Abstract
Purpose
In colorectal cancer (CRC), circulating tumor cells (CTCs) are released into the mesenteric veins (MV). We chose to determine whether KRAS mutations detected in CTCs from blood obtained at the time of surgery could be a marker of survival.
Methods
From 52 surgically resected CRC patients who later relapsed, samples of tumor tissue, normal tissue, and blood from the peripheral vein (PV) and MV were obtained from each patient at the time of surgery. KRAS mutations were assessed by Sanger sequencing and digital PCR (DGPCR) in tissue samples and by DGPCR in CTCs. Mutant KRAS copy number was assessed in CTCs. Results were correlated with overall survival (OS).
Results
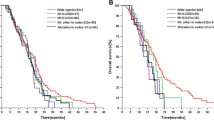
Sanger sequencing detected KRAS mutations in ten tumor samples (19.2%), while DGPCR detected mutations in 30 (58%). Mutations were detected in CTCs in 21 MV samples (40.4%) and 18 PV samples (34.6%). Patients with G13D mutations in CTCs from the MV had shorter OS than those with G12D mutations (28.1 vs 54.6 months; p = 0.025). Patients with a high mutant KRAS copy number in CTCs had shorter OS than those with a low mutant KRAS copy number (MV: 20.5 vs 43.7 months; p = 0.002; PV: 15.1 vs 38.2 months; p = 0.027).
Conclusion
DGPCR is more efficient than Sanger sequencing for detecting KRAS mutations. KRAS G13D mutations and high mutant KRAS copy number are associated with shorter OS. The analysis of KRAS mutations in CTCs from blood obtained at the time of surgery can identify patients with a higher risk of relapse.



Similar content being viewed by others
References
Miller KD, Siegel RL, Lin CC, Mariotto AB, Kramer JL, Rowland JH (2016) Cancer treatment and survivorship statistics. CA Cancer J Clin 66(4):271–289
Benson AB 3rd, Schrag D, Somerfield MR et al (2004) American Society of Clinical Oncology recommendations on adjuvant chemotherapy for stage II colon cancer. J Clin Oncol 22(16):3408–3419
Pita-Fernández S, Alhayek-Aí M, González-Martín C, López-Calviño B, Seoane-Pillado T, Pértega-Díaz S (2015) Intensive follow-up strategies improve outcomes in nonmetastatic colorectal cancer patients after curative surgery: a systematic review and meta-analysis. Ann Oncol 26(4):644–656
Rose J, Augestad KM, Cooper GS (2014) Colorectal cancer surveillance: what’s new and what’s next. World J Gastroenterol 20(8):1887–1897
de Jong MC, Pulitano C, Ribero D et al (2009) Rates and patterns of recurrence following curative intent surgery for colorectal liver metastasis: an international multi-institutional analysis of 1669 patients. Ann Surg 250(3):440–448
Pfannschmidt J, Dienemann H, Hoffmann H (2007) Surgical resection of pulmonary metastases from colorectal cancer: a systematic review of published series. Ann Thorac Surg 84(1):324–338
Jones RP, Jackson R, Dunne DF, Malik HZ, Fenwick SW, Poston GJ, Ghaneh P (2012) Systematic review and meta-analysis of follow-up after hepatectomy for colorectal liver metastases. Br J Surg 99(4):477–486
Andreyev HJ, Norman AR, Cunningham D, Oates J, Dix BR, Iacopetta BJ, Young J, Walsh T, Ward R, Hawkins N, Beranek M, Jandik P, Benamouzig R, Jullian E, Laurent-Puig P, Olschwang S, Muller O, Hoffmann I, Rabes HM, Zietz C, Troungos C, Valavanis C, Yuen ST, Ho JW, Croke CT, O’Donoghue DP, Giaretti W, Rapallo A, Russo A, Bazan V, Tanaka M, Omura K, Azuma T, Ohkusa T, Fujimori T, Ono Y, Pauly M, Faber C, Glaesener R, de Goeij AF, Arends JW, Andersen SN, Lövig T, Breivik J, Gaudernack G, Clausen OP, de Angelis PD, Meling GI, Rognum TO, Smith R, Goh HS, Font A, Rosell R, Sun XF, Zhang H, Benhattar J, Losi L, Lee JQ, Wang ST, Clarke PA, Bell S, Quirke P, Bubb VJ, Piris J, Cruickshank NR, Morton D, Fox JC, al-Mulla F, Lees N, Hall CN, Snary D, Wilkinson K, Dillon D, Costa J, Pricolo VE, Finkelstein SD, Thebo JS, Senagore AJ, Halter SA, Wadler S, Malik S, Krtolica K, Urosevic N (2001) Kirsten ras mutations in patients with colorectal cancer: the ‘RASCAL II’ study. Br J Cancer 85(5):692–696
Haigis KM (2017) KRAS alleles: the devil is in the detail. Trends Cancer 3(10):686–697
McGranahan N, Favero F, de Bruin EC et al (2015) Clonal status of actionable driver events and the timing of mutational processes in cancer evolution. Sci Transl Med 7(283):283ra54
