Abstract
Purposes
The present study was designed to evaluate the prognostic value of the perioperative neutrophil-to-lymphocyte ratio (NLR) for the long-term survival in patients with colorectal cancer.
Methods
This was a retrospective study of 524 patients with histologically proven stage II or III colorectal cancer who underwent curative colorectal resection. We classified patients into a low NLR group or high NLR group base on their NLR values at three time points (before surgery (Pre), on the first postoperative day (POD1), and on the third or fourth postoperative day (POD3)) and evaluated the survival according to the group.
Results
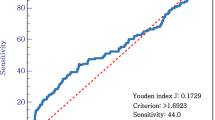
The cancer-specific survival was significantly longer in the groups with a low NLR on POD3. The disease-free survival was significantly longer in the group with a low NLR on Pre. We subsequently allocated a score of 1 to patients with a high NLR at each point and reclassified patients into those with a low perioperative NLR group (score of 0 or 1) and high perioperative NLR group (score of 2 or 3). Both the cancer-specific survival and disease-free survival rates were significantly different between the two perioperative NLR groups. Both univariate and multivariate analyses demonstrated that being in the high perioperative NLR group was an independent risk factor for both the cancer-specific survival and disease-free survival.
Conclusions
Not only the preoperative but also the postoperative NTR is thus considered to be a predictor of the long-time survival in patients with colorectal cancer.





Similar content being viewed by others
References
DerHagopian RP, Sugarbaker EV, Ketcham A (1978) Inflammatory oncotaxis. JAMA 240:374–375
Balkwill F, Mantovani A (2001) Inflammation and cancer: back to Virchow? Lancet 357:539–545
Coussens LM, Werb Z (2002) Inflammation and cancer. Nature 420:860–867
Grivennikov SI, Greten FR, Karin M (2010) Immunity, inflammation, and cancer. Cell 140:883–899
Little D, Regan M, Keane RM, Bouchier-Hayes D (1993) Perioperative immune modulation. Surgery 114:87–91
Tsuchiya Y, Sawada S, Yoshioka I, Ohashi Y, Matsuo M, Harimaya Y, Tsukada Y, Saiki I (2003) Increased surgical stress promotes tumor metastasis. Surgery 133:547–555
Hiki N, Shimizu N, Yamaguchi H, Imamura K, Kami K, Kubota K, Kaminishi M (2006) Manipulation of the small intestine as a cause of the increased inflammatory response after open compared with laparoscopic surgery. Br J Surg 93:195–204
Luk JM, Tung PH, Wong KF, Chan KL, Law S, Wong J (2009) Laparoscopic surgery induced interleukin-6 levels in serum and gut mucosa: implications of peritoneum integrity and gas factors. Surg Endosc 23:370–376
Shiromizu A, Suematsu T, Yamaguchi K, Shiraishi N, Adachi Y, Kitano S (2000) Effect of laparotomy and laparoscopy on the establishment of lung metastasis in a murine model. Surgery 128:799–805
Pera M, Nelson H, Rajkumar SV, Young-Fadok TM, Burgat LJ (2003) Influence of postoperative acute-phase response on angiogenesis and tumor growth: open vs. laparoscopic-assisted surgery in mice. J Gastrointest Surg 7:783–790
Evans C, Galustian C, Kumar D, Hagger R, Melville DM, Bodman-Smith M, Jourdan I, Gudgeon AM, Dalgleish AG (2009) Impact of surgery on immunologic function: comparison between minimally invasive techniques and conventional laparotomy for surgical resection of colorectal tumors. Am J Surg 197:238–245
Proctor MJ, Morrison DS, Talwar D, Balmer SM, Fletcher CD, O’Reilly DS, Foulis AK, Horgan PG, Mcmillan DC (2011) A comparison of inflammation-based prognostic scores in patients with cancer. A Glasgow Inflammation Outcome Study. Eur J Cancer 47:2633–2641
Kwon HC, Kim SH, Oh SY, Lee S, Lee JH, Choi HJ, Park KJ, Roh MS, Kim SG, Kim HJ, Lee JH (2012) Clinical significance of preoperative neutrophil-lymphocyte versus platelet-lymphocyte ratio in patients with operable colorectal cancer. Biomarkers 17:216–222
Mallappa S, Sinha A, Gupta S, Chadwick SJ (2013) Preoperative neutrophil to lymphocyte ratio >5 is a prognostic factor for recurrent colorectal cancer. Color Dis 15:323–328
Malietzis G, Giacometti M, Askari A, Nachiappan S, Kennedy RH, Faiz OD, Aziz O, Jenkins JT (2013) A preoperative neutrophil to lymphocyte ratio of 3 predicts disease-free survival after curative elective colorectal cancer surgery. Ann Surg. Epub ahead of print
