Abstract
Purpose
The aim of our study was to compare the characteristics and prognosis between right- and left-sided metastatic colorectal carcinomas.
Methods
Data from 937 patients with stage IV colorectal carcinomas (synchronous distant metastasis) who had a resection of the primary tumour between 1985 and 2014 were analysed. Carcinomas in the caecum to transverse colon were defined as right-sided (n = 250; 26.7%). They were compared to tumours located from the splenic flexure to the rectum categorised as left-sided (n = 687; 73.3%).
Results
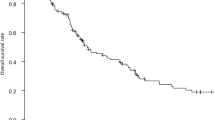
In right-sided carcinomas, we observed significantly more female patients (50.8 vs 36.2%; p < 0.001), more unfavourable histological types (24.0 vs 8.6%; p < 0.001), more M1c carcinomas (metastases to the peritoneum ± others; 32.0 vs 14.4%; p < 0.001) and more emergencies (11.6 vs 7.1%; p = 0.029), while multimodal treatment was utilised in fewer patients (51.6 vs 63.8%; p = 0.001) and curative resections were less frequently (24.1 vs 35.4%; p = 0.002). Prognosis was significantly worse in patients with right-sided carcinomas (2-year-survival 27.2 vs 44.6%, p < 0.01). This difference was more pronounced after R2 resection (15.3 vs 29.7%; p < 0.001), than after macroscopic curative resection (2-year-survival 63.9 vs 71.9%; p = 0.106). In multivariate Cox regression analysis, tumour site was found to be an independent prognostic factor for overall survival (HR 1.2; 95% CI 1.0–1.5; p = 0.012). During the three 10-year periods, the prognosis improved equally in patients with right- and left-sided carcinomas, while the differences in survival remained identical.
Conclusions
In a surgical patient cohort undergoing primary tumour resection, significant differences in prognosis were observed between patients with metastatic right- and left-sided colorectal carcinomas.

Similar content being viewed by others
References
Arnold D, Lueza B, Douillard JY, Peeters M, Lenz HJ, Venook A, Heinemann V, Van Cutsem E, Pignon JP, Tabernero J, Cervantes A, Ciardiello F (2017) Prognostic and predictive value of primary tumour side in patients with RAS wild-type metastatic colorectal cancer treated with chemotherapy and EGFR directed antibodies in six randomized trials. Annals of oncology : Official Journal of the European Society for Medical Oncology 28(8):1713–1729. https://doi.org/10.1093/annonc/mdx175
Tejpar S, Stintzing S, Ciardiello F, Tabernero J, Van Cutsem E, Beier F, Esser R, Lenz HJ, Heinemann V (2016) Prognostic and predictive relevance of primary tumor location in patients with RAS wild-type metastatic colorectal Cancer: retrospective analyses of the CRYSTAL and FIRE-3 trials. JAMA Oncology 3:194. https://doi.org/10.1001/jamaoncol.2016.3797
Stintzing S, Modest DP, Rossius L, Lerch MM, von Weikersthal LF, Decker T, Kiani A, Vehling-Kaiser U, Al-Batran SE, Heintges T, Lerchenmuller C, Kahl C, Seipelt G, Kullmann F, Stauch M, Scheithauer W, Held S, Giessen-Jung C, Moehler M, Jagenburg A, Kirchner T, Jung A, Heinemann V, FIRE-3 investigators (2016) FOLFIRI plus cetuximab versus FOLFIRI plus bevacizumab for metastatic colorectal cancer (FIRE-3): a post-hoc analysis of tumour dynamics in the final RAS wild-type subgroup of this randomised open-label phase 3 trial. Lancet Oncol 17(10):1426–1434. https://doi.org/10.1016/S1470-2045(16)30269-8
