Abstract
Background
Health care utilisation (HCU) can be a useful outcome for estimating costs and patient needs. It can also be used as a surrogate parameter for healthy ageing. The aim of this study was to analyse the associations of formerly described and potentially new parameters influencing health care utilisation in older adults in Germany.
Patients and methods
The ActiFE Ulm (Activity and Function in the Elderly in Ulm) study is a population-based study in 1,506 community dwelling older adults aged 65–90 years in Ulm and surrounding areas in southwestern Germany. Between March 2009 and April 2010 a full geriatric assessment was performed including accelerometer-based average daily walking duration, comorbidity, medication, physical and psychological functioning, health care utilisation, sociodemographic factors etc. The association between above named measures and health care utilisation, represented by the number of drugs, the days in hospital and the number of physician contacts over one year was calculated in multiple regression models. Analysis was conducted among subjects with complete information (n = 1,059, mean age 76 years, 55% male).
Results
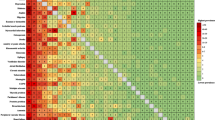
The average number of drugs was 4.5 and over 95% of participants visited a physician at least once a year while still more than 65% contacted their physician more than twice a year. Reduced physical activity, BMI, self-rated health and/or comorbidity and male sex were the best predictors of health care utilisation in community dwelling older adults when looking at both the number of drugs and the number of physician contacts over 12 months together. With regard to single diseases entities the best predictors of both the number of drugs and the number of physician contacts were asthma, chronic obstructive pulmonary disease (COPD)/chronic bronchitis and chronic neurological diseases (mostly Parkinson’s disease). The number of drugs was most strongly associated with coronary heart disease, diabetes, and high blood pressure.
Conclusion
Reduced walking activity, self-rated health and/or comorbidity and male sex are the best predictors of health care utilisation as measured by the number of drugs and number of physician contacts over 12 months. Walking activity could be regarded as the most promising modifiable predictor of HCU in older adults.
Zusammenfassung
Hintergrund
Die Erfassung einer Inanspruchnahme des Gesundheitswesens kann zur Kostenabschätzung nützlich sein und einen Eindruck vermitteln, welche Erkrankungen Patienten am meisten beeinträchtigen. Somit kann es auch als Surrogat für gesundes Altern verwendet werden. In dieser Analyse sollten die Zusammenhänge bereits bekannter und möglicher neuer Faktoren mit der Inanspruchnahme des Gesundheitswesens bei älteren Menschen in Deutschland beschrieben werden.
Patienten und Methoden
Die Studie ActiFE Ulm (Activity and Function in the Elderly in Ulm) ist eine populationsbasierte Studie bei 1506 zu Hause lebenden Personen zwischen 65 und 90 Jahren, die in der Stadt Ulm und Umgebung wohnen. Zwischen März 2009 und April 2010 wurde ein komplettes geriatrisches Assessment durchgeführt. Darunter waren u. a. eine akzelerometerbasierte Aktivitätsmessung, Assessments der Komorbidität, der Medikation, der physischen und psychischen Funktionen, soziodemographische und zahlreiche weitere Faktoren. Die Zusammenhänge zwischen den oben genannten Parametern und der Inanspruchnahme des Gesundheitswesens, dargestellt durch die Zahl der Medikamente, die stationären Tage im Krankenhaus und die Zahl der Arztbesuche in einem Jahr, wurden mittels multipler Regression (verschiedene Modelle) berechnet. Von 1059 Teilnehmern konnten komplette Daten ausgewertet werden (Alter im Mittel 76 Jahre, 55% Männer).
