Abstract
Objective
Hypercholesterolemia is a common risk factor for cardiovascular diseases; however, there are only few data available on associated costs. The objective of this study is, therefore, to analyse direct and indirect costs in patients with hypercholesterolemia and to determine predictors of costs.
Methods
The ORBITAL Study is a randomised controlled trial evaluating the effectiveness of a compliance-enhancing program in patients with statin therapy. Consecutive patients eligible for statin therapy according to the Joint European Guidelines were enrolled nationwide in 1961 primary care practices in Germany. For the present cost-of-illness analysis, patients were asked retrospectively about medical resource use and employment status in the 6 months preceding enrolment. The perspective chosen was societal. Factors associated with costs were determined using linear regression.
Results
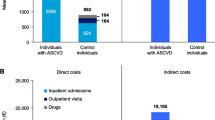
A total of 7,640 patients (56% men, mean age 60 ± 10 years, and 44% women, 64 ± 10 years) were included. Of these patients, 32% were employed, 17% had a history of myocardial infarction, 7% a history of stroke, 58% had hypertension, and 29% diabetes. Total disease-related costs amounted to a mean of 2,498 ± 4,898 Euros per patient over 6 months, comprising direct (44%) and indirect (56%) costs. Disease-related early retirement was responsible for 42% of costs, followed by hospital visits (19%), medication (15%), workdays lost (14%), physician visits (5%), outpatient therapy (2%), and rehabilitation (2%). In multivariable analyses, factors associated with direct costs included coronary interventions, risk stratum, and medical history. Factors associated with indirect costs included disease-related early retirement, other socio-economic and lifestyle factors, coronary interventions, risk stratum, and medical history.
Conclusion
The considerable economic burden associated with hypercholesterolemia indicates the need to assess long-term cost-effectiveness of health care programs in patients with this disorder.

Similar content being viewed by others
References
Anderson KM, Wilson PW, Odell PM, Kannel WB (1991) An updated coronary risk profile. A statement for health professionals. Circulation 83:356–362
Baigent C, Keech A, Kearney PM et al. (2005) Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet 366:1267–1278
Bundesministerium für Gesundheit (2002) Statistisches Taschenbuch Gesundheit 2002. Bundesministerium für Gesundheit, Bonn
Cleemput I, Kesteloot K, DeGeest S (2002) A review of the literature on the economics of noncompliance. Room for methodological improvement. Health Policy 59:65–94
Drummond M (2001) Introducing economic and quality of life measurements into clinical studies. Ann Med 33:344–349
Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) (2001). JAMA 285:2486–2497
Franco OH, Peeters A, Looman CW, Bonneux L (2005) Cost effectiveness of statins in coronary heart disease. J Epidemiol Community Health 59:927–933
Gesundheitsberichterstattung des Bundes (2006) Gesundheit in Deutschland. Robert Koch-Institut, Berlin
Grover SA, Ho V, Lavoie F et al. (2003) The importance of indirect costs in primary cardiovascular disease prevention: can we save lives and money with statins? Arch Intern Med 163:333–339
Hanoverian Consensus-Group (1999) German recommendations for health economic evaluations—revised version of the Hanover Consensus. Gesundh Ökon Qual Manag 4:A62–A65
van Hout BA, Simoons ML (2001) Cost-effectiveness of HMG coenzyme reductase inhibitors; whom to treat? Eur Heart 22:751–761
Johannesson M, Jonsson B, Kjekshus J et al. (1997) Cost effectiveness of simvastatin treatment to lower cholesterol levels in patients with coronary heart disease. Scandinavian Simvastatin Survival Study Group. N Engl J Med 336:332–336
Klever-Deichert G, Hinzpeter B, Wendland G, Lauterbach K (2000) Cost-benefit analysis of an evidence-based secondary prevention of coronary heart diseases by statins. An analysis for Germany from a social security perspective. Med Klin (Munich) 95:305–313
Luley C (2006) Lipometabolic disorder—cholesterol and triglycerides. Clin Res Cardiol 95(suppl):VI17–VI22
MediMedia GmbH (2002) Gelbe Liste Pharmindex (http://www.gelbe-liste.de). MediMedia GmbH, Neu-Isenburg
Mihaylova B, Briggs A, Armitage J et al. (2005) Cost-effectiveness of simvastatin in people at different levels of vascular disease risk: economic analysis of a randomised trial in 20,536 individuals. Lancet 365:1779–1785