Chiang SF, Hung HY, Tang R, Changchien CR, Chen JS, You YT, Chiang JM, Lin JR (2012) Can neutrophil-to-lymphocyte ratio predict the survival of colorectal cancer patients who have received curative surgery electively? Int J Color Dis 27:1347–1357
Zahorec R (2001) Ratio of neutrophil to lymphocyte counts—rapid and simple parameter of systemic inflammation and stress in critically ill. Bratisl Lek Listy 102:5–14
Sobin LH, Compton CC (2010) TNM seventh edition: what’s new, what’s changed: communication from the International Union Against Cancer and the American Joint Committee on Cancer. Cancer 116:5336–5339
Petrelli N, Douglass HO Jr, Herrera L, Russell D, Stablein DM, Bruckner HW, Mayer RJ, Schinella R, Green MD, Muggia FM et al (1989) The modulation of fluorouracil with leucovorin in metastatic colorectal carcinoma: a prospective randomized phase III trial. Gastrointestinal Tumor Study Group. J Clin Oncol 7:1419–1426
Poon MA, O'Connell MJ, Wieand HS, Krook JE, Gerstner JB, Tschetter LK, Levitt R, Kardinal CG, Mailliard JA (1991) Biochemical modulation of fluorouracil with leucovorin: confirmatory evidence of improved therapeutic efficacy in advanced colorectal cancer. J Clin Oncol 9:1967–1972
Douillard JY, Hoff PM, Skillings JR, Eisenberg P, Davidson N, Harper P, Vincent MD, Lembersky BC, Thompson S, Maniero A, Benner SE (2002) Multicenter phase III study of uracil/tegafur and oral leucovorin versus fluorouracil and leucovorin in patients with previously untreated metastatic colorectal cancer. J Clin Oncol 20:3605–3616
Kishi Y, Kopetz S, Chun YS, Palavecino M, Abdalla EK, Vauthey JN (2009) Blood neutrophil-to-lymphocyte ratio predicts survival in patients with colorectal liver metastases treated with systemic chemotherapy. Ann Surg Oncol 16:614–622
Zhang Y, Peng Z, Chen M, Liu F, Huang J, Xu L, Zhang Y, Chen M (2012) Elevated neutrophil to lymphocyte ratio might predict poor prognosis for colorectal liver metastasis after percutaneous radiofrequency ablation. Int J Hyperth 28:132–140
Motomura T, Shirabe K, Mano Y, Muto J, Toshima T, Umemoto Y, Fukuhara T, Uchiyama H, Ikegami T, Yoshizumi T, Soejima Y, Maehara Y (2013) Neutrophil-lymphocyte ratio reflects hepatocellular carcinoma recurrence after liver transplantation via inflammatory microenvironment. J Hepatol 58:58–64
Okano K, Maeba T, Moroguchi A, Ishimura K, Karasawa Y, Izuishi K, Goda F, Usuki H, Wakabayashi H, Maeta H (2003) Lymphocytic infiltration surrounding liver metastases from colorectal cancer. J Surg Oncol 82:28–33
Jass JR (1986) Lymphocytic infiltration and survival in rectal cancer. J Clin Pathol 39:585–589
Kusumanto YH, Dam WA, Hospers GA, Meijer C, Mulder NH (2003) Platelets and granulocytes, in particular the neutrophils, form important compartments for circulating vascular endothelial growth factor. Angiogenesis 6:283–287
Park BK, Paik YH, Park JY, Park KH, Bang S, Park SW, Chung JB, Park YN, Song SY (2006) The clinicopathologic significance of the expression of vascular endothelial growth factor-C in intrahepatic cholangiocarcinoma. Am J Clin Oncol 29:138–142
Law WL, Choi HK, Lee YM, Ho JW, Seto CL (2007) Anastomotic leakage is associated with poor long-term outcome in patients after curative colorectal resection for malignancy. J Gastrointest Surg 11:8–15
Tsujimoto H, Ichikura T, Ono S, Sugasawa H, Hiraki S, Sakamoto N, Yaguchi Y, Yoshida K, Matsumoto Y, Hase K (2009) Impact of postoperative infection on long-term survival after potentially curative resection for gastric cancer. Ann Surg Oncol 16:311–318
Mirnezami A, Mirnezami R, Chandrakumaran K, Sasapu K, Sagar P, Finan P (2011) Increased local recurrence and reduced survival from colorectal cancer following anastomotic leak: systematic review and meta-analysis. Ann Surg 253:890–899
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kubo, T., Ono, S., Ueno, H. et al. Impact of the perioperative neutrophil-to-lymphocyte ratio on the long-term survival following an elective resection of colorectal carcinoma. Int J Colorectal Dis 29, 1091–1099 (2014). https://doi.org/10.1007/s00384-014-1964-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-014-1964-1