van Rooijen KL, Shi Q, Goey KKH, Meyers J, Heinemann V, Diaz-Rubio E, Aranda E, Falcone A, Green E, de Gramont A, Sargent DJ, Punt CJA, Koopman M (2018) Prognostic value of primary tumour resection in synchronous metastatic colorectal cancer: individual patient data analysis of first-line randomised trials from the ARCAD database. Eur J Cancer 91:99–106. https://doi.org/10.1016/j.ejca.2017.12.014
Hohenberger W, Weber K, Matzel K, Papadopoulos T, Merkel S (2009) Standardized surgery for colonic cancer: complete mesocolic excision and central ligation—technical notes and outcome. Colorectal disease : the official Journal of the Association of Coloproctology of Great Britain and Ireland 11(4):354–364; discussion 364-355. https://doi.org/10.1111/j.1463-1318.2008.01735.x
Merkel S, Weber K, Matzel KE, Agaimy A, Gohl J, Hohenberger W (2016) Prognosis of patients with colonic carcinoma before, during and after implementation of complete mesocolic excision. Br J Surg 103(9):1220–1229. https://doi.org/10.1002/bjs.10183
Heald RJ, Husband EM, Ryall RD (1982) The mesorectum in rectal cancer surgery—the clue to pelvic recurrence? Br J Surg 69(10):613–616
Sargent DJ, Kohne CH, Sanoff HK, Bot BM, Seymour MT, de Gramont A, Porschen R, Saltz LB, Rougier P, Tournigand C, Douillard JY, Stephens RJ, Grothey A, Goldberg RM (2009) Pooled safety and efficacy analysis examining the effect of performance status on outcomes in nine first-line treatment trials using individual data from patients with metastatic colorectal cancer. J Clin Oncol Off J Am Soc Clin Oncol 27(12):1948–1955. https://doi.org/10.1200/JCO.2008.20.2879
Brierly JD, Gospodarowicz MK, Wittekind C (2017) TNM classification of malignant tumours, 8th edn. Wiley Blackwell, Oxford
Amin MB, Edge SB, Greene FL, Schilsky RL, Gaspar LE, Washington MK, Sullivan DC, Brookland RK (2017) AJCC Cancer Staging Manual. 8th edn. Springer
WHO; Bosman FT, Carneiro F, Hruban RH,Theise ND (eds) (2010) WHO Classification of Tumours of the Digestive System. 4th edn. WHO Press, Geneva, Switzerland
Greenwood M (1926) The errors of sampling of the survivorship table reports on public health and medical subjects, vol vol.33. Her Majesty’s Stationery Office, London
He WZ, Liao FX, Jiang C, Kong PF, Yin CX, Yang Q, Qiu HJ, Zhang B, Xia LP (2017) Primary tumor location as a predictive factor for first-line bevacizumab effectiveness in metastatic colorectal cancer patients. J Cancer 8(3):388–394. https://doi.org/10.7150/jca.16804
Boeckx N, Koukakis R, Op de Beeck K, Rolfo C, Van Camp G, Siena S, Tabernero J, Douillard JY, Andre T, Peeters M (2017) Primary tumor sidedness has an impact on prognosis and treatment outcome in metastatic colorectal cancer: results from two randomized first-line panitumumab studies. Annals of Oncology : Official Journal of the European Society for Medical Oncology 28(8):1862–1868. https://doi.org/10.1093/annonc/mdx119
Cao DD, Xu HL, Xu XM, Ge W (2017) The impact of primary tumor location on efficacy of cetuximab in metastatic colorectal cancer patients with different KRAS status: a systematic review and meta-analysis. Oncotarget 8(32):53631–53641. https://doi.org/10.18632/oncotarget.19022