Miller PS, Smith DG, Jones P (2005) Cost effectiveness of rosuvastatin in treating patients to low-density lipoprotein cholesterol goals compared with atorvastatin, pravastatin, and simvastatin (a US Analysis of the STELLAR Trial). Am J Cardiol 95:1314–1319
Müller-Nordhorn J, Brüggenjürgen B, Böhmig M et al. (2005) Direct and indirect costs in a prospective cohort of patients with pancreatic cancer. Aliment Pharmacol Ther 22:405–415
Müller-Nordhorn J, Reinhold T, Sonntag F, Wegscheider K, Willich SN (2007) Projected trends in costs of patients with hypercholesterolemia in Germany. E-J Cardiol Practice 6
Murray CJ, Lauer JA, Hutubessy RC et al. (2003) Effectiveness and costs of interventions to lower systolic blood pressure and cholesterol: a global and regional analysis on reduction of cardiovascular-disease risk. Lancet 361:717–725
Neymark N, Adriaenssen I (1999) The costs of managing patients with advanced colorectal cancer in 10 different European centres. Eur J Cancer 35:1789–1795
Prevention of coronary heart disease in clinical practice (1998) Recommendations of the Second Joint Task Force of European and other Societies on coronary prevention. Eur Heart J 19:1434–1503
Prosser LA, Stinnett AA, Goldman PA et al. (2000) Cost-effectiveness of cholesterol-lowering therapies according to selected patient characteristics. Ann Intern Med 132:769–779
Rossnagel K, Nolte CH, Müller-Nordhorn J et al. (2005) Medical resource use and costs of health care after acute stroke in Germany. Eur J Neurol 12:862–868
Ruof J, Huelsemann JL, Mittendorf T et al. (2004) Patient-reported health care utilization in rheumatoid arthritis: what level of detail is required? Arthritis Rheum 51:774–781
Rychlik R (1999) Gesundheitsökonomie - Grundlagen und Praxis. Enke, Stuttgart, pp 15–172
Schwabe U, Pfaff D (2002) Arzneiverordnungsreport 2002. Springer-Verlag, Berlin
Statistisches Bundesamt (2003) Die Bevölkerung Deutschlands bis 2050. 10. koordinierte Bevölkerungsvorausberechnung. Statistisches Bundesamt, Bonn
Strandberg TE, Lehto S, Pyorala K et al. (1997) Cholesterol lowering after participation in the Scandinavian Simvastatin Survival Study (4S) in Finland. Eur Heart J 18:1725–1727
Verband deutscher Rentenversicher ungsträger (VDR) (2003) Durchschnittliche Bruttojahresarbeitsentgelte (http://www.vdr.de/internet/vdr/statzr.nsf/). Verband deutscher Rentenversicherungsträger, Frankfurt am Main
Willich SN, Müller-Nordhorn J, Sonntag F et al. (2004) Economic evaluation of a compliance-enhancing intervention in patients with hypercholesterolemia: design and baseline results of the Open Label Primary Care Study: rosuvastatin based compliance initiatives to achievements of LDL goals (ORBITAL) study. Am Heart J 148:1060–1067
Willich SN, Reinhold T, Lenz C, Brüggenjürgen B (2005) Herzinsuffizienz nach Myokardinfarkt in Deutschland – Ökonomische Bedeutung und Einschränkung der Lebensqualität. Pharmacoecon – German Res Art 3:25–39
Willich SN, Nocon M, Kulig M et al. (2006) Cost-of-disease analysis in patients with gastro-oesophageal reflux disease and Barrett’s mucosa. Aliment Pharmacol Ther 23:371–376
World Health Organization (2003) The World Health Report 2002. Reducing risks, promoting healthy life. World Health Organization, Geneva
Zentralinstitut für die kassenärztliche Versorgung in der BRD (2002) Die 50 häufigsten Diagnosen von Patienten, Kontakthäufigkeit und angeforderter Leistungsbedarf in Punkten. Zentralinstitut für kassenärztliche Versorgung, Köln
Zhou XH, Melfi CA, Hui SL (1997) Methods for comparison of cost data. Ann Intern Med 127:752–756
Acknowledgments
We would like to thank all participating investigators and patients for their cooperation. Ines Ziese, Verena Wölfert and Ulrike Stasun performed an excellent job with regard to study coordination and data management. The study was supported by a grant from AstraZeneca. Prof. Dr. Wegscheider had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Author information
Authors and Affiliations
Corresponding author
Additional information
ClinicalTrials.gov Identifier: NCT00379249.
Rights and permissions
About this article
Cite this article
Müller-Nordhorn, J., Englert, H., Wegscheider, K. et al. Productivity loss as a major component of disease-related costs in patients with hypercholesterolemia in Germany. Clin Res Cardiol 97, 152–159 (2008). https://doi.org/10.1007/s00392-007-0602-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-007-0602-0