Abstract
Introduction
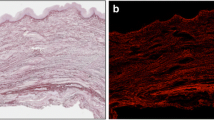
It is still an enigma that some patients develop rectal prolapse whilst others with similar risk factors do not. Biomechanical assessment of the skin may provide further insight into the aetiology of this complex condition. Elastin fibres are an abundant and integral part of many extracellular matrices and are especially critical for providing the property of elastic recoil to tissues. The significance of elastin fibres is clearly reflected by the numerous human conditions in which a skin phenotype occurs as a result of elastin fibre abnormalities.
Method
Between January and June 2013, skin specimens were obtained prospectively during surgery on 20 patients with rectal prolapse and 21 patients without prolapse undergoing surgery for other indications. Expression levels of elastin in the skin were measured by Orcein staining, and Image J. Tensile tests were performed using the Zwick Roell device, with custom ceramic clamps. For statistical analysis, Student’s t test was used.
Results
Histological analysis of prolapse vs control showed percentage dermal elastin fibres of 9 vs 5.8 % (p = 0.001) in males and 6.5 vs 5.3 % (p = 0.05) in females. Patients with more severe prolapse (external) had a significantly (p = 0.05) higher percentage dermal elastin fibres 6.9 vs 6.1 % than internal prolapse. Young’s modulus of patients with prolapse was lower in males (3.3 vs 2.8, p = 0.05) and females (3.1 vs 2.7, p = 0.05).
Conclusion
Patients with prolapse have a higher concentration of elastin fibres in the skin, and these differences are quantitatively demonstrated through mechanical testing. This suggests that the aetiology may be a result of a dysfunction of elastin fibre assembly.






Similar content being viewed by others
References
Jones OM, Cunningham C, Lindsey I (2011) The assessment and management of rectal prolapse, rectal intussusception, rectocoele, and enterocoele in adults. BMJ 342:c7099
Collinson R et al (2010) The emerging role of internal rectal prolapse in the aetiology of faecal incontinence. Gastroenterol Clin Biol 34(11):584–586
Harmston C et al (2011) The relationship between internal rectal prolapse and internal anal sphincter function. Colorectal Dis 13(7):791–795
Jan S, Hills RK, Gray R (2003) PROSPER: a uniquely flexible randomised controlled trial in rectal prolapse repair. Control Clin Trials 24:107–109
Keane DP et al (1997) Analysis of collagen status in premenopausal nulliparous women with genuine stress incontinence. Br J Obstet Gynaecol 104(9):994–998
Bo K et al (1994) Clinical and urodynamic assessment of nulliparous young women with and without stress incontinence symptoms: a case-control study. Obstet Gynecol 84(6):1028–1032
Arunkalaivanan AS et al (2009) Prevalence of urinary and faecal incontinence among female members of the Hypermobility Syndrome Association (HMSA). J Obstet Gynaecol 29(2):126–128
Jha S, Arunkalaivanan AS, Situnayake RD (2007) Prevalence of incontinence in women with benign joint hypermobility syndrome. Int Urogynecol J Pelvic Floor Dysfunct 18(1):61–64
Aydeniz A et al (2010) The relation between genitourinary prolapse and joint hypermobility in Turkish women. Arch Gynecol Obstet 281(2):301–304
Kerkhof MH, Hendriks L, Brolmann HA (2009) Changes in connective tissue in patients with pelvic organ prolapse—a review of the current literature. Int Urogynecol J Pelvic Floor Dysfunct 20(4):461–474
Reilly DJ et al (2008) Connective tissue disorder—a new subgroup of boys with slow transit constipation? J Pediatr Surg 43(6):1111–1114
Lin SY et al (2007) Changes in the extracellular matrix in the anterior vagina of women with or without prolapse. Int Urogynecol J Pelvic Floor Dysfunct 18(1):43–48
Beighton P (1988) Hypermobility scoring. Br J Rheumatol 27(2):163
Remvig L (2005) Generalised joint hypermobility and benign joint hypermobility syndrome. I: reproducibility and validity of tests and criteria. Ugeskr Laeger 167(47):4443–4448
Zarate N et al (2010) Unexplained gastrointestinal symptoms and joint hypermobility: is connective tissue the missing link? Neurogastroenterol Motil 22(3):252–e78
Holbrook KA, Byers PH (1989) Skin is a window on heritable disorders of connective tissue. Am J Med Genet 34(1):105–121
Jackson SR et al (1996) Changes in metabolism of collagen in genitourinary prolapse. Lancet 347(9016):1658–1661
Moalli PA et al (2005) Remodeling of vaginal connective tissue in patients with prolapse. Obstet Gynecol 106(5 Pt 1):953–963
Mosier E, Lin VK, Zimmern P (2010) Extracellular matrix expression of human prolapsed vaginal wall. Neurourol Urodyn 29(4):582–586
Marshman D et al (1987) Rectal prolapse: relationship with joint mobility. Aust N Z J Surg 57(11):827–829, 25
Fachinelli A, Trindade MR, Fachinelli FA (2011) Elastic fibers in the anterior abdominal wall. Hernia
Author information
Authors and Affiliations
Corresponding author
Additional information
H. M. Joshi and A. K. Woods are co-first authors.
Rights and permissions
About this article
Cite this article
Joshi, H.M., Woods, A.K., Smyth, E. et al. Histological and mechanical differences in the skin of patients with rectal prolapse. Int J Colorectal Dis 30, 1117–1122 (2015). https://doi.org/10.1007/s00384-015-2222-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-015-2222-x