Abstract
Objective
Our study aimed to analyse the hospital mortality of patients admitted in- and off-regular working hours with ST-elevation myocardial infarction (STEMI) within the special logistical setting of the urban area of the city of Berlin.
Background
There is a debate whether patients with acute myocardial infarction admitted to hospital outside regular working hours experience higher mortality rates than those admitted within regular working hours.
Methods
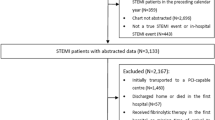
This study analyses data from the Berlin Myocardial Infarction Registry and comprises 2,131 patients with STEMI and treated with percutaneous coronary intervention (PCI) in 2004–2007. Data of patients admitted during in- and off-regular working hours were compared.
Results
There was significant difference in door-to-balloon time (median in-hours: 79 min; median off-hours: 90 min, p < 0.001) and in hospital mortality (in-hours: 4.3%; off-hours: 6.8%, p = 0.020) between STEMI patients admitted in- and off-hours for treatment with PCI. After adjustment, admission off-hours remained an independent predictor for in-hospital death for patients (OR = 2.50; 95% CI 1.38–4.56). In patients with primary care from physician-escorted Emergency Medical Services (EMS), door-to-balloon time was reduced by 10 min for in-hours as well as off-hours patients. The difference in hospital mortality between off-hour and in-hour admission was reduced to a non-significant OR = 1.61 (95% CI 0.79–3.27).
Conclusions
In conclusion, patients admitted off-hours experienced longer door-to-balloon times and higher hospital mortality than did those admitted in-hours. The differences observed between patients admitted in-hours and off-hours were reduced through physician-escorted EMS reflecting the influence of optimized STEMI care.


Similar content being viewed by others

References
Antman EM (2008) Time is muscle: translation into practice. J Am Coll Cardiol 52(15):1216–1221
Kostis WJ, Demissie K, Marcella SW, Shao YH, Wilson AC, Moreyra AE (2007) Weekend versus weekday admission and mortality from myocardial infarction. N Engl J Med 356(11):1099–1109
Magid DJ, Wang Y, Herrin J, McNamara RL, Bradley EH, Curtis JP, Pollack CV Jr, French WJ, Blaney ME, Krumholz HM (2005) Relationship between time of day, day of week, timeliness of reperfusion, and in-hospital mortality for patients with acute ST-segment elevation myocardial infarction. JAMA 294(7):803–812
Peberdy MA, Ornato JP, Larkin GL, Braithwaite RS, Kashner TM, Carey SM, Meaney PA, Cen L, Nadkarni VM, Praestgaard AH, Berg RA (2008) Survival from in-hospital cardiac arrest during nights and weekends. JAMA 299(7):785–792
Jneid H, Fonarow GC, Cannon CP, Palacios IF, Kilic T, Moukarbel GV, Maree AO, Labresh KA, Liang L, Newby LK, Fletcher G, Wexler L, Peterson E (2008) Impact of time of presentation on the care and outcomes of acute myocardial infarction. Circulation 117:2502–2509
Henriques JP, Haasdijk AP, Zijlstra F (2003) Outcome of primary angioplasty for acute myocardial infarction during routine duty hours versus during off-hours. J Am Coll Cardiol 41(12):2138–2142
Mukamal KJ, Muller JE, Maclure M, Sherwood JB, Mittleman MA (2000) Increased risk of congestive heart failure among infarctions with nighttime onset. Am Heart J 140(3):438–442
Spencer FA, Becker RC (2003) Circadian variations in acute myocardial infarction: patients or health care delivery? J Am Coll Cardiol 41(12):2143–2146
Arntz HR, Stern R, Linderer T, Schroder R (1992) Efficiency of a physician-operated mobile intensive care unit for prehospital thrombolysis in acute myocardial infarction. Am J Cardiol 70(4):417–420
Bradley EH, Herrin J, Wang Y, Barton BA, Webster TR, Mattera JA, Roumanis SA, Curtis JP, Nallamothu BK, Magid DJ, McNamara RL, Parkosewich J, Loeb JM, Krumholz HM (2006) Strategies for reducing the door-to-balloon time in acute myocardial infarction. N Engl J Med 355(22):2308–2320
Fukuoka Y, Dracup K, Ohno M, Kobayashi F, Hirayama H (2005) Symptom severity as a predictor of reported differences of prehospital delay between medical records and structured interviews among patients with AMI. Eur J Cardiovasc Nurs 4(2):171–176
Johansson I, Stromberg A, Swahn E (2004) Factors related to delay times in patients with suspected acute myocardial infarction. Heart Lung 33(5):291–300
Jacobs AK, Antman EM, Faxon DP, Gregory T, Solis P (2007) Development of systems of care for ST-elevation myocardial infarction patients: executive summary. Circulation 116(2):217–230
Khot UN, Johnson ML, Ramsey C, Khot MB, Todd R, Shaikh SR, Berg WJ (2007) Emergency department physician activation of the catheterization laboratory and immediate transfer to an immediately available catheterization laboratory reduce door-to-balloon time in ST-elevation myocardial infarction. Circulation 116(1):67–76
