Summary
Background
Evaluating myocardial function, assessing ischemic myocardial areas and detecting myocardial viability are necessary diagnostic information for guiding further therapy in patients with angina. The aim of this study was to show feasibility and safety of a compiled contrast- enhanced magnetic resonance imaging (ceMRI) protocol providing the above mentioned diagnostic possibilities and to demonstrate its applicability in daily routine.
Methods
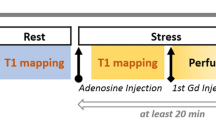
Consecutive patients with angina were screened on a 1.5 Tesla system. Functional images in short and long axis orientation were acquired for each patient. First-pass kinetics of a gadolinium-based contrast agent (0.1 mmol/kg) were measured after three minutes of stress with adenosine infusion (140μg/kg/min). 10 min after a second bolus injection of contrast agent “late enhancement” (MLE) sequences were acquired for the detection of myocardial necrosis.
Results
We enrolled 3174 patients referred for ceMRI for detection or exclusion of ischemic heart disease. One patient experienced a major complication due to hyperventilation followed by grand mal seizure. In 1121 (35.3%) patients minor complications, such as mild chest pain or dyspnea (30%), temporarily and asymptomatic AV block (3%) or nausea (2%) could be observed under adenosine infusion. Hypoperfusion in more than one myocardial segment and affecting more than 1/3 of the myocardial wall diameter could be detected in 1972 (62%) patients. Subendocardial hypoperfusion with limited duration could be shown in 897 (28%) patients. In 305 (10%) patients hypoperfusion could be excluded. MLE could be seen in 532 (17%) patients.
Conclusion
This compiled ceMRI protocol is suitable for detection or exclusion of ischemic heart disease in an outpatient routine. We showed feasibility, applicability and safety of our protocol. CeMRI may serve as a useful surrogate for non-invasive diagnostics prior to invasive coronary angiography in many outpatients.
Similar content being viewed by others
References
Al–Saadi N, Gross M, Bornstedt A, Schnackenburg B, Klein C, Fleck E, Nagel E (2001) Comparison of various parameters for determining an index of myocardial perfusion reserve in detecting coronary stenosis with cardiovascular magnetic resonance tomography. Z Kardiol 90:824–834
Ansari M, Araoz PA, Gerard SK, Watzinger N, Lund GK, Massie BM, Higins CB, Saloner DA (2004) Comparison of late enhancement cardiovascular magnetic resonance and thallium SPECT in patients with coronary disease and left ventricular dysfunction. J Cardiovasc Magn Reson 6:549–556
Bellenger NG, Francis JM, Davies CL, Coats AJ, Pennell DJ (2000) Establishment and performance of a magnetic resonance cardiac function clinic. J Cardiovasc Magn Reson 2:15–22
Bernhardt P, Engels T, Levenson B, Haase K, Albrecht A, Strohm O (2006) Prediction of necessity for coronary artery revascularization by adenosine contrast–enhanced magnetic resonance imaging. Int J Cardiol; in press
Cannon RO III, Epstein SE (1988) “Microvascular angina” as a cause of chest pain with angiographically normal coronary arteries. Am J Cardiol 61:1338–1343
Cannon RO III. Watson RM, Rosing DR, Epstein SE (1983) Angina caused by reduced vasodilator reserve of the small coronary arteries. J Am Coll Cardiol 1:1359–1373
Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, Pennell DJ, Rumberger JA, Ryan T, Verani MS (2002) Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart: a statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation 105:539–542
Chiu CW, So NM, Lam WW, Chan KY, Sanderson JE (2003) Combined first–pass perfusion and viability study at MR imaging in patients with non–ST segment–elevation acute coronary syndromes: feasibility study. Radiology 226:717–722
Friedrich MG, Schulz–Menger J, Strohm O, Dick AJ, Dietz R (2000) The diagnostic impact of 2D– versus 3D– left ventricular volumetry by MRI in patients with suspected heart failure. MAGMA 11:16–19
Grebe O, Kestler HA, Merkle N, Wohrle J, Kochs M, Hoher M, Hombach V (2004) Assessment of left ventricular function with steady–statefree– precession magnetic resonance imaging. Reference values and a comparison to left ventriculography. Z Kardiol 93:686–695
Grebe O, Paetsch I, Kestler HA, Herkommer B, Schnackenburg B, Hombach V, Fleck E, Nagel E (2003) Optimal acquisition parameters for contrast enhanced magnetic resonance imaging after chronic myocardial infarction. J Cardiovasc Magn Reson 5:575–587
