Abstract
Objectives
Inflammation is an important driver of abdominal pain in inflammatory bowel disease (IBD). However, some patients in remission still experience pain. We aimed to identify risk factors associated with abdominal pain in quiescent IBD (QP-IBD) and to characterize differences from patients with active disease experiencing pain (AP-IBD).
Methods
We performed a retrospective analysis utilizing data from our institution’s IBD Natural History Registry (January 1, 2015–August 31, 2018). Endoscopic evaluation, concurrent laboratory studies, and validated surveys were completed by participants. Demographic and clinical data were also abstracted.
Results
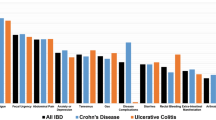
We recruited 122 patients with quiescent disease (65f:57 m; 93CD:26UC:3Indeterminate) for participation in this study, 74 (60.7%) had QP-IBD. QP-IBD patients were more likely to have anxiety/depression (71.6% vs. 25.0%, p < 0.001) or to use antidepressants (47.3% vs. 22.9%, p < 0.010), opiates (18.9% vs. 2.1%, p < 0.010), other pain medications (50.0% vs. 18.8%, p < 0.010), or corticosteroids (18.9% vs. 2.1%, p < 0.010). On logistic regression analysis, corticosteroid use, anxious/depressed state, and female gender were each independently associated with QP-IBD (p < 0.050 or less). Compared with AP-IBD patients (n = 110, 59f:51 m; 69CD:38UC:3Indeterminate), QP-IBD patients were more likely to use antidepressants (45.6% vs. 26.4%, p < 0.010). Platelet, white blood cell, C-reactive protein, and sedimentation rate levels were all less likely to be elevated in QP-IBD (all p < 0.050), though 44% exhibited pathological elevation in at least one.
Discussion
QP-IBD was independently associated with corticosteroid use, anxiety/depression, and female gender. Compared with AP-IBD, QP-IBD patients were more likely to use antidepressants and less likely to exhibit elevated inflammatory markers. However, many QP-IBD patients still demonstrated pathological elevation of these tests, demonstrating the need to develop new noninvasive screening methods for this condition.
Similar content being viewed by others
Data availability
Not applicable.
References
Bielefeldt K, Davis B, Binion DG (2009) Pain and inflammatory bowel disease. Inflamm Bowel Dis 15(5):778–788. https://doi.org/10.1002/ibd.20848
Coates MD, Lahoti M, Binion DG, Szigethy EM, Regueiro MD, Bielefeldt K (2013) Abdominal pain in ulcerative colitis. Inflamm Bowel Dis 19(10):2207–2214. https://doi.org/10.1097/MIB.0b013e31829614c6
Zeitz J, Ak M, Muller-Mottet S, Scharl S, Biedermann L, Fournier N, Frei P, Pittet V, Scharl M, Fried M, Rogler G, Vavricka S, Swiss IBDCSG (2016) Pain in IBD patients: very frequent and frequently insufficiently taken into account. PLoS One 11(6):e0156666. https://doi.org/10.1371/journal.pone.0156666
Schirbel A, Reichert A, Roll S, Baumgart DC, Buning C, Wittig B, Wiedenmann B, Dignass A, Sturm A (2010) Impact of pain on health-related quality of life in patients with inflammatory bowel disease. World J Gastroenterol 16(25):3168–3177. https://doi.org/10.3748/wjg.v16.i25.3168
Kim ES, Cho KB, Park KS, Jang BI, Kim KO, Jeon SW, Jung MK, Kim EY, Yang CH, Daegukyungbook Gastrointestinal Study G (2013) Predictive factors of impaired quality of life in Korean patients with inactive inflammatory bowel disease: association with functional gastrointestinal disorders and mood disorders. J Clin Gastroenterol 47(4):e38–e44. https://doi.org/10.1097/MCG.0b013e318266fff5
Mikocka-Walus AA, Turnbull DA, Andrews JM, Moulding NT, Holtmann GJ (2008) The effect of functional gastrointestinal disorders on psychological comorbidity and quality of life in patients with inflammatory bowel disease. Aliment Pharmacol Ther 28(4):475–483. https://doi.org/10.1111/j.1365-2036.2008.03754.x
Minderhoud IM, Oldenburg B, Wismeijer JA, van Berge Henegouwen GP, Smout AJ (2004) IBS-like symptoms in patients with inflammatory bowel disease in remission; relationships with quality of life and coping behavior. Dig Dis Sci 49(3):469–474
Hay JW, Hay AR (1992) Inflammatory bowel disease: costs-of-illness. J Clin Gastroenterol 14(4):309–317
Kappelman MD, Rifas-Shiman SL, Porter CQ, Ollendorf DA, Sandler RS, Galanko JA, Finkelstein JA (2008) Direct health care costs of Crohn’s disease and ulcerative colitis in US children and adults. Gastroenterology 135(6):1907–1913. https://doi.org/10.1053/j.gastro.2008.09.012
