Abstract
Background
Personal autonomy in advanced age critically depends on mobility in the environment. Geriatric patients are often not able to walk safely with sufficient velocity. In many cases, multiple factors contribute to the deficit. Diagnostic identification of single components enables a specific treatment.
Objective
This article describes the most common neurological causes of imbalance and impaired gait that are relevant for a pragmatic approach for the assessment of deficits in clinical and natural environments taking into account the physiology of balance and gait control, typical morbidities in older people and the potential of innovative assessment technologies.
Material and methods
Expert opinion based on a narrative review of the literature and with reference to selected research topics.
Results and discussion
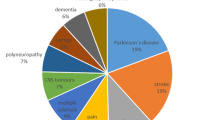
Common neurological causes of impaired balance and mobility are sensory deficits (reduced vision, peripheral neuropathy, vestibulopathy), neurodegeneration in disorders with an impact on movement control and motoric functions (Parkinsonian syndromes, cerebellar ataxia, vascular encephalopathy) and functional (psychogenic) disorders, particularly a fear of falling. Clinical tests and scores in laboratory environments are complemented by the assessment in the natural environment. Wearable sensors, mobile smartphone-based assessment of symptoms and functions and adopted strategies for analysis are currently emerging. Use of these data enables a personalized treatment. Furthermore, sensor-based assessment ensures that effects are measured objectively.
Zusammenfassung
Hintergrund
Der Erhalt der Autonomie im Alter hängt wesentlich von den Möglichkeiten der selbstbestimmten Mobilität in der jeweiligen Lebensumgebung ab. Die Fähigkeit, mit ausreichender Geschwindigkeit und Sicherheit zu gehen, ist bei geriatrischen Patienten oft beeinträchtigt, und mehrere Faktoren tragen zu dieser Einschränkung bei. Die Komponentendiagnostik alltagsrelevanter Defizite erlaubt eine spezifische Behandlung.
Ziel der Arbeit
Auf Basis der Kenntnis der Physiologie der Gleichgewichtserhaltung und der typischen Morbidität älterer Menschen, sowie den aktuellen Innovationen im Bereich der diagnostischen Technologien wird ein pragmatisches Vorgehen bei der Erfassung von Mobilitätsdefiziten in Klinik und Alltagsumgebung vorgeschlagen.
Material und Methoden
Expertenmeinung mit Recherche und Einbeziehung von Literatur und Forschungsthemen.
Ergebnisse und Diskussion
Besonders häufige neurologische Komponenten der Störung von Mobilität und Gleichgewicht sind sensorische Defizite (Visusminderung, Polyneuropathie, Vestibulopathie), neurodegenerative Erkrankungen mit Auswirkungen auf Bewegungskontrolle und motorische Funktion (Parkinson-Syndrome, Kleinhirnataxie, vaskuläre Enzephalopathie) sowie die funktionellen (psychischen) Komponenten, insbesondere die Angst zu stürzen. Zur Erweiterung der Untersuchung in Klinik und Praxis ist das Erfassen von Einschränkungen in der Alltagsumgebung wichtig. Tragbare Sensoren und mobile, Smartphone-basierte Symptom- und Funktionserfassung, sowie digital unterstützte Auswertungsstrategien werden derzeit entwickelt. Die Therapie kann damit auf die alltagsrelevanten Einschränkungen zugeschnitten und objektiv bewertet werden.


