Abstract
Purpose
Laparoscopic surgery in the treatment of colon carcinoma causes pH value alterations as well as changes in fibrinolytic activity. This results in enhanced proliferation of colon carcinoma cells in vitro and also in enhanced growth of liver metastasis when compared to isobaric (gasless) laparoscopy in vivo. So far, the direct influence of CO2 pneumoperitoneum on the invasiveness and metastatic capabilities of colon cancer cells remains unclear. We therefore evaluated transcripts of the uPA system.
Methods
The influence of CO2 pneumoperitoneum on the gene expression of plasminogen activator inhibitor-1 (PAI-1), urokinase-type plasminogen activator (uPA), and tissue-type plasminogen activator (tPA) was investigated in colon carcinoma cell lines (HT116, SW48, and WiDr) and mesothelial cells employing a pneumoperitoneum chamber in vitro. Quantitative gene expression data were collected using real-time RT-PCR and statistical analysis was performed by means of analysis of variance and Bonferroni correction.
Results
The expression of uPA and PAI-1 was increased in colon carcinoma cell lines when cultivated at pH 6.1, a value corresponding to intraabdominal pH values during CO2 insufflation. Elevated PAI-1 mRNA levels were also observed when CO2 was simultaneously applied with a pressure of 10 mmHg. In contrast, there were no significant changes in mesothelial cells in the investigated parameter.
Conclusion
The conditions of CO2 pneumoperitoneum cause changes in the expression of genes controlling the fibrinolytic activity. The increase of PAI-1 and uPA can contribute to the enhancement of metastasis and invasive potential of tumour cells. Therefore, changes in the conditions of laparoscopy may well optimise laparoscopic therapy in colon cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although there has been a steady increase in the number of laparoscopic colorectal resections of malignant disease since the mid-1990s, minimally invasive procedures were more commonly performed for benign conditions. In this context, the literature refers to the increased proliferation of tumour cells in vitro under CO2 pneumoperitoneum conditions [1] as well as enhanced growth of liver metastases compared to isobaric (gasless) laparoscopy in vivo [2]. Therefore, the question has to be addressed as to whether CO2 pneumoperitoneum may be directly or indirectly related to the enhanced invasion and metastatic capabilities of colon cancer cells and to what extent the fibrinolytic system is involved in this process.
During surgery, the intraperitoneal fibrinolytic activity of the plasminogen activator system plays a pivotal role in the maintenance of intraperitoneal fibrinolysis and in the formation of postoperative adhesions. Moreover, the urokinase plasminogen activator (uPA) system is intimately implicated in tumour cell interaction with the extracellular matrix (ECM) and mesothelial cells, both being essential to tumour progression. The uPA system is based on the serine protease plasmin, their activators tissue-type plasminogen activator (tPA) and urokinase-type plasminogen activator (uPA), as well as the plasminogen activator inhibitors PAI-1 and PAI-2 [3]. tPA and uPA effect proteolysis by converting plasminogen to plasmin.
Abdominal insufflation with CO2 causes severe trauma leading to disintegration of the peritoneal mesothelium, which is covered by monolayer mesothelial cells. Electron microscopic investigations revealed morphological changes of the peritoneum under laparoscopic conditions such as high infiltration of granulocytes [4]. Furthermore, changes in pressure, pH shifts, or dehydration effects may also result in functional impairment. The literature reports only few experimental data on the evaluation of intraperitoneal fibrinolytic activity under laparoscopic conditions. The findings of these studies are controversial [5–8] and focus on the peritoneum with regard to peritoneal healing and the development of clinically relevant postoperative adhesions. However, the effect of pneumoperitoneum on the uPA system has severe consequences for tumour cell progression. Plasmin displays an extended substrate spectrum and degrades fibrin as well as a large number of ECM proteins such as fibronectin or vitronectin. In addition, plasmin activates several metalloproteinases and these in turn degrade ECM, a crucial requirement for activating the metastatic cascade. Proteolysis, effective tumour cell invasion, and metastatic dispersal depend on the balance of the uPA system. In this context, it was recently demonstrated that expression levels of uPA and PAI-1 correlate with the prognosis of bronchial [9], ovarian [10], endometrial cancer [11], breast [12], gastric [13–15], and colon carcinomas [16–24]. CO2 insufflation influences essential cell functions of colon carcinoma cells such as intra- and extracellular pH values, intracellular calcium levels, and the oxygen partial pressure in the surrounding tissue. Wildbrett et al. [25, 26] demonstrated an evident intra- and extracellular increase in the pH value from 7.4 to 6.2 due to CO2 application leading to acidification. Small numbers of emerging protons can be buffered, whereas higher concentrations lower intra- and extracellular pH values. The decrease in intracellular pH values leads to a series of physiological changes relating to the respiratory chain [27], mitotic activity [28], as well as the secretion of cytokines and inflammation mediators [29]. Additionally, the increased intracellular proton concentration influences the calcium influx into the cell [30]. Even submicromolar increments cause maximum stimulation of calcium-dependent signal transduction pathways [31]. Elevated intracellular calcium levels increase gene transcription [32], stimulation of mitosis [33–35], as well as cell migration, enhance transcellular ion transport, neurotransmitter release, acid secretion, and several other cell functions [36].
Previous investigations demonstrated that mechanical deformation of the human colon carcinoma cell line HCT116 causes an increased expression of PAI-1 [37]. Such a deformation of tumour cells following insufflation with CO2 and the subsequent increase in intraabdominal pressure during laparoscopy might be conceivable. Nevertheless, there are no studies on the effect of pneumoperitoneum on the expression of PAI-1 or uPA in tumour cells so far.