Ramos-Rivers C, Regueiro M, Vargas EJ, Szigethy E, Schoen RE, Dunn M, Watson AR, Schwartz M, Swoger J, Baidoo L, Barrie A, Dudekula A, Youk AO, Binion DG (2014) Association between telephone activity and features of patients with inflammatory bowel disease. Clin Gastroenterol Hepatol 12(6):986–994 e981. https://doi.org/10.1016/j.cgh.2013.11.015
Peery AF, Crockett SD, Murphy CC, Lund JL, Dellon ES, Williams JL, Jensen ET, Shaheen NJ, Barritt AS, Lieber SR, Kochar B, Barnes EL, Fan YC, Pate V, Galanko J, Baron TH, Sandler RS (2019) Burden and cost of gastrointestinal, liver, and pancreatic diseases in the United States: Update 2018. Gastroenterology 156(1):254–272 e211. https://doi.org/10.1053/j.gastro.2018.08.063
Keohane J, O'Mahony C, O'Mahony L, O'Mahony S, Quigley EM (1788) Shanahan F (2010) Irritable bowel syndrome-type symptoms in patients with inflammatory bowel disease: a real association or reflection of occult inflammation? Am J Gastroenterol 105(8):1789–1794; quiz 1795. https://doi.org/10.1038/ajg.2010.156
Deberry JJ, Bielefeldt K, Davis BM, Szigethy EM, Hartman DJ, Coates MD (2014) Abdominal pain and the neurotrophic system in ulcerative colitis. Inflamm Bowel Dis 20(12):2330–2339. https://doi.org/10.1097/MIB.0000000000000207
Vivinus-Nebot M, Frin-Mathy G, Bzioueche H, Dainese R, Bernard G, Anty R, Filippi J, Saint-Paul MC, Tulic MK, Verhasselt V, Hebuterne X, Piche T (2014) Functional bowel symptoms in quiescent inflammatory bowel diseases: role of epithelial barrier disruption and low-grade inflammation. Gut 63(5):744–752. https://doi.org/10.1136/gutjnl-2012-304066
Goodhand JR, Wahed M, Mawdsley JE, Farmer AD, Aziz Q, Rampton DS (2012) Mood disorders in inflammatory bowel disease: relation to diagnosis, disease activity, perceived stress, and other factors. Inflamm Bowel Dis 18(12):2301–2309. https://doi.org/10.1002/ibd.22916
Derwa Y, Williams CJM, Sood R, Mumtaz S, Bholah MH, Selinger CP, Hamlin PJ, Ford AC, Gracie DJ (2018) Factors affecting clinical decision-making in inflammatory bowel disease and the role of point-of-care calprotectin. Therap Adv Gastroenterol 11:1756283X17744739. https://doi.org/10.1177/1756283X17744739
Gracie DJ, Hamlin JP, Ford AC (2018) Longitudinal impact of IBS-type symptoms on disease activity, healthcare utilization, psychological health, and quality of life in inflammatory bowel disease. Am J Gastroenterol 113(5):702–712. https://doi.org/10.1038/s41395-018-0021-z
Gao Y, Khan S, Akerman M, Sultan K (2017) Analysis of the clinical indications for opiate use in inflammatory bowel disease. Intest Res 15(1):83–89. https://doi.org/10.5217/ir.2017.15.1.83
Sands BE (2004) From symptom to diagnosis: clinical distinctions among various forms of intestinal inflammation. Gastroenterology 126(6):1518–1532
Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67(6):361–370. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x
Coates MD, Soriano C, Dalessio S, Stuart A, Walter V, Koltun W, Bernasko N, Tinsley A, Clarke K, Williams ED (2020) Gastrointestinal hypoalgesia in inflammatory bowel disease. Ann Gastroenterol 33(1):45–52. https://doi.org/10.20524/aog.2019.0442
Farrokhyar F, Marshall JK, Easterbrook B, Irvine EJ (2006) Functional gastrointestinal disorders and mood disorders in patients with inactive inflammatory bowel disease: prevalence and impact on health. Inflamm Bowel Dis 12(1):38–46
Long MD, Kappelman MD, Martin CF, Chen W, Anton K, Sandler RS (2016) Role of nonsteroidal anti-inflammatory drugs in exacerbations of inflammatory bowel disease. J Clin Gastroenterol 50(2):152–156. https://doi.org/10.1097/MCG.0000000000000421
Long MD, Drossman DA (2010) Inflammatory bowel disease, irritable bowel syndrome, or what?: a challenge to the functional-organic dichotomy. Am J Gastroenterol 105(8):1796–1798. https://doi.org/10.1038/ajg.2010.162
van Hoboken EA, Thijssen AY, Verhaaren R, van der Veek PP, Prins FA, Verspaget HW, Masclee AA (2011) Symptoms in patients with ulcerative colitis in remission are associated with visceral hypersensitivity and mast cell activity. Scand J Gastroenterol 46(7-8):981–987. https://doi.org/10.3109/00365521.2011.579156
Chang L, Munakata J, Mayer EA, Schmulson MJ, Johnson TD, Bernstein CN, Saba L, Naliboff B, Anton PA, Matin K (2000) Perceptual responses in patients with inflammatory and functional bowel disease. Gut 47(4):497–505
Akbar A, Yiangou Y, Facer P, Brydon WG, Walters JR, Anand P, Ghosh S (2010) Expression of the TRPV1 receptor differs in quiescent inflammatory bowel disease with or without abdominal pain. Gut 59(6):767–774. https://doi.org/10.1136/gut.2009.194449