Misale S, Yaeger R, Hobor S, Scala E, Janakiraman M, Liska D, Valtorta E, Schiavo R, Buscarino M, Siravegna G, Bencardino K, Cercek A, Chen CT, Veronese S, Zanon C, Sartore-Bianchi A, Gambacorta M, Gallicchio M, Vakiani E, Boscaro V, Medico E, Weiser M, Siena S, di Nicolantonio F, Solit D, Bardelli A (2012) Emergence of KRAS mutations and acquired resistance to anti-EGFR therapy in colorectal cancer. Nature 486(7404):532–536
Normanno N, Tejpar S, Morgillo F, De Luca A, Van Cutsem E, Ciardiello F (2009) Implications for KRAS status and EGFR-targeted therapies in metastatic CRC. Nat Rev Clin Oncol 6(9):519–527
Imamura Y, Morikawa T, Liao X et al (2012) Specific mutations in KRAS codons 12 and 13, and patient prognosis in 1075 BRAF wild-type colorectal cancers. Clin Cancer Res 18(17):4753–4763
Yoon HH, Tougeron D, Shi Q, Alberts SR, Mahoney MR, Nelson GD, Nair SG, Thibodeau SN, Goldberg RM, Sargent DJ, Sinicrope FA, Alliance for Clinical Trials in Oncology (2014) KRAS codon 12 and 13 mutations in relation to disease-free survival in BRAF-wild-type stage III colon cancers from an adjuvant chemotherapy trial (N0147 alliance). Clin Cancer Res 20(11):3033–3043
Samowitz WS, Curtin K, Schaffer D, Robertson M, Leppert M, Slattery ML (2000) Relationship of Ki-ras mutations in colon cancers to tumor location, stage, and survival: a population-based study. Cancer Epidemiol Biomark Prev 9(11):1193–1197
Modest DP, Stintzing S, Laubender RP et al (2011) Clinical characterization of patients with metastatic colorectal cancer depending on the KRAS status. Anti-Cancer Drugs 22(9):913–918
Karapetis CS, Khambata-Ford S, Jonker DJ, O’Callaghan CJ, Tu D, Tebbutt NC, Simes RJ, Chalchal H, Shapiro JD, Robitaille S, Price TJ, Shepherd L, Au HJ, Langer C, Moore MJ, Zalcberg JR (2008) K-ras mutations and benefit from cetuximab in advanced colorectal cancer. N Engl J Med 359(17):1757–1765
De Roock W, Jonker DJ, Di Nicolantonio F et al (2010) Association of KRAS p.G13D mutation with outcome in patients with chemotherapy-refractory metastatic colorectal cancer treated with cetuximab. JAMA 304(16):1812–1820
Gajate P, Sastre J, Bando I, Alonso T, Cillero L, Sanz J, Caldés T, Díaz-Rubio E (2012) Influence of KRAS p.G13D mutation in patients with metastatic colorectal cancer treated with cetuximab. Clin Colorectal Cancer 11(4):291–296
Sottoriva A, Kang H, Ma Z, Graham TA, Salomon MP, Zhao J, Marjoram P, Siegmund K, Press MF, Shibata D, Curtis C (2015) A big bang model of human colorectal tumor growth. Nat Genet 47(3):209–216
Normanno N, Rachiglio AM, Lambiase M, Martinelli E, Fenizia F, Esposito C, Roma C, Troiani T, Rizzi D, Tatangelo F, Botti G, Maiello E, Colucci G, Ciardiello F, CAPRI-GOIM investigators (2015) Heterogeneity of KRAS, NRAS, BRAF and PIK3CA mutations in metastatic colorectal cancer and potential effects on therapy in the CAPRI GOIM trial. Ann Oncol 26(8):1710–1714
Pantel K, Alix-Panabières C (2019) Liquid biopsy and minimal residual disease - latest advances and implications for cure. Nat Rev Clin Oncol 16(7):409–424
Sabari JK, Offin M, Stephens D et al (2019) A prospective study of circulating tumor DNA to guide matched targeted therapy in lung cancers. J Natl Cancer Inst 111(6):575–583
Cohen SJ, Punt CJ, Iannotti N, Saidman BH, Sabbath KD, Gabrail NY, Picus J, Morse M, Mitchell E, Miller MC, Doyle GV, Tissing H, Terstappen LW, Meropol NJ (2008) Relationship of circulating tumor cells to tumor response, progression-free survival, and overall survival in patients with metastatic colorectal cancer. J Clin Oncol 26(19):3213–3221
Sastre J, Maestro ML, Gómez-España A et al (2012) Circulating tumor cell count is a prognostic factor in metastatic colorectal cancer patients receiving first-line chemotherapy plus bevacizumab: a Spanish Cooperative Group for the Treatment of Digestive Tumors study. Oncologist 17(7):947–955
Lu CY, Tsai HL, Uen YH, Hu HM, Chen CW, Cheng TL, Lin SR, Wang JY (2013) Circulating tumor cells as a surrogate marker for determining clinical outcome to mFOLFOX chemotherapy in patients with stage III colon cancer. Br J Cancer 108(4):791–797
Demuth C, Spindler KG, Johansen JS et al (2018) Measuring KRAS mutations in circulating tumor DNA by droplet digital PCR and next-generation sequencing. Trans Oncol 11(5):1220–1224