Ergebnisse
Die mittlere Anzahl an Medikamenten lag bei 4,5, und über 95% der Teilnehmer hatten im letzten Jahr mindestens einmal einen Arzt aufgesucht, mehr als 65% sogar dreimal und öfter. Eine reduzierte körperliche Aktivität, der Body-Mass-Index, die Selbsteinschätzung der Gesundheit und die Komorbidität sowie männliches Geschlecht waren die besten Prädiktoren der Inanspruchnahme des Gesundheitswesens, wenn man die beiden Endpunkte, die Zahl der Medikamente und die Arztbesuche zusammen betrachtet. Bei der Analyse einzelner Krankheitsbilder waren Asthma, COPD/chronische Bronchitis und chronische neurologische Erkrankungen führend. Bei alleiniger Betrachtung der Medikamentenzahl als Endpunkt zeigten KHK, Diabetes, hoher Blutdruck und andere, vor allem kardiologische Krankheitsbilder die stärkste Assoziation. Krankenhausaufenthalte waren nur mit der Anzahl der Medikamente signifikant korreliert.
Schlussfolgerung
Reduzierte körperliche Aktivität, Selbsteinschätzung der Gesundheit, Komorbidität sowie das männliche Geschlecht sind die besten Prädiktoren für die Inanspruchnahme des Gesundheitswesens. Die körperliche Aktivität kann aus Sicht der Prävention und des gesunden Alterns als interessantester modifizierbarer Parameter angesehen werden.
Similar content being viewed by others
References
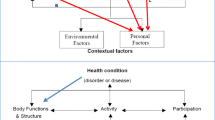
Andersen R (1973) Societal and individual determinants of medical care utilization in the United States. Milbank Mem Fund Q Health Soc 51:95
Antonicelli, L, Bucca C, Neri M et al (2004) Asthma severity and medical resource utilisation. Eur Respir J 23:723–729
Blair SN (2006) Objectively measured physical activity and mortality in older adults. JAMA 296:216–218
Braune BT, Berger K (2005) The influence of depressive mood on activities of daily living and health care utilization in the elderly–the MEMO study on the KORA platform Augsburg. Gesundheitswesen 67(Suppl 1):S176–S179
Bustacchini S, Chiatti C, Furneri G et al (2011) The economic burden of chronic obstructive pulmonary disease in the elderly: results from a systematic review of the literature. Curr Opin Pulm Med 17(Suppl 1):S35–S41
Deeg DJH, Knipscheer CPM, Van Tilburg W (1993) Autonomy and well-being in the aging population: Concepts and design of the Longitudinal Aging Study Amsterdam. Netherlands Institute of Gerontology, Bunnik, The Netherlands
Denkinger MD, Franke S, Rapp K et al (2010) Accelerometer-based physical activity in a large observational cohort–study protocol and design of the activity and function of the elderly in Ulm (ActiFE Ulm) study. BMC Geriatr 10:50
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Glaesmer H, Braehler E, Riedel-Heller SG et al (2011) The association of traumatic experiences and posttraumatic stress disorder with health care utilization in the elderly – a German population based study. Gen Hosp Psychiatry 33:177–184
Grant PM, Ryan CG, Tigbe WW, Granat MH (2006) The validation of a novel activity monitor in the measurement of posture and motion during everyday activities. Br J Sports Med 40:992–997
Groll DL, To T, Bombardier C, Wright JG (2005) The development of a comorbidity index with physical function as the outcome. J Clin Epidemiol 58:595–602
Guralnik JM, Simonsick EM, Ferrucci L et al (1994) A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol 49:M85–M94
Hessel A, Gunzelmann T, Geyer M, Brähler E (2000) Utilization of medical services and medication intake of patients over 60 in Germany – health related, social structure related, socio-demographic and subjective factors. Z Gerontol Geriatr 33:289–299
Lehnert T, Heider D, Leicht H et al (2011) Review: health care utilization and costs of elderly persons with multiple chronic conditions. Med Care Res Rev 68:387–420
Linden M, Horgas AL, Gilberg R et al (1997) Predicting health care utilization in the very old. The role of physical health, mental health, attitudinal and social factors. J Aging Health 9:3–27