Similar content being viewed by others
References
Agrawal Y, Carey JP, Santina DCC et al (2009) Disorders of balance and vestibular function in US adults: data from the National Health and Nutrition Examination Survey, 2001–2004. Arch Intern Med 169:938–944
Ambrose AF, Noone ML, Pradeep VG et al (2010) Gait and cognition in older adults: insights from the Bronx and Kerala. Ann Indian Acad Neurol 13:99–103
Arber S (2017) Organization and function of neuronal circuits controlling movement. EMBO Mol Med 9:281–284
Bachor E, Wright CG, Karmody CS (2002) The incidence and distribution of cupular deposits in the pediatric vestibular labyrinth. Laryngoscope 112:147–151
Beauchet O, Allali G, Thiery S et al (2011) Association between high variability of gait speed and mild cognitive impairment: a cross-sectional pilot study. J Am Geriatr Soc 59:1973–1974
Bergmann J, Kreuzpointner MA, Krewer C et al (2015) The subjective postural vertical in standing: reliability and normative data for healthy subjects. Atten Percept Psychophys 77:953–960
Bohnen NI, Jahn K (2013) Imaging: What can it tell us about parkinsonian gait? Mov Disord 28:1492–1500
Bridenbaugh SA, Kressig RW (2015) Motor cognitive dual tasking: early detection of gait impairment, fall risk and cognitive decline. Z Gerontol Geriatr 48:15–21
Dieterich M, Brandt T (2008) Functional brain imaging of peripheral and central vestibular disorders. Brain 131:2538–2552
Eskofier EM, Sunghoohn IL, Baron M et al (2017) An overview of smart shoes in the internet of health things: gait and mobility assessment in health promotion and disease monitoring. Appl Sci (Basel) 7:986–1002
Espay AJ, Bonato P, Nahab FB et al (2016) Technology in Parkinson’s disease: challenges and opportunities. Mov Disord 31:1272–1282
Freiberger E (2018) Cognition and mobility : the influence of the brain on gait. Internist 59:316–325
Fritz S, Lusardi M (2009) White paper: “walking speed: the sixth vital sign”. J Geriatr Phys Ther 32:46–49
Furman JM, Raz Y, Whitney SL (2010) Geriatric vestibulopathy assessment and management. Curr Opin Otolaryngol Head Neck Surg 18:386–391
Gassner H, Marxreiter F, Steib S et al (2017) Gait and cognition in Parkinson’s disease: cognitive impairment is inadequately reflected by gait performance during dual task. Front Neurol 8:550
Grillner S (1981) Control of locomotion in bipeds, tetrapods and fish. In: Brooks VB (ed) Motor control, part 2. Handbook of physiology, the nervous system, vol II. American Physiological Society, Bethesda, MD, pp 1179–1236
Grillner S, Wallen P (1985) Central pattern generators for locomotion, with special reference to vertebrates. Annu Rev Neurosci 8:233–261
Herdman SJ (2013) Vestibular rehabilitation. Curr Opin Neurol 26:96–101
Jacobs AH, Bollheimer C (2019) Frailty. In: Maetzler WDR, Jacobs AH (eds) Neurogeriatrie: ICF-basierte Diagnose und Behandlung. Springer, Berlin, pp 49–68
Jahn K, Deutschlander A, Stephan T et al (2008) Imaging human supraspinal locomotor centers in brainstem and cerebellum. Neuroimage 39:786–792
Jahn K, Deutschländer A, Stephan T et al (2004) Brain activation patterns during imagined stance and locomotion in functional magnetic resonance imaging. Neuroimage 22:1722–1731
Jahn K, Kressig RW, Bridenbaugh SA et al (2015) Dizziness and unstable gait in old age: etiology, diagnosis and treatment. Dtsch Arztebl Int 112:387–393
Jahn K, Naessl A, Schneider E et al (2003) Inverse U‑shaped curve for age dependency of torsional eye movement responses to galvanic vestibular stimulation. Brain 126:1579–1589
Jahn K, Saul AK, Elstner M et al (2018) Vestibular rehabilitation therapy and Nintendo Wii balance board training both improve postural control in bilateral vestibulopathy. J Neurol 265:70–73
Jahn K, Zwergal A, Schniepp R (2010) Gait disturbances in old age: classification, diagnosis, and treatment from a neurological perspective. Dtsch Arztebl Int 107:306–315
Jonsson R, Sixt E, Landahl S et al (2004) Prevalence of dizziness and vertigo in an urban elderly population. J Vestib Res 14:47–52
Kumar A, Delbaere K, Zijlstra GA et al (2016) Exercise for reducing fear of falling in older people living in the community: Cochrane systematic review and meta-analysis. Age Ageing 45:345–352
Lopez I, Honrubia V, Baloh RW (1997) Aging and the human vestibular nucleus. J Vestib Res 7:77–85
Mueller M, Strobl R, Jahn K et al (2014) Impact of vertigo and dizziness on self-perceived participation and autonomy in older adults: results from the KORA-Age study. Qual Life Res 23:2301–2308