Li XF, Tan YN, Zhong CH, Zhu LZ, Fang XF, Li J, Ding KF, Yuan Y (2017) Left-sided primary tumor is a favorable prognostic factor for metastatic colorectal cancer patients receiving surgery. Oncotarget 8(45):79618–79628. https://doi.org/10.18632/oncotarget.18896
Kohne CH, Wils J, Lorenz M, Schoffski P, Voigtmann R, Bokemeyer C, Lutz M, Kleeberg C, Ridwelski K, Souchon R, El-Serafi M, Weiss U, Burkhard O, Ruckle H, Lichnitser M, Langenbuch T, Scheithauer W, Baron B, Couvreur ML, Schmoll HJ, European Organization of R, Treatment of Cancer Gastrointestinal Group S (2003) Randomized phase III study of high-dose fluorouracil given as a weekly 24-hour infusion with or without leucovorin versus bolus fluorouracil plus leucovorin in advanced colorectal cancer: European organization of Research and Treatment of Cancer Gastrointestinal Group Study 40952. J Clin Oncol Off J Am Soc Clin Oncol 21(20):3721–3728. https://doi.org/10.1200/JCO.2003.11.122
de Gramont A, Bosset JF, Milan C, Rougier P, Bouche O, Etienne PL, Morvan F, Louvet C, Guillot T, Francois E, Bedenne L (1997) Randomized trial comparing monthly low-dose leucovorin and fluorouracil bolus with bimonthly high-dose leucovorin and fluorouracil bolus plus continuous infusion for advanced colorectal cancer: a French intergroup study. J Clin Oncol Off J Am Soc Clin Oncol 15(2):808–815. https://doi.org/10.1200/JCO.1997.15.2.808
de Gramont A, Figer A, Seymour M, Homerin M, Hmissi A, Cassidy J, Boni C, Cortes-Funes H, Cervantes A, Freyer G, Papamichael D, Le Bail N, Louvet C, Hendler D, de Braud F, Wilson C, Morvan F, Bonetti A (2000) Leucovorin and fluorouracil with or without oxaliplatin as first-line treatment in advanced colorectal cancer. J Clin Oncol Off J Am Soc Clin Oncol 18(16):2938–2947. https://doi.org/10.1200/JCO.2000.18.16.2938
Douillard JY, Cunningham D, Roth AD, Navarro M, James RD, Karasek P, Jandik P, Iveson T, Carmichael J, Alakl M, Gruia G, Awad L, Rougier P (2000) Irinotecan combined with fluorouracil compared with fluorouracil alone as first-line treatment for metastatic colorectal cancer: a multicentre randomised trial. Lancet 355(9209):1041–1047
Saltz LB, Cox JV, Blanke C, Rosen LS, Fehrenbacher L, Moore MJ, Maroun JA, Ackland SP, Locker PK, Pirotta N, Elfring GL, Miller LL (2000) Irinotecan plus fluorouracil and leucovorin for metastatic colorectal cancer. Irinotecan Study Group The New England Journal of Medicine 343(13):905–914. https://doi.org/10.1056/NEJM200009283431302
Van Cutsem E, Kohne CH, Lang I, Folprecht G, Nowacki MP, Cascinu S, Shchepotin I, Maurel J, Cunningham D, Tejpar S, Schlichting M, Zubel A, Celik I, Rougier P, Ciardiello F (2011) Cetuximab plus irinotecan, fluorouracil, and leucovorin as first-line treatment for metastatic colorectal cancer: updated analysis of overall survival according to tumor KRAS and BRAF mutation status. J Clin Oncol Off J Am Soc Clin Oncol 29(15):2011–2019. https://doi.org/10.1200/JCO.2010.33.5091
Saltz LB, Clarke S, Diaz-Rubio E, Scheithauer W, Figer A, Wong R, Koski S, Lichinitser M, Yang TS, Rivera F, Couture F, Sirzen F, Cassidy J (2008) Bevacizumab in combination with oxaliplatin-based chemotherapy as first-line therapy in metastatic colorectal cancer: a randomized phase III study. J Clin Oncol Off J Am Soc Clin Oncol 26(12):2013–2019. https://doi.org/10.1200/JCO.2007.14.9930