Horstick G, Petersen SE, Voigtländer T, Mohrs OK, Schreiber WG (2005) Cardio–MRT. The multimodal functional analysis of the future. Z Kardiol 93 Suppl 4:IV36–47
Ishida N, Sakuma H, Motoyasu M, Okinaka T, Isaka N, Nakano T, Takeda K (2003) Noninfarcted myocardium: correlation between dynamic first–pass contrast–enhanced myocardial MR imaging and quantitative coronary angiography. Radiology 229:209–216
Kaski JC, Aldama G, Cosin–Sales J (2004) Cardiac syndrome X. Diagnosis, pathogenesis and management. Am J Cardiovasc Drugs 4:179–194
Keijer JT, van Rossum AC, Wilke N, van Eenige MJ, Jerosch–Herold M, Bronzwaer JG, Visser CA (2000) Magnetic resonance imaging of myocardial perfusion in single–vessel coronary artery disease: implications for transmural assessment of myocardial perfusion. J Cardiovasc Magn Reson 2:189–200
Kim RJ, Fieno DS, Parish TB, Harris K, Chen EL, Simonetti O, Bundy J, Finn JP, Klocke FJ, Judd RM (1999) Relationship of MRI delayed contrast enhancement to irreversible injury, infarct age, and contractile function. Circulation 100:1992–2002
Kitagwa K, Sakuma H, Hirano T, Okamoto S, Makino K, Takeda K (2003) Acute myocardial infarction: myocardial viability assessment in patients early thereafter – comparison of contrast–enhanced MR imaging with resting 201T1 SPECT1. Radiology 226:138–144
Klein C, Nekolla SG, Bengel FM, Momose M, Sammer A, Haas F, Schnackenburg B, Delius W, Mudra H, Wolfram D, Schwaiger M (2002) Assessment of myocardial viability with contrast–enhanced magnetic resonance imaging: comparison with positron emission tomography. Circulation 105:162–167
Knuesel PR, Nanz D, Wyss C, Buechi M, Kaufmann PA, von Schulthess GK, Lüscher TF, Schwitter J (2003) Characterization of dysfunctional myocardium by positron emission tomography and magnetic resonance: relation to functional outcome after revascularization. Circulation 108:1095–1100
Kramer CM, Rogers WJ, Mankad S, Theobald TM, Pakstis DL, Hu YL (2000) Contractile reserve and contrast uptake pattern by magnetic resonance imaging and functional recovery after reperfused myocardial infarction. J Am Coll Cardiol 36: 1835–1840
Maseri A, Crea F, Kasaki JC, Crake T (1991) Mechanisms of angina pectoris in syndrome X. J Am Coll Cardiol 17:499–506
Noguchi Y, Nagata–Kobayashi S, Stahl JE, Wong JB (2005) A meta–analytic comparison of echocardiographic stressors. Int J Cardiovasc Imaging 21:189–207
Panting JR, Gatehouse PD, Yang GZ, Grothues F, Firmin DN, Collins P, Pennell DJ (2002) Abnormal subendocardial perfusion in cardiac syndrome X detected by cardiovascular magnetic resonance imaging. N Engl J Med 346:1948–1953
Petersen SE, Mohrs OK, Horstick G, Oberholzer K, Abegunewardene N, Ruetzel K, Selvanayagam JB, Robson MD, Neubauer S, Thelen M, Meyer J, Kreitner KF (2004) Influence of contrast agent dose and image acquisition timing on the quantitative determination of nonviable myocardial tissue using delayed contrast–enhanced magnetic resonance imaging. J Cardiovasc Magn Reson 6:541–548
Rehwald WG, Fieno DS, Chen EL, Kim RJ, Judd RM (2002) Myocardial magnetic resonance imaging contrast agent concentrations after reversible and irreversible ischemic injury. Circulation 105:224–229
Schwitter J, Nanz D, Kneifel S, Bertschinger K, Buchi M, Knusel PR, Marincek B, Luscher TF, von Schulthess GK (2001) Perfusion in coronary artery disease by magnetic resonance: a comparison with positron emission tomography and coronary angiography. Circulation 103:2230–2235
Wagner A, Marholdt H, Holly TA, Elliott MD, Regenfus M, Parker M, Klocke FJ, Bonow RO, Kim RJ, Judd RM (2003) Contrast–enhanced MRI and routine single photon emission computed tomography (SPECT) perfusion imaging for detection of subendocardial myocardial infarcts: an imaging study. Lancet 361:374–379
Wu E, Judd RM, Vargas JD, Klocke FJ, Bonow RO, Kim RJ (2001) Visualisation of presence, location, and transmural extent of healed Q–wave and non–Q–wave myocardial infarction. Lancet 357:21–28
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bernhardt, P., Levenson, B., Engels, T. et al. Contrast-enhanced adenosine-stress magnetic resonance imaging. Clin Res Cardiol 95, 461–467 (2006). https://doi.org/10.1007/s00392-006-0410-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-006-0410-y