Minderhoud IM, Oldenburg B, Schipper ME, ter Linde JJ, Samsom M (2007) Serotonin synthesis and uptake in symptomatic patients with Crohn’s disease in remission. Clin Gastroenterol Hepatol 5(6):714–720. https://doi.org/10.1016/j.cgh.2007.02.013
Mawdsley JE, Rampton DS (2005) Psychological stress in IBD: new insights into pathogenic and therapeutic implications. Gut 54(10):1481–1491. https://doi.org/10.1136/gut.2005.064261
Rubio A, Pellissier S, Van Oudenhove L, Ly HG, Dupont P, Tack J, Dantzer C, Delon-Martin C, Bonaz B (2016) Brain responses to uncertainty about upcoming rectal discomfort in quiescent Crohn’s disease - a fMRI study. Neurogastroenterol Motil 28(9):1419–1432. https://doi.org/10.1111/nmo.12844
Spiller R, Garsed K (2009) Postinfectious irritable bowel syndrome. Gastroenterology 136(6):1979–1988. https://doi.org/10.1053/j.gastro.2009.02.074
Boeckxstaens GE (2018) The emerging role of mast cells in irritable bowel syndrome. Gastroenterol Hepatol (N Y) 14(4):250–252
Walker MM, Talley NJ, Prabhakar M, Pennaneac’h CJ, Aro P, Ronkainen J, Storskrubb T, Harmsen WS, Zinsmeister AR, Agreus L (2009) Duodenal mastocytosis, eosinophilia and intraepithelial lymphocytosis as possible disease markers in the irritable bowel syndrome and functional dyspepsia. Aliment Pharmacol Ther 29(7):765–773. https://doi.org/10.1111/j.1365-2036.2009.03937.x
Grabauskas G, Wu X, Gao J, Li JY, Turgeon DK, Owyang C (2020) Prostaglandin E2, produced by mast cells in colon tissues from patients with irritable bowel syndrome, contributes to visceral hypersensitivity in mice. Gastroenterology. 158:2195–2207.e6. https://doi.org/10.1053/j.gastro.2020.02.022
Saibeni S, Rondonotti E, Iozzelli A, Spina L, Tontini GE, Cavallaro F, Ciscato C, de Franchis R, Sardanelli F, Vecchi M (2007) Imaging of the small bowel in Crohn’s disease: a review of old and new techniques. World J Gastroenterol 13(24):3279–3287. https://doi.org/10.3748/wjg.v13.i24.3279
Coffey CJ, Kiernan MG, Sahebally SM, Jarrar A, Burke JP, Kiely PA, Shen B, Waldron D, Peirce C, Moloney M, Skelly M, Tibbitts P, Hidayat H, Faul PN, Healy V, O'Leary PD, Walsh LG, Dockery P, O'Connell RP, Martin ST, Shanahan F, Fiocchi C, Dunne CP (2018) Inclusion of the mesentery in ileocolic resection for Crohn’s disease is associated with reduced surgical recurrence. J Crohns Colitis 12(10):1139–1150. https://doi.org/10.1093/ecco-jcc/jjx187
Rivera ED, Coffey JC, Walsh D, Ehrenpreis ED (2019) The mesentery, systemic inflammation, and Crohn’s disease. Inflamm Bowel Dis 25(2):226–234. https://doi.org/10.1093/ibd/izy201
Funding
This research was supported by the Peter and Marsha Carlino Early Career Professorship in Inflammatory Bowel Disease and the Margot E. Walrath Career Development Professorship in Gastroenterology.
Author information
Authors and Affiliations
Contributions
MC developed the conceptual framework for this study, assisted with, and oversaw data collection and analysis in addition to assisting with writing and editing the manuscript. AJ assisted with data collection and analysis and helped in writing and editing the manuscript. VG assisted with analysis along with writing and editing the manuscript. PM assisted with data collection and review and editing the manuscript. SD assisted with writing and editing the manuscript. VW assisted with data analysis and helped edit the manuscript. AS assisted with data collection and organization and assisted with editing the manuscript. WK assisted in providing data and some of the conceptual frameworks for the study and edited the manuscript. NB, AT, EW, and KC assisted with the collection of data, providing the conceptual framework of the study and editing the study.
Corresponding author
Ethics declarations
Conflicts of interest
The authors of this manuscript have no relevant conflicts of interest or financial disclosures to report.
Ethics approval
This study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments and approved by the Pennsylvania State University College of Medicine Institutional Review Board.
Consent to participate
A written informed consent was obtained by all individual participants included in this study.
Consent for publication
Every patient involved in this study signed a consent form to participate in research work that could eventually be published.
Code availability
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Coates, M.D., Johri, A., Gorrepati, V.S. et al. Abdominal pain in quiescent inflammatory bowel disease. Int J Colorectal Dis 36, 93–102 (2021). https://doi.org/10.1007/s00384-020-03727-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-020-03727-3