Kabbinavar FF, Schulz J, McCleod M, Patel T, Hamm JT, Hecht JR, Mass R, Perrou B, Nelson B, Novotny WF (2005) Addition of bevacizumab to bolus fluorouracil and leucovorin in first-line metastatic colorectal cancer: results of a randomized phase II trial. J Clin Oncol Off J Am Soc Clin Oncol 23(16):3697–3705. https://doi.org/10.1200/JCO.2005.05.112
Hurwitz H, Fehrenbacher L, Novotny W, Cartwright T, Hainsworth J, Heim W, Berlin J, Baron A, Griffing S, Holmgren E, Ferrara N, Fyfe G, Rogers B, Ross R, Kabbinavar F (2004) Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med 350(23):2335–2342. https://doi.org/10.1056/NEJMoa032691
Heinemann V, von Weikersthal LF, Decker T, Kiani A, Vehling-Kaiser U, Al-Batran SE, Heintges T, Lerchenmuller C, Kahl C, Seipelt G, Kullmann F, Stauch M, Scheithauer W, Hielscher J, Scholz M, Muller S, Link H, Niederle N, Rost A, Hoffkes HG, Moehler M, Lindig RU, Modest DP, Rossius L, Kirchner T, Jung A, Stintzing S (2014) FOLFIRI plus cetuximab versus FOLFIRI plus bevacizumab as first-line treatment for patients with metastatic colorectal cancer (FIRE-3): a randomised, open-label, phase 3 trial. Lancet Oncol 15(10):1065–1075. https://doi.org/10.1016/S1470-2045(14)70330-4
Lievre A, Bachet JB, Boige V, Cayre A, Le Corre D, Buc E, Ychou M, Bouche O, Landi B, Louvet C, Andre T, Bibeau F, Diebold MD, Rougier P, Ducreux M, Tomasic G, Emile JF, Penault-Llorca F, Laurent-Puig P (2008) KRAS mutations as an independent prognostic factor in patients with advanced colorectal cancer treated with cetuximab. J Clin Oncol Off J Am Soc Clin Oncol 26(3):374–379. https://doi.org/10.1200/JCO.2007.12.5906
Folprecht G, Grothey A, Alberts S, Raab HR, Kohne CH (2005) Neoadjuvant treatment of unresectable colorectal liver metastases: correlation between tumour response and resection rates. Annals of Oncology : Official Journal of the European Society for Medical Oncology 16(8):1311–1319. https://doi.org/10.1093/annonc/mdi246
Folprecht G, Gruenberger T, Bechstein WO, Raab HR, Lordick F, Hartmann JT, Lang H, Frilling A, Stoehlmacher J, Weitz J, Konopke R, Stroszczynski C, Liersch T, Ockert D, Herrmann T, Goekkurt E, Parisi F, Kohne CH (2010) Tumour response and secondary resectability of colorectal liver metastases following neoadjuvant chemotherapy with cetuximab: the CELIM randomised phase 2 trial. Lancet Oncol 11(1):38–47. https://doi.org/10.1016/S1470-2045(09)70330-4
Ye LC, Liu TS, Ren L, Wei Y, Zhu DX, Zai SY, Ye QH, Yu Y, Xu B, Qin XY, Xu J (2013) Randomized controlled trial of cetuximab plus chemotherapy for patients with KRAS wild-type unresectable colorectal liver-limited metastases. J Clin Oncol Off J Am Soc Clin Oncol 31(16):1931–1938. https://doi.org/10.1200/JCO.2012.44.8308
Jegatheeswaran S, Mason JM, Hancock HC, Siriwardena AK (2013) The liver-first approach to the management of colorectal cancer with synchronous hepatic metastases: a systematic review. JAMA Surg 148(4):385–391. https://doi.org/10.1001/jamasurg.2013.1216
Wein A, Emmert M, Merkel S, Harich HD, Siebler J, Thiemann R, Lamberti C, Gottler B, Fries S, Kiani A, Schlag R, Gruner M, Steinbild S, Eberl S, Pohl-Dernick K, Dorje F, Horbach T, Schoffski O, Neurath MF, Hohenberger W (2015) Palliative treatment of colorectal cancer with secondary metastasis resection in Germany—impact of the multidisciplinary treatment approach on prognosis and cost: the northern Bavaria IVOPAK I project. Oncology 88(2):103–121. https://doi.org/10.1159/000368246
