Abstract
Purpose
This study aimed to define the controlled outcomes into adulthood for bowel function and lower urinary tract symptoms (LUTS) for males treated for low ARMs with individualized, minimally invasive approaches that preserve the native continence mechanisms as far as possible.
Methods
This is a single-institution, cross-sectional study. All males treated for low ARMs with cutback anoplasty, incision of anocutaneous membrane or dilatations based on the exact type of each malformation between 1983 and 2006 were invited to answer a detailed questionnaire on bowel function and LUTS. Each patient was matched to three controls representing the normal population. Ethical approval was obtained.
Results
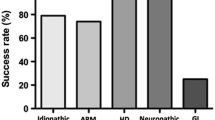
Amongst 46 respondents (67 %; median age 12.3 (5–29) years), overall fecal control was comparable to controls (p = NS). All patients had voluntary bowel movements; 98 % of patients and 97 % of controls were socially continent (p = NS); 67 % of patients and 64 % of controls were totally continent (p = NS). Constipation amongst patients (33 vs 3 % in controls; p < 0.0001) declined significantly with age. Outcomes by bowel function score were good in 85 %, satisfactory in 15 % and poor in 0 %. Prevalence of LUTS and age at completion of toilet training were comparable to controls (p = NS).
Conclusions
Our results support the adequacy and appropriateness of treating males with low ARMs with individualized, minimally invasive perineal procedures. Long-term functional outcomes comparable to controls are achieved in the majority, provided that constipation is effectively addressed.





Similar content being viewed by others
References
Pakarinen MP, Rintala RJ (2010) Management and outcome of low anorectal malformations. Pediatr Surg Int 26:1057–1063
Rintala RJ (1996) Anorectal malformations—management and outcome. Semin Neonatol 1:219–230
Levitt MA, Peña A (2005) Outcomes from the correction of anorectal malformations. Curr Opin Pediatr 17:394–401
Rintala RJ (2009) Congenital anorectal malformations—anything new? J Pediatr Gastroenterol Nutr 48:S79–S82
Chahine AA (2009) Imperforate anus and Hirschsprung’s disease. In: Evans SRT, Chahine AA (eds) Surgical pitfalls: prevention and management. Elsevier Saunders Publ, Philadelphia, pp 827–839, chapter 81
Pakarinen MP, Goyal A, Koivusalo A, Baillie C, Turnock R, Rintala RJ (2006) Functional outcome in correction of perineal fistula in boys with anoplasty versus posterior sagittal anorectoplasty. Pediatr Surg Int 22:961–965
Rintala RJ, Lindahl HG (1995) Is normal bowel function possible after repair of intermediate and high anorectal malformations? J Pediatr Surg 30:491–494
Rintala RJ, Lindahl HG, Rasanen M (1997) Do children with repaired low anorectal malformations have normal bowel function? J Pediatr Surg 32:823–826
Kyrklund K, Koivusalo A, Rintala RJ, Pakarinen MP (2012) Evaluation of bowel function and fecal continence in 594 Finnish individuals aged 4–26 years. Dis Col Rect 55:671–676
Kyrklund K, Taskinen S, Rintala RJ, Pakarinen MP (2012) Lower urinary tract symptoms from childhood to adulthood: a population-based study of 594 Finnish individuals 4 to 26 years old. J Urol 188:588–593
Schou J, Poulsen AL, Nordling J (1993) The value of a new symptoms score (DAN-PSS) in diagnosing uro-dynamic infravesical obstruction in BPH. Scand J Urol Nephrol 27:489–492
Malone PS, Ransley PG, Kiely EM (1990) Preliminary report: the antegrade continence enema. Lancet 336:1217–1218
Pakarinen MP, Rintala RJ (2010) Management and outcome of low anorectal malformations. Pediatr Surg Int 26:1057–1063
Pakarinen MP, Baillie C, Koivusalo A, Rintala RJ (2006) Transanal endoscopic-assisted proctoplasty—a novel surgical approach for individual management of patients with imperforate anus without fistula. J Pediatr Surg 41:314–317
Pena A (1988) Posterior sagittal anorectoplasty: results in the management of 332 cases of anorectal malformations. Pediatr Surg Int 3:94–104
Yeung CK, Kiely EM (1991) Low anorectal anomalies: a critical appraisal. Pediatr Surg Int 6:333–335
Pakarinen MP, Koivusalo A, Lindahl H, Rintala RJ (2007) Prospective controlled long-term follow-up for functional outcome after anoplasty for boys with perineal fistula. J Pediatr Gastroenterol Nutr 44:436–439
Jarvi K, Laitakari EM, Koivusalo A, Rintala RJ, Pakarinen MP (2010) Bowel function and gastrointestinal quality of life among adults operated for Hirschsprung disease during childhood: a population-based study. Ann Surg 252:977–981
Peña A (1995) Anorectal malformations. Semin Pediatr Surg 3:105–109
Lombardi L, Bruder E, Caravaggi F, Del Rossi C, Martucciello G (2013) Abnormalities in “low” anorectal malformations (ARMs) and functional results resecting the distal 3 cm. J Pediatr Surg 48:1294–1300
Rintala R, Lindahl H, Sariola H, Rapola J, Louhimo I (1990) The rectourogenital connection in anorectal malformations is an ectopic anal canal. J Pediatr Surg 25:665–668
Acknowledgments
The authors wish to thank nurse E. Tenhovuori and paediatric radiologist Dr R. Kivisaari from our institution for assistance with logistical aspects and review of sacral imaging, respectively.
Conflicts of interest
None to declare
Sources of funding
This research was supported by grants from the Finnish Medical Foundation, Foundation for Pediatric Research (Finland), and the Päivikki and Sakari Sohlberg Foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kyrklund, K., Pakarinen, M.P., Taskinen, S. et al. Bowel function and lower urinary tract symptoms in males with low anorectal malformations: an update of controlled, long-term outcomes. Int J Colorectal Dis 30, 221–228 (2015). https://doi.org/10.1007/s00384-014-2074-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-014-2074-9