as was mortality at 30 days (4.2%). Overall, 1.2% of patients required conversion to surgery. The cost of the index hospitalisation (minus the prosthesis) was higher in the EHT condition (difference + €1604), largely driven by expenditure on physicians (difference + €581; p < 0.001), medical technicians (difference + €372; p < 0.001) and medical supplies (difference +€244; p = 0.001).
Conclusion
At our site, the presence of an EHT throughout the TAVI procedure appears to substantially increase hospital expenditure without significantly improving patient outcomes. We suggest that TAVI by a minimalist HT with a surgical team on call in case of emergency may be sufficient.

Similar content being viewed by others
References
Baumgartner H, Falk V, Bax JJ, De Bonis M, Hamm C, Holm PJ, Iung B, Lancellotti P et al (2017) 2017 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J 38:2739–2791
Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Fleisher LA, Jneid H, Mack MJ et al (2017) 2017 AHA/ACC focused update of the 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 70:252–289
Mollmann H, Bestehorn K, Bestehorn M, Papoutsis K, Fleck E, Ertl G, Kuck KH, Hamm C (2016) In-hospital outcome of transcatheter vs. surgical aortic valve replacement in patients with aortic valve stenosis: complete dataset of patients treated in 2013 in Germany. Clin Res Cardiol 105:553–559
Eggebrecht H, Bestehorn M, Haude M, Schmermund A, Bestehorn K, Voigtländer T, Kuck K-H, Mehta RH (2016) Outcomes of transfemoral transcatheter aortic valve implantation at hospitals with and without on-site cardiac surgery department: insights from the prospective German aortic valve replacement quality assurance registry (AQUA) in 17 919 patients. Eur Heart J 37:2240–2248
Kim WK, Hamm CW (2018) Transcatheter aortic valve implantation in Germany. Clin Res Cardiol 107:81–87
Kiefer P, Seeburger J, Noack T, Schroter T, Linke A, Schuler G, Haensig M, Vollroth M et al (2015) The role of the heart team in complicated transcatheter aortic valve implantation: a 7-year single-centre experience. Eur J Cardiothorac Surg 47:1090–1096
Seiffert M, Conradi L, Baldus S, Schirmer J, Blankenberg S, Reichenspurner H, Diemert P, Treede H (2013) Severe intraprocedural complications after transcatheter aortic valve implantation: calling for a heart team approach. Eur J Cardiothorac Surg 44:478–484; discussion 484
Seidler T, Hunlich M, Puls M, Hasenfuss G, Jacobshagen C (2017) Feasibility and outcomes of interventional treatment for vascular access site complications following transfemoral aortic valve implantation. Clin Res Cardiol 106:183–191
Motloch LJ, Rottlaender D, Reda S, Larbig R, Bruns M, Muller-Ehmsen J, Strauch J, Madershahian N et al (2012) Local versus general anesthesia for transfemoral aortic valve implantation. Clin Res Cardiol 101:45–53
Bundesministerium für Gesundheit (2015) Bekanntmachung eines Beschlusses des Gemeinsamen Bundesausschusses über eine Richtlinie zu minimalinvasiven Herzklappeninterventionen: Erstfassung (Notice of a decision of the Federal Joint Committee on a directive on minimally invasive heart valve interventions: initial version). Bundesministerium für Gesundheit (German Federal Ministry of Health), Berlin
Gemeinsamer Bundesausschuss (2015) Tragende Gründe zum Beschluss des Gemeinsamen Bundesausschusses über eine Richtlinie zu minimalinvasiven Herzklappeninterventionen: Erstfassung (Supporting motives for the decision of the Common Federal Committee about a directive on minimally invasive Valvular interventions: first version). Gemeinsamer Bundesausschuss, Berlin
Kappetein AP, Head SJ, Genereux P, Piazza N, van Mieghem NM, Blackstone EH, Brott TG, Cohen DJ et al (2012) Updated standardized endpoint definitions for transcatheter aortic valve implantation: the Valve Academic Research Consortium-2 consensus document (VARC-2). Eur J Cardiothorac Surg 42:S45–S60
Mehran R, Rao SV, Bhatt DL, Gibson CM, Caixeta A, Eikelboom J, Kaul S, Wiviott SD et al (2011) Standardized bleeding definitions for cardiovascular clinical trials. A consensus report from the Bleeding Academic Research Consortium. Circulation 123:2736–2747
Deutsche Krankenhausgesellschaft (DKG), Spitzenverbände der Krankenkassen (GKV), Verband der privaten Krankenversicherung (PKV) (2016) Kalkulation von Behandlungskosten, Handbuch zur Anwendung in Krankenhäusern, Version 4.0 (Calculation of treatment costs; manual for in-hospital use, version 4.0). Deutsche Krankenhaus Verlagsgesellschaf, Düsseldorf
Wendler O, Schymik G, Treede H, Baumgartner H, Dumonteil N, Neumann F-J, Tarantini G, Zamorano JL et al (2017) SOURCE 3: 1-year outcomes post-transcatheter aortic valve implantation using the latest generation of the balloon-expandable transcatheter heart valve. Eur Heart J 38:2717–2726