Lubben J, Blozik E, Gillmann G et al (2006) Performance of an Abbreviated Version of the Lubben Social Network Scale Among Three European Community-Dwelling Older Adult Populations. Gerontologist 46:503–513
Nöthen M (2011) destatis Gesundheit – Magazin Wirtschaft und Statistik. Available at: http://www.destatis.de/jetspeed/portal/cms/Sites/destatis/Internet/DE/Navigation/Publikationen/Querschnittsveroeffentlichungen/WirtschaftStatistik_Gesundheit.psml. Accessed 25 January 2012
Peters D, Chen C, Markson LE et al (2006) Using an asthma control questionnaire and administrative data to predict health-care utilization. Chest 129:918–924
Plotnikoff RC, Karunamuni ND, Johnson JA et al (2008) Health-related behaviours in adults with diabetes: associations with health care utilization and costs. Can J Public Health 99:227–231
Ryan CG, Grant PM, Tigbe WW, Granat MH (2006) The validity and reliability of a novel activity monitor as a measure of walking. Br J Sports Med 40:779–784
Saliba D, Orlando M, Wenger NS et al (2000) Identifiying a short functional disability screen for older persons. J Gerontol A Biol Sci Med Sci 55:M750–M756
Stevens J, Cai J, Pamuk ER et al (1998) The effect of age on the association between body-mass index and mortality. N Engl J Med 338:1–7
Thinggaard M, Jacobsen R, Jeune B et al (2010) Is the relationship between BMI and mortality increasingly U-shaped with advancing age? A 10-year follow-up of persons aged 70–95 years. J Gerontol A Biol Sci Med Sci 65A:526–531
UCLA: Academic Technology Services, Statistical Consulting Group. Introduction to SAS. Available at: http://www.ats.ucla.edu/stat/sas/notes2/. Accessed 10 January 2012
Wernitz MH (2011) Gesundheitsökonomie und das deutsche Gesundheitswesen: ein praxisorientiertes Lehrbuch für Studium und Beruf/Martin H, Wernitz; Jörg Pelz. 1. Aufl. Kohlhammer, Stuttgart, Germany
Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67:361–370
Acknowledgement
The authors would like to thank all participants in the study.
The ActiFE Ulm study group consists of: B. Böhm, Department of Internal Medicine I – Division of Endocrinology, M. Denkinger, Agaplesion Bethesda Clinic, Ulm, Germany, H. Geiger, Department of Dermatology and Allergology, F. Herbolsheimer, Institute of Epidemiology & Medical Biometry, A. Lukas, Agaplesion Bethesda Clinic, Ulm, Germany, J. Kirchheiner, Institute of Pharmacology of Natural Products & Clinical Pharmacology, W. Koenig, Department of Internal Medicine II – Cardiology, G. Nagel, Institute of Epidemiology & Medical Biometry, T. Nikolaus (PI), Agaplesion Bethesda Clinic, Ulm, Germany, R. Peter (PI), Institute of Epidemiology & Medical Biometry, M. Riepe, Division of Gerontopsychiatry, Dept. of Psychiatry and Psychotherapy II, L. Rudolph, Max-Planck Group for Stem Cell Research, D. Rothenbacher, Institute of Epidemiology & Medical Biometry, K. Scharffetter-Kochanek, Department of Dermatology and Allergology, Ch. Schumann, Department of Internal Medicine II – Pneumology, J.M. Steinacker, Department of Sports- and Rehabilitation Medicine, C. von Arnim, Department of Neurology, G. Weinmayr, Institute of Epidemiology & Medical Biometry. (if not differently indicated: All Ulm University Ulm, Germany; PI = Principle Investigator)
Funding source
The study was funded by a grant from the Ministry of Science, Research and Arts, state of Baden-Wuerttemberg, Germany, as part of the Geriatric Competence Center, Ulm University. Michael Denkinger was supported by a research fellowship program from the Robert Bosch Foundation, Stuttgart, Germany, which did not have any influence on the content.
Conflict of interest
The corresponding author states that there are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Denkinger, M., Lukas, A., Herbolsheimer, F. et al. Physical activity and other health-related factors predict health care utilisation in older adults. Z Gerontol Geriat 45, 290–297 (2012). https://doi.org/10.1007/s00391-012-0335-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00391-012-0335-1