Abstract
Purpose
Several studies demonstrate an increased prevalence and concordance of inflammatory bowel disease among the relatives of patients. Other studies suggest that genetic influence is over-estimated. The aims of this study are to evaluate the phenotypic expression and the treatment requirements in familial inflammatory bowel disease, to study the relationship between number of relatives and degree of kinship with disease severity and to quantify the impact of family aggregation compared to other environmental factors.
Methods
Observational analytical study of 1211 patients followed in our unit. We analyzed, according to the existence of familial association, number and degree of consanguinity, the phenotypic expression, complications, extraintestinal manifestations, treatment requirements, and mortality. A multivariable analysis considering smoking habits and non-steroidal-anti-inflammatory drugs was performed.
Results
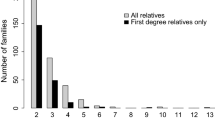
14.2% of patients had relatives affected. Median age at diagnosis tended to be lower in the familial group, 32 vs 29, p = 0.07. In familial ulcerative colitis, there was a higher proportion of extraintestinal manifestations: peripheral arthropathy (OR = 2.3, p = 0.015) and erythema nodosum (OR = 7.6, p = 0.001). In familial Crohn’s disease, there were higher treatment requirements: immunomodulators (OR = 1.8, p = 0.029); biologics (OR = 1.9, p = 0.011); and surgery (OR = 1.7, p = 0.044). The abdominal abscess increased with the number of relatives affected: 5.1% (sporadic), 7.0% (one), and 14.3% (two or more), p=0.039. These associations were maintained in the multivariate analysis.
Conclusions
Familial aggregation is considered a risk factor for more aggressive disease and higher treatment requirements, a tendency for earlier onset, more abdominal abscess, and extraintestinal manifestations, remaining a risk factor analyzing the influence of some environmental factors.


Similar content being viewed by others
References
Trier F et al (2015) Familial risk of inflammatory bowel disease: a population-based cohort study 1977-2011. Am J Gastroenterol 110:564–571
Andreu M et al (2014) Disease severity in familial cases of IBD. J Crohn’s Colitis 8:234–239
Colombel J-F et al (1996) Clinical characteristics of Crohn’s disease in 72 families. Gastroenterol 111:604–607
Peeters M et al (1996) Familial aggregation in Crohn’s disease: increased age-adjusted risk and concordance in clinical characteristics. Gastroenterol 11:597–603
Orholm M et al (1991) Familial occurrence of inflammatory bowel disease. N Engl J Med 324:84–88
Cabré E et al (2014) Phenotypic concordance in familial inflammatory bowel disease (IBD). Result of a nationwide IBD Spanish database. J Crohn’s Colitis 8:654–661
Steven R. Brant (2011). Update on the heritability of inflammatory bowel disease: the importance of twin studies. Inflamm Bowel Dis.
Bayless T et al (1996) Crohn’s disease: concordance for site and clinical type in affected family members- potential hereditary influences. Gastroenterol 111:573–579
Halfvarson J et al (2011) Genetic in twins with Chron’s disease: less pronounced than previously believed? Inflamm Bowel Dis 17:6–12
John C et al (1996) Inflammatory bowel disease in 97 families each with three or more affected first-degree relatives. Gastroenterol 111:587–596
Dignass A et al (2012) The second European evidence-based consensus on the diagnosis and management of ulcerative colitis part 1: definitions and diagnosis. J Crohn’s Colitis 6:965–990
Van Assche G et al (2010) The second European evidence-based consensus on the diagnosis and management of Crohn’s disease: definitions and diagnosis. J Crohn’s Colitis 4:7–27
Silverberg MS et al (2005) Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a working party of the 2005 Montreal Congress of Gastroenterology. Can J Gastroenterol 19:5–36
Satsangi J et al (1996) Clinical patterns of familial inflammatory bowel disease. Gut 38:738–741
Loddo I et al (2015) Inflammatory bowel disease: genetics, epigenetics, and pathogenesis. Front Immunol 6:551
Gordon H et al (2015) Heritability in inflammatory bowel disease: from the first twin study to genome-wide association studies. Inflamm Bowel Dise 21:1428–1434
Acknowledgement
To all the people who collaborated in the study:
Data collection: Joan Tosca, Marta Maia Bosca-Watts, Ana Sanahuja, Pablo Navarro, Isabel Pascual, Rosario Antón, Francisco Mora, Miguel Mínguez.
Study design: María Pilar Ballester, David Martí, Miguel Minguez.
Literature search: María Pilar Ballester, David Martí.
Data analysis and interpretation: María Pilar Ballester, Joan Tosca.
Writing: María Pilar Ballester, David Martí, Joan Tosca, Marta Maia Bosca-Watts, Miguel Minguez.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the institutional ethics committee of the hospital.
Funding statement
The authors declare no funding support.
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Spanish Gastroenterology conference (Spanish Gastroenterology Association) in Madrid, March 2016 and Digestive Disease Week (American Gastroenterology Association) in San Diego, May 2016.
Electronic supplementary material
Supplementary Figure 1
(DOCX 24 kb)
Supplementary Figure 2
(DOCX 18 kb)
Supplementary Figure 3
(DOCX 25 kb)
Supplementary Figure 4
(DOCX 19 kb)
Supplementary Table 1
(DOCX 11.9 kb)
Rights and permissions
About this article
Cite this article
Ballester, M.P., Martí, D., Tosca, J. et al. Disease severity and treatment requirements in familial inflammatory bowel disease. Int J Colorectal Dis 32, 1197–1205 (2017). https://doi.org/10.1007/s00384-017-2791-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-017-2791-y