Abstract
Purpose
The anti-anginal efficacy of the selective If inhibitor ivabradine has been demonstrated in controlled clinical trials. However, there is limited information about the safety and efficacy of a combined treatment of ivabradine with beta-blockers, particularly outside of clinical trials in every day practice. This analysis from the REDUCTION study evaluated the safety and efficacy of a combined therapy of beta-blockers and ivabradine in every day practice.
Methods
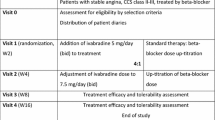
In this multi-center study 4,954 patients with stable angina pectoris were treated with ivabradine in every day routine practice and underwent a clinical follow-up for 4 months. 344 of these patients received a co-medication with beta-blockers. Heart rate (HR), angina pectoris episodes, nitrate consumption, overall efficacy and tolerance were analyzed.
Results
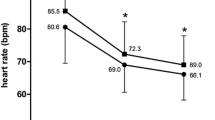
After 4 months of treatment with ivabradine HR was reduced by 12.4 ± 11.6 bpm from 84.3 ± 14.6 to 72.0 ± 9.9 bpm, p < 0.0001. Angina pectoris episodes were reduced from 2.8 ± 3.3 to 0.5 ± 1.3 per week, p < 0.0001. Consumption of short-acting nitrates was reduced from 3.7 ± 5.6 to 0.7 ± 1.7 units per week, p < 0.0001. Five patients (1.5%) reported adverse drug reactions (ADR). The most common ADR were nausea and dizziness (<0.6% each). There was no clinically relevant bradycardia. Efficacy and tolerance were graded as ‘very good/good’ for 96 and 99% of the patients treated.
Conclusion
Ivabradine effectively reduces heart rate and angina pectoris in combination with beta-blockers and is well tolerated by patients in every day practice.



Similar content being viewed by others
References
McLenachan JM, Weidinger FF, Barry J, Yeung A, Nabel EG, Rocco MB, Selwyn AP (1991) Relations between heart rate, ischemia, and drug therapy during daily life in patients with coronary artery disease. Circulation 83:1263–1270
Heusch G, Schulz R (2007) The role of heart rate and the benefits of heart rate reduction in acute myocardial ischemia. Eur Heart J 9(Suppl F):F8–F14
Möhlenkamp S, Lehmann N, Schmermund A, Roggenbuck U, Moebus S, Dragano N, Bauer M, Kälsch H, Hoffmann B, Stang A, Bröcker-Preuss M, Böhm M, Mann K, Jöckel KH, Erbel R, Heinz Nixdorf Recall Study Investigators (2009) Association of exercise capacity and the heart rate profile during exercise stress testing with subclinical coronary atherosclerosis: data from the Heinz Nixdorf Recall Study. Clin Res Cardiol 98(10):665–676
Fox K, Garcia MA, Ardissino D, Buszman P, Camici PG, Crea F, Daly C, De Backer G, Hjemdahl P, Lopez-Sendon J, Marco J, Morais J, Pepper J, Sechtem U, Simoons M, Thygesen K, Priori SG, Blanc JJ, Budaj A, Camm J, Dean V, Deckers J et al (2006) Guidelines on the management of stable angina pectoris. Eur Heart J 27:1341–1381
Fraker TD, Fihn SD (2007) Chronic Angina Focused Update of the ACC/AHA 2002 guidelines for the management of patients with chronic stable angina. Circulation 116:2762–2772
Donner-Banzhoff N, Held K, Laufs U, Trappe HJ, Werdan K, Zerkowski HR. Nationale Versorgungsleitlinie Chronische KHK. Version 2008. http://www.versorgungsleitlinien.de/themen/khk/pdf/nvl_khk_lang.pdf. Accessed 22 January 2009
Kannel WB, Kannel C, Paffenbarger RS Jr, Cupples LA (1987) Heart rate and cardiovascular mortality: the Framingham Study. Am Heart J 113:1489–1494
Palatini P (2007) Heart rate as an independent risk factor for cardiovascular disease. Current evidence and basic mechanisms. Drugs 67(Suppl 2):3–13
Fox K, Borer J, Camm AJ, Danchin N, Ferrari R, Lopez Sendon JL, Steg PG, Tardiff JC, Tavazzi L, Tendera M (2007) Resting heart rate in cardiovascular disease. J Am Coll Cardiol 50:823–830
Fox K, Ford I, Steg PG, Tendera M, Robertson M, Ferrari R (2008) Heart rate as a prognostic risk factor in patients with coronary artery disease and left-ventricular systolic dysfunction (BEAUTIFUL): a subgroup analysis of a randomised controlled trial. Lancet 372(9641):817–821
Fox K, Ford I, Steg PG, Tendera M, Ferrari R, on behalf of the BEAUTIFUL investigators (2008) Ivabradine for patients with stable coronary artery disease and left-ventricular systolic dysfunction (BEAUTIFUL): a randomised, double-blind, placebo-controlled trial. Lancet 372(9641):807–816
DiFrancesco D (2006) Funny channels in the control of cardiac rhythm and mode of action of selective blockers. Pharmacol Res 53:399–406
DiFrancesco D, Camm JA (2004) Heart rate lowering by specific and selective If current inhibition with Ivabradine. Drugs 64:1757–1765
Tardiff JC, Ponikowski P, Kahan T, for the ASSOCIATE study investigators (2009) Efficacy of the If current inhibitor ivabradine in patients with chronic stable angina receiving beta-blocker therapy: a 4 month, randomized, placebo-controlled trial. Eur Heart J 30(5):540–548