Le May MR, So DY, Dionne R, Glover CA, Froeschl MP, Wells GA, Davies RF, Sherrard HL, Maloney J, Marquis JF, O’Brien ER, Trickett J, Poirier P, Ryan SC, Ha A, Joseph PG, Labinaz M (2008) A citywide protocol for primary PCI in ST-segment elevation myocardial infarction. N Engl J Med 358(3):231–240
Redelmeier DA, Bell CM (2007) Weekend worriers. N Engl J Med 356(11):1164–1165
Bradley EH, Curry LA, Webster TR, Mattera JA, Roumanis SA, Radford MJ, McNamara RL, Barton BA, Berg DN, Krumholz HM (2006) Achieving rapid door-to-balloon times: how top hospitals improve complex clinical systems. Circulation 113(8):1079–1085
Bauer T, Hoffmann R, Juenger C, Koeth O, Zahn R, Gitt A, Heer T, Bestehorn K, Senges J, Zeymer U (2009) Efficacy of a 24-h primary percutaneous coronary intervention service on outcome in patients with ST elevation myocardial infarction in clinical practice. Clin Res Cardiol 98(3):171–178
Quaas A, Curzen N, Garratt C (2004) Non-clinical factors influencing the selection of patients with acute coronary syndromes for angiography. Postgrad Med J 80(945):411–414
The Joint European Society of Cardiology/American College of Cardiology Committee (2000) Myocardial infarction redefined-a consensus document of the Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. Eur Heart J 21(18):1502–1513
Holmes DR Jr, Bell MR, Gersh BJ, Rihal CS, Haro LH, Bjerke CM, Lennon RJ, Lim CC, Ting HH (2008) Systems of care to improve timeliness of reperfusion therapy for ST-segment elevation myocardial infarction during off hours: The Mayo clinic STEMI protocol. J Am Coll Cardiol Interv 1(1):88–96
Krueth P, Zeymer U, Gitt A, Juenger C, Wienbergen H, Niedermeier F, Glunz H-G, Senges J, Zahn R (2008) Influence of presentation at the weekend on treatment and outcome on ST-elevation myocardial infarction in hospitals with catheterization laboratories. Clin Res Cardiol 97(10):742–747
Van de Werf F, Ardissino D, Betriu A, Cokkinos DV, Falk E, Fox KA, Julian D, Lengyel M, Neumann FJ, Ruzyllo W, Thygesen C, Underwood SR, Vahanian A, Verheugt FW, Wijns W (2003) Management of acute myocardial infarction in patients presenting with ST-segment elevation. The Task force on the management of acute myocardial infarction of the European society of cardiology. Eur Heart J 24(1):28–66
Mandelzweig L, Battler A, Boyko V, Bueno H, Danchin N, Filippatos G, Gitt A, Hasdai D, Hasin Y, Marrugat J, Van de Werf F, Wallentin L, Behar S (2006) The second Euro Heart Survey on acute coronary syndromes: Characteristics, treatment, and outcome of patients with ACS in Europe and the Mediterranean Basin in 2004. Eur Heart J 27:2285–2293
Schiele F, Meneveau N, Seronde MF, Caulfield F, Fouche R, Lassabe G, Baborier D, Legalery P, Bassand J-P (2005) Compliance with guidelines and 1-year mortality in patients with acute myocardial infarction: a prospective study. Eur Heart J 26:873–880
Maier B, Thimme W, Schoeller R, Fried A, Behrens S, Theres H (2008) Improved therapy and outcome for patients with acute myocardial infarction—data of the Berlin Myocardial Infarction Registry from 1999 to 2004. Int J Cardiol 130:211–219
Zeymer U, Senges J (2003) Why do we need prospective registries in patients with acute myocardial infarction? Eur Heart J 24(18):1611–1612
Alpert JS (2000) Are data from clinical registries of any value? Eur Heart J 21(17):1399–1401
Acknowledgments
The Berlin Myocardial Infarction Registry was supported by unrestricted grants from the participating hospitals, the Technische Universität Berlin; the Senate of the City of Berlin; the Berlin Chamber of Physicians; Freunde und Förderer der Charité e.V. in Berlin, and the companies Boehringer Ingelheim Pharma GmbH & Co. KG (Ingelheim am Rhein), Cordis Medizinische Apparate GmbH (Langenfeld), Lilly Deutschland GmbH (Bad Homburg), MSD Chibropharm GmbH (Haar), Boston Scientific Medizin-Technik GmbH (Ratingen), GlaxoSmithKline GmbH & Co. KG (München). The BMIR is grateful to all the hospitals in which the study was carried out: Charité Universitätsmedizin Berlin, Campus Mitte; Charité Universitätsmedizin Berlin, Campus Virchow; DRK Kliniken Koepenick, Berlin; DRK Kliniken Westend, Berlin; Gemeinschaftskrankenhaus Havelhöhe; Juedisches Krankenhaus; Krankenhaus Lichtenberg; St. Gertrauden-Krankenhaus; Unfallkrankenhaus Berlin; Vivantes Auguste-Viktoria-Klinikum; Vivantes-Humboldt-Klinikum; Vivantes Klinikum Spandau. Their effort and support is very much appreciated.
Conflict of interest statement
No other financial conflicts of interest have been declared by the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
For the Berlin Myocardial Infarction Registry (BMIR).
Rights and permissions
About this article
Cite this article
Maier, B., Behrens, S., Graf-Bothe, C. et al. Time of admission, quality of PCI care, and outcome of patients with ST-elevation myocardial infarction. Clin Res Cardiol 99, 565–572 (2010). https://doi.org/10.1007/s00392-010-0158-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-010-0158-2