Kondo Y, Hayashi K, Kawakami K, Miwa Y, Hayashi H, Yamamoto M (2017) KRAS mutation analysis of single circulating tumor cells from patients with metastatic colorectal cancer. BMC Cancer 17(1):311
Kalikaki A, Politaki H, Souglakos J, Apostolaki S, Papadimitraki E, Georgoulia N, Tzardi M, Mavroudis D, Georgoulias V, Voutsina A (2014) KRAS genotypic changes of circulating tumor cells during treatment of patients with metastatic colorectal cancer. PLoS One 9(8):e104902
Navarro A, Molins L, Marrades RM et al (2019) Exosome Analysis in Tumor-Draining Pulmonary Vein Identifies NSCLC Patients with Higher Risk of Relapse after Curative Surgery. Cancers (Basel) 11(2):249
Crosbie PA, Shah R, Krysiak P, Zhou C, Morris K, Tugwood J, Booton R, Blackhall F, Dive C (2016) Circulating tumor cells detected in the tumor-draining pulmonary vein are associated with disease recurrence after surgical resection of NSCLC. J Thorac Oncol 11(10):1793–1797
Santasusagna S, Moreno I, Navarro A, Castellano JJ, Martinez F, Hernández R, Muñoz C, Monzo M (2018) Proteomic analysis of liquid biopsy from tumor-draining vein indicates that high expression of exosomal ECM1 is associated with relapse in stage I-III colon cancer. Transl Oncol 11(3):715–721
Chemi F, Rothwell DG, McGranahan N, Gulati S, Abbosh C, Pearce SP, Zhou C, Wilson GA, Jamal-Hanjani M, Birkbak N, Pierce J, Kim CS, Ferdous S, Burt DJ, Slane-Tan D, Gomes F, Moore D, Shah R, al Bakir M, Hiley C, Veeriah S, Summers Y, Crosbie P, Ward S, Mesquita B, Dynowski M, Biswas D, Tugwood J, Blackhall F, Miller C, Hackshaw A, Brady G, Swanton C, Dive C, TRACERx Consortium (2019) Pulmonary venous circulating tumor cell dissemination before tumor resection and disease relapse. Nat Med 25(10):1534–1539
Gutiérrez C, Rodriguez J, Patiño-García A, García-Foncillas J, Salgado J (2013) KRAS mutational status analysis of peripheral blood isolated circulating tumor cells in metastatic colorectal patients. Oncol Lett 6(5):1343–1345
Brungs D, Lynch D, Luk AW, Minaei E, Ranson M, Aghmesheh M, Vine KL, Carolan M, Jaber M, de Souza P, Becker TM (2018) Cryopreservation for delayed circulating tumor cell isolation is a valid strategy for prognostic association of circulating tumor cells in gastroesophageal cancer. World J Gastroenterol 24(7):810–818
Laurent-Puig P, Pekin D, Normand C, Kotsopoulos SK, Nizard P, Perez-Toralla K, Rowell R, Olson J, Srinivasan P, le Corre D, Hor T, el Harrak Z, Li X, Link DR, Bouché O, Emile JF, Landi B, Boige V, Hutchison JB, Taly V (2015) Clinical relevance of KRAS-mutated subclones detected with picodroplet digital PCR in advanced colorectal cancer treated with anti-EGFR therapy. Clin Cancer Res 21(5):1087–1097
Pekin D, Skhiri Y, Baret JC, le Corre D, Mazutis L, Salem CB, Millot F, el Harrak A, Hutchison JB, Larson JW, Link DR, Laurent-Puig P, Griffiths AD, Taly V (2011) Quantitative and sensitive detection of rare mutations using droplet-based microfluidics. Lab Chip 11(13):2156–2166
Strilic B, Offermanns S (2017) Intravascular survival and extravasation of tumor cells. Cancer Cell 32(3):282–293
Funding
This study was partially supported by Servei de Donació del Cos a la Ciencia (Body Donation Service) of the Faculty of Medicine and Health Sciences, University of Barcelona, and by grants from the Ministry of Economy, Industry and Competition, Agencia Estatal de Investigación co-financed with the European Union FEDER funds SAF2017-88606-P (AEI/FEDER, UE).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional review board of the Hospital Municipal de Badalona and the Ethical Committee of the School of Medicine, University of Barcelona (Institutional Review Board—IRB00003099) and with the 1964 Helsinki Declaration and its later amendments. Informed consent was obtained from all individual participants included in the study. Y.L and J.C are APIF fellows of the Universitat de Barcelona. The other authors declare no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, Y., Monzo, M., Moreno, I. et al. KRAS mutations by digital PCR in circulating tumor cells isolated from the mesenteric vein are associated with residual disease and overall survival in resected colorectal cancer patients. Int J Colorectal Dis 35, 805–813 (2020). https://doi.org/10.1007/s00384-020-03538-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-020-03538-6