Concato J, Shah N, Horwitz RI (2000) Randomized, controlled trials, observational studies, and the hierarchy of research designs. N Engl J Med 342:1887–1892
Pocock SJ, Elbourne DR (2000) Randomized trials or observational tribulations? N Engl J Med 342:1907–1909
Bonzel T, Erbel R, Hamm CW, Levenson B, Neumann FJ, Rupprecht HJ, Zahn R (2008) Percutaneous coronary interventions. Clin Res Cardiol 97(8):513–547
Köster R, Kaehler J, Meinertz T (2009) Treatment of stable angina pectoris by ivabradine in every day practice: the REDUCTION study. Am Heart J 158(4):e51–e57
Campeau L (1976) Grading of angina pectoris. Circulation 54:522–523
Zhang R, Haverich A, Strüber M, Simon A, Pichlmaier M, Bara C (2008) Effects of ivabradine on allograft function and exercise performance in heart transplant recipients with permanent sinus tachycardia. Clin Res Cardiol 97(11):811–819
Gislason GH, Rasmussen JN, Abildstom SZ, Gadsboll N, Buch P, Friberg J, Rasmussen S, Kober L, Stender S, Madsen M, Torp-Pedersen C (2006) Long-term compliance with beta-blockers, angiotensin-converting enzyme inhibitors, and statins after acute myocardial infarction. Eur Heart J 27:1153–1158
Wiest FC, Bryson CL, Burmann M, McDonell MB, Henikoff JG, Fihn SD (2004) Suboptimal pharmacotherapeutic management of chronic stable angina in the primary care setting. Am J Med 117:234–241
Fonarow GC, Abraham WT, Alberrt NM, Stough WG, Gheorghiade M, Greenberg BH, O’Connor CM, Sun JL, Yancy CW, Young JB (2008) Dosing of beta-blocker therapy before, during, and after hospitalization for heart failure (from organized program to initiate lifesaving treatment in hospitalized patients with heart failure) 102:1524–1529
Fox K, Ford I, Steg PG, Tendera M, Robertson M, Ferrari R, on behalf of the BEAUTIFUL investigators (2009) Relationship between ivabradine treatment and cardiovascular outcomes in patients with stable coronary artery disease and left ventricular systolic dysfunction with limiting angina: a subgroup analysis of the randomized, controlled BEAUTIFUL trial. Eur Heart J 30(19):2337–2345
Wenzel P, Abegunewardene N, Münzel T (2009) Effects of selective I f -channel inhibition with ivabradine on hemodynamics in a patient with restrictive cardiomyopathy. Clin Res Cardiol 98(10):681–684
Link A, Reil JC, Selejan S, Böhm M (2009) Effect of ivabradine in dobutamine induced sinus tachycardia in a case of acute heart failure. Clin Res Cardiol 98(8):513–515
Tardiff JC, Ford I, Tendera M, Bourassa MG, Fox K (2005) Efficacy of ivabradine, a new selective If inhibitor, compared with atenolol in patients with chronic stable angina. Eur Heart J 26:2529–2536
Tardiff JC (2007) Clinical results of If current inhibition by ivabradine. Drugs 67(Suppl 2):35–41
Robinson BF (1967) Relation of heart rate and systolic blood pressure to the onset of pain in angina pectoris. Circulation 35:1073–1083
Borer JS, Fox K, Jaillon P, Lerebours G (2003) Antianginal and antiischemic effects of ivabradine, an If inhibitor, in stable angina. A randomized, double-blind, multicentered, placebo-controlled trial. Circulation 107:817–823
Siegel RK (1977) Hallucinations. Sci Am 237:132–140
Acknowledgments
The authors thank Dieter Schremmer from the ‘Gesellschaft für Therapieforschung’ in Munich, Germany, for his substantive support of the statistical analysis, and all investigators for their contributions to the study. The investigators participated were J. Taggeselle, L. Feß, R. Aubele, N. Hassler, K. Hofmann, V. Adelberger, T. Arnold, B. Holz, M. Hwaidi, H.-D. Kombächer, R. Meysing, S. Appel, J. Bazowski, R. Bernauer, H. Böneke, M. Braun, E. Daelmann, M. Deißner, S. Duddy, M.-A. Eisenbarth, H. Fissan, C. Freese, G. Gölz, M. Gutting, K. Hallbaum, M. Hilgedieck, J.-A. Hintze, H. Hohensee, T. Hohenstatt, O. Khan, H.-H. Knäbchen, A. Krämer, K. Krämer, R. Lange, A. Levertov, H. Littwitz, U. Meyer, K. Müller, L. Rokitzki, C. Ruhnau, K. Rybak, R. Schmitt, A. Spingler, H. Stellmach, R. Tietze, W. Türk, R. Vormann, T.-A. Wiegmann, G. Will, E. Wüstenberg, J. Zivojinovic. The list of the further investigators is available from the corresponding author. TM’s, KW’s, HE’s, GS’s and RK’s participation at scientific congresses has been supported by Servier Deutschland. The study was supported by funding from Servier, Germany.
Conflict of interest statement
TM is member of the advisory board. JK has no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
On behalf of the Reduction Study Investigators
Rights and permissions
About this article
Cite this article
Koester, R., Kaehler, J., Ebelt, H. et al. Ivabradine in combination with beta-blocker therapy for the treatment of stable angina pectoris in every day clinical practice. Clin Res Cardiol 99, 665–672 (2010). https://doi.org/10.1007/s00392-010-0172-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-010-0172-4