Schadde E, Ardiles V, Slankamenac K, Tschuor C, Sergeant G, Amacker N, Baumgart J, Croome K, Hernandez-Alejandro R, Lang H, de Santibanes E, Clavien PA (2014) ALPPS offers a better chance of complete resection in patients with primarily unresectable liver tumors compared with conventional-staged hepatectomies: results of a multicenter analysis. World J Surg 38(6):1510–1519. https://doi.org/10.1007/s00268-014-2513-3
Schadde E, Ardiles V, Robles-Campos R, Malago M, Machado M, Hernandez-Alejandro R, Soubrane O, Schnitzbauer AA, Raptis D, Tschuor C, Petrowsky H, De Santibanes E, Clavien PA, Group AR (2014) Early survival and safety of ALPPS: first report of the international ALPPS registry. Ann Surg 260(5):829–836; discussion 836-828. https://doi.org/10.1097/SLA.0000000000000947
de Baere T, Auperin A, Deschamps F, Chevallier P, Gaubert Y, Boige V, Fonck M, Escudier B, Palussiere J (2015) Radiofrequency ablation is a valid treatment option for lung metastases: experience in 566 patients with 1037 metastases. Annals of Oncology : Official Journal of the European Society for Med Oncol 26(5):987–991. https://doi.org/10.1093/annonc/mdv037
Cho JH, Kim S, Namgung M, Choi YS, Kim HK, Zo JI, Shim YM, Kim J (2015) The prognostic importance of the number of metastases in pulmonary metastasectomy of colorectal cancer. World Journal of Surgical Oncology 13:222. https://doi.org/10.1186/s12957-015-0621-7
Elias D, Goere D, Dumont F, Honore C, Dartigues P, Stoclin A, Malka D, Boige V, Ducreux M (2014) Role of hyperthermic intraoperative peritoneal chemotherapy in the management of peritoneal metastases. Eur J Cancer 50(2):332–340. https://doi.org/10.1016/j.ejca.2013.09.024
Schmiegel W, Buchberger B, Follmann M, Graeven U, Heinemann V, Langer T, Nothacker M, Porschen R, Rodel C, Rosch T, Schmitt W, Wesselmann S, Pox C (2017) S3-Leitlinie - Kolorektales Karzinom. Zeitschrift fur Gastroenterologie 55(12):1344–1498. https://doi.org/10.1055/s-0043-121106
Douillard JY, Oliner KS, Siena S, Tabernero J, Burkes R, Barugel M, Humblet Y, Bodoky G, Cunningham D, Jassem J, Rivera F, Kocakova I, Ruff P, Blasinska-Morawiec M, Smakal M, Canon JL, Rother M, Williams R, Rong A, Wiezorek J, Sidhu R, Patterson SD (2013) Panitumumab-FOLFOX4 treatment and RAS mutations in colorectal cancer. N Engl J Med 369(11):1023–1034. https://doi.org/10.1056/NEJMoa1305275
Overman MJ, McDermott R, Leach JL, Lonardi S, Lenz HJ, Morse MA, Desai J, Hill A, Axelson M, Moss RA, Goldberg MV, Cao ZA, Ledeine JM, Maglinte GA, Kopetz S, Andre T (2017) Nivolumab in patients with metastatic DNA mismatch repair-deficient or microsatellite instability-high colorectal cancer (CheckMate 142): an open-label, multicentre, phase 2 study. Lancet Oncol 18(9):1182–1191. https://doi.org/10.1016/S1470-2045(17)30422-9
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Merkel, S., Schellerer, V.S., Wein, A. et al. The influence of tumour site on prognosis in metastatic colorectal carcinomas with primary tumour resection. Int J Colorectal Dis 33, 1215–1223 (2018). https://doi.org/10.1007/s00384-018-3098-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-018-3098-3