Nijhoff F, Abawi M, Agostoni P, Ramjankhan FZ, Doevendans PA, Stella PR (2015) Transcatheter aortic valve implantation with the new balloon-expandable Sapien 3 versus Sapien XT valve system: a propensity score-matched single-center comparison. Circ Cardiovasc Interv 8:e002408
Wendler O, Schymik G, Treede H, Baumgartner H, Dumonteil N, Ihlberg L, Neumann FJ, Tarantini G et al (2017) SOURCE 3 registry: design and 30-day results of the european postapproval registry of the latest generation of the SAPIEN 3 transcatheter heart valve. Circulation 135:1123–1132
Auffret V, Lefevre T, Van Belle E, Eltchaninoff H, Iung B, Koning R, Motreff P, Leprince P et al (2017) Temporal trends in transcatheter aortic valve replacement in France: FRANCE 2 to FRANCE TAVI. J Am Coll Cardiol 70:42–55
Silaschi M, Conradi L, Seiffert M, Schnabel R, Schon G, Blankenberg S, Reichenspurner H, Diemert P et al (2015) Predicting risk in transcatheter aortic valve implantation: comparative analysis of EuroSCORE II and established risk stratification tools. Thorac Cardiovasc Surg 63:472–478
Anand A, Harley C, Visvanathan A, Shah ASV, Cowell J, MacLullich A, Shenkin S, Mills NL (2017) The relationship between preoperative frailty and outcomes following transcatheter aortic valve implantation: a systematic review and meta-analysis. Eur Heart J Qual Care Clin Outcomes 3:123–132
Kotronias RA, Kwok CS, George S, Capodanno D, Ludman PF, Townend JN, Doshi SN, Khogali SS et al (2017) Transcatheter aortic valve implantation with or without percutaneous coronary artery revascularization strategy: a systematic review and meta-analysis. J Am Heart Assoc 6:e005960
Arsalan M, Kim WK, Van Linden A, Liebetrau C, Pollock BD, Filardo G, Renker M, Mollmann H et al (2018) Predictors and outcome of conversion to cardiac surgery during transcatheter aortic valve implantation. Eur J Cardiothorac Surg 54:267–272
Rezq A, Basavarajaiah S, Latib A, Takagi K, Hasegawa T, Figini F, Cioni M, Franco A et al (2012) Incidence, management, and outcomes of cardiac tamponade during transcatheter aortic valve implantation: a single-center study. JACC Cardiovasc Interv 5:1264–1272
Clayton B, Morgan-Hughes G, Roobottom C (2014) Transcatheter aortic valve insertion (TAVI): a review. Br J Radiol 87:20130595
Fernandes P, Cleland A, Bainbridge D, Jones PM, Chu MW, Kiaii B (2015) Development of our TAVI protocol for emergency initiation of cardiopulmonary bypass. Perfusion 30:34–39
Eggebrecht H, Schmermund A, Mehta RH (2014) Reducing severe intraprocedural complications during transcatheter aortic valve implantation with an interdisciplinary heart team approach. Eur J Cardiothorac Surg 45:203–204
Beohar N, Kirtane AJ, Blackstone E, Waksman R, Holmes D Jr, Minha S, Alli O, Suri RM et al (2016) Trends in complications and outcomes of patients undergoing transfemoral transcatheter aortic valve replacement: experience from the PARTNER continued access registry. JACC Cardiovasc Interv 9:355–363
Eggebrecht H, Schmermund A, Kahlert P, Erbel R, Voigtlander T, Mehta RH (2013) Emergent cardiac surgery during transcatheter aortic valve implantation (TAVI): a weighted meta-analysis of 9,251 patients from 46 studies. EuroIntervention 8:1072–1080
Drakopoulou M, Toutouzas K, Stathogiannis K, Latsios G, Synetos A, Oikonomou G, Penesopoulou V, Xanthopoulou M et al (2018) Impact of moderate/severe tricuspid regurgitation on survival of patients undergoing transcatheter aortic valve replacement. J Am College Cardiol 71:A2018
Khawaja MZ, Williams R, Hung J, Arri S, Asrress KN, Bolter K, Wilson K, Young CP et al (2014) Impact of preprocedural mitral regurgitation upon mortality after transcatheter aortic valve implantation (TAVI) for severe aortic stenosis. Heart 100:1799–1803
Acknowledgements
This study was in part funded by the DFG (German Research Foundation) Klinische Forschergruppe 274—Platelets—Molecular Mechanisms and Translational Implications and the Collaborative Research Center Transregio 240. We acknowledge the help of Helen Sims (both Institute for Pharmacology and Preventive Medicine, Cloppenburg, Germany) with the preparation of the manuscript and Lars Knapp (University Hospital Tübingen, Management and Controlling) with collection of InEK data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
MD received travel honoraria by Medtronic; MG has received speaker’s fees from Medtronic and AstraZeneca; TG received restricted grants by Edwards and travel honoraria by Medtronic; PB received consultancy honoraria from Edwards Lifesciences for the preparation of the first draft; OB, TK, RK, HL, CS, CG have nothing to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Droppa, M., Borst, O., Katzenberger, T. et al. Clinical and economical impact of the presence of an extended heart team throughout the balloon-expandable transcatheter aortic valve implantation procedure. Clin Res Cardiol 108, 315–323 (2019). https://doi.org/10.1007/s00392-018-1359-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-018-1359-3