The aim of the present study was to evaluate the effect of CO2 pressure and pH shifts on the expression of uPA, tPA and PAI in colon cancer cells and mesothelial cells.
Material and methods
Materials
Unless specified otherwise, all chemicals and reagents were supplied by Sigma–Aldrich (Deisenhofen, Germany). Petri dishes and culture flasks were obtained from Sarstedt (Nuremberg, Germany). Antibiotics were supplied by PAA (Linz, Austria), and PBS (10×), HBSS (10×) and trypsin by Invitrogen (Karlsruhe, Germany).
Tumour cell lines
Human colon carcinoma cell lines WiDr, HCT116 and SW48 (ATCC, Manassas, USA) were routinely cultured on gelatine-coated (0.2%) 25-cm² culture flasks in RPMI supplemented with 10% FCS, 1% penicillin/streptomycin at 37°C and 5% CO2 in a humidified incubator. Cells were trypsinized when obtaining 75% confluence and distributed to 18 Petri dishes (Ø 3.5 cm). Experiments were performed in the pneumoperitoneum chamber when 75% confluency was once more achieved. All colon carcinoma cell lines were derived from primary colon tumours.
Mesothelial cells
Experiments were approved by the local ethics committee. Human mesothelial cells were isolated from omental adipose tissue according to the protocol of Ivarsson et al. [38] with minor modifications. A 5 × 5-cm² (approx. 10 g) tissue biopsy was washed in 50 ml HBSS, following incubation in HBSS supplemented with 0.05% trypsin–EDTA. Tissue was slightly shaken for 10 min in 37°C and flushed immediately with RPMI supplemented with 20% FCS to neutralise enzyme activity and to aid in detachment. Cell suspensions were centrifuged for 10 min at 260×g and cultivated in M199 (Gibco, Eggenstein, Germany) +20% FCS + 1% penicillin/streptomycin at 37°C and 5% CO2 in a humidified incubator. The cells were seeded on gelatine-coated (0.2%) 25-cm² culture flasks. One week later, cells were trypsinized and disseminated in 18 Petri dishes (Ø 3.5 cm). Experiments were performed following achievement of 75% confluent cell growth. For immunohistological characterisation, the primary monoclonal antibodies (DAKO, Glostrup) CK7 (clone OV-TL 12/30), CK8 LMV (clone 35βH11), CK18 (clone DC10) and CK19 (clone RCK108) were used in a 1:100 dilution [39]. Data of mesothelial cell experiments were gathered from four different patients.
In vitro pneumoperitoneum/experimental design
Tumour cells and similarly mesothelial cells were incubated under three different conditions.
Experimental set 1 (pH 6.1 + CO2) was performed in Petri dishes placed inside a Perspex chamber and incubated at a CO2 pressure of 10 mmHg and a continuous gas flow of 2.5 l/min. The settings of CO2 pneumoperitoneum were mimicked in vitro by an airtight Perspex chamber (26 × 26 × 7 cm) with one influx for the application of humidified CO2 and two ports to measure gas pressure and saturation, respectively. The pneumoperitoneum chamber was located in an incubator set at 37°C. Prior to incubation in the chamber, medium was equilibrated for 1 h to CO2 and pH was adjusted to 6.1. After 0.5, 1, 2, and 5 h of incubation in a 99.5% CO2 atmosphere, samples were harvested.
Experimental set 2 (pH 6.1) was performed in a standard cell incubator (5% CO2 atmosphere) and again pH was adjusted to 6.1. Under these conditions, the cells were harvested again after 0.5, 1, 2, and 5 h of incubation.
Set 3 (pH 7.4) served as control with cells incubated in a standard cell incubator and physiological pH of 7.4.
RNA extraction and real-time reverse transcription polymerase chain reaction analysis
Total RNA was isolated by RNeasy Mini Kit (Qiagen, Hilden, Germany) according to the manufacturer’s instructions and stored at −80°C.
Concentration and integrity of the total RNA were analysed on a RNA Nano LabChip® Kit (Agilent Technologies, Waldbronn, Germany). Reverse transcription polymerase chain reactions (RT-PCRs) were performed with one-step RT-PCR Kit (Qiagen, Hilden, Germany). Gene expression was quantified using an iCycler iQ real-time detection system (BioRad, Munich, Germany). Amplification was performed using the following intron-spanning primers: PAI-1 forward primer, 5′-CTG ACT TCA CGA GTC TTT CAG ACC-3′; PAI-1 reverse primer, 5′-CCC ATG AAA AGG ACT GTT CCT GTG-3′; uPA forward primer 5′-AGA ATT CAC CAC CAT CGA GA-3′; uPA reverse primer, 5′-ATC AGC TTC ACA ACA GTC AT-3′; tPA forward primer, 5′-CAT AAG GAA TTC GAT GAT GAC ACT TAC GAC-3′ and tPA reverse primer, 5′-GAC TGT TCT GTT AAG TAA ATG TTG TGA TGT-3′.
For quantification, the standard curves were established with gene-specific standard cRNA in tenfold dilution series of 0.01 to 1,000 attomol instead of total RNA. The standard curves were generated individually for all genes investigated, and data were calculated by iCycler iQ real-time detection system software (BioRad).
Statistical analysis
The expression of PAI, uPA and tPA was analysed in an ANOVA model using the statistical software package SAS (Proc Mixed). In the analysis of tumour cell lines, all lines HCT116, SW48, and WiDr were included simultaneously in one analysis. In a second analysis, the mesothelial