Mueller M, Strobl R, Jahn K et al (2014) Burden of disability attributable to vertigo and dizziness in the aged: results from the KORA-Age study. Eur J Public Health 24:802–807
Payette MC, Belanger C, Leveille V et al (2016) Fall-related psychological concerns and anxiety among community-dwelling older adults: systematic review and meta-analysis. PlosOne 11:e152848
Peterka RJ, Black FO, Schoenhoff MB (1990) Age-related changes in human vestibulo-ocular reflexes: sinusoidal rotation and caloric tests. J Vestib Res 1:49–59
Reelick MF, Van Iersel MB, Kessels RP et al (2009) The influence of fear of falling on gait and balance in older people. Age Ageing 38:435–440
Richter E (1980) Quantitative study of human Scarpa’s ganglion and vestibular sensory epithelia. Acta Otolaryngol 90:199–208
Rosenhall U (1973) Degenerative patterns in the aging human vestibular neuro-epithelia. Acta Otolaryngol 76:208–220
Schniepp R, Boerner JC, Decker J et al (2018) Noisy vestibular stimulation improves vestibulospinal function in patients with bilateral vestibulopathy. J Neurol 265:57–62
Schniepp R, Wuehr M, Neuhaeusser M et al (2012) Locomotion speed determines gait variability in cerebellar ataxia and vestibular failure. Mov Disord 27:125–131
Schulein S, Barth J, Rampp A et al (2017) Instrumented gait analysis: a measure of gait improvement by a wheeled walker in hospitalized geriatric patients. J Neuroeng Rehabil 14:18
Schwenk M, Zieschang T, Oster P, Hauer K (2010) Dual-task performance can be improved in patients with dementia. A randomized controlled trial. Baillieres Clin Neurol 74:1961–1968
Selge C, Schoeberl F, Zwergal A et al (2018) Gait analysis in PSP and NPH: Dual-task conditions make the difference. Baillieres Clin Neurol 90:e1021–e1028
Sloane PD, Baloh RW, Honrubia V (1989) The vestibular system in the elderly: clinical implications. Am J Otolaryngol 10:422–429
Snijders AH, Van De Warrenburg BP, Giladi N et al (2007) Neurological gait disorders in elderly people: clinical approach and classification. Lancet Neurol 6:63–74
Steinhubl SR, Muse ED, Topol EJ (2015) The emerging field of mobile health. Sci Transl Med 7:283rv283
Studenski S, Perera S, Patel K et al (2011) Gait speed and survival in older adults. JAMA 305:50–58
Szmulewicz DJ, Waterston JA, Halmagyi GM et al (2011) Sensory neuropathy as part of the cerebellar ataxia neuropathy vestibular areflexia syndrome. Baillieres Clin Neurol 76:1903–1910
Todd C, Skelton D (2004) What are the main risk factors for falls among older people and what are the most effecxtive interventions to prevent these falls? WROfE, Copenhagen
Topol EJ, Steinhubl SR, Torkamani A (2015) Digital medical tools and sensors. JAMA 313:353–354
Van Haastregt JC, Zijlstra GA, Van Rossum E et al (2008) Feelings of anxiety and symptoms of depression in community-living older persons who avoid activity for fear of falling. Am J Geriatr Psychiatry 16:186–193
Velazquez-Villasenor L, Merchant SN, Tsuji K et al (2000) Temporal bone studies of hte human peripheral vestibular system. Normative Scarpa’s ganglion cell data. Ann Otol Rhinol Laryngol Suppl 181:14–19
Verghese J, Annweiler C, Ayers E et al (2014) Motoric cognitive risk syndrome: multicountry prevalence and dementia risk. Baillieres Clin Neurol 83:718–726
Verghese J, Wang C, Lipton RB et al (2013) Motoric cognitive risk syndrome and the risk of dementia. J Gerontol 68:412–418
Verghese J, Wang C, Lipton RB et al (2007) Quantitative gait dysfunction and risk of cognitive decline and dementia. J Neurol Neurosurg Psychiatry 78:929–935
Wuehr M, Schniepp R, Ilmberger J et al (2013) Speed-dependent temporospatial gait variability and long-range correlations in cerebellar ataxia. Gait Posture 37:214–218
Zingler VC, Cnyrim C, Jahn K et al (2007) Causative factors and epidemiology of bilateral vestibulopathy in 255 patients. Ann Neurol 61:524–532
Zwergal A, Linn J, Xiong G et al (2012) Aging of human supraspinal locomotor and postural control in fMRI. Neurobiol Aging 33:1073–1084
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
K. Jahn, E. Freiberger, B.M. Eskofier, C. Bollheimer and J. Klucken declare that they have no competing interests.
For this article no studies with human participants or animals were performed by any of the authors. All studies performed were in accordance with the ethical standards indicated in each case.
Rights and permissions
About this article
Cite this article
Jahn, K., Freiberger, E., Eskofier, B.M. et al. Balance and mobility in geriatric patients. Z Gerontol Geriat 52, 316–323 (2019). https://doi.org/10.1007/s00391-019-01561-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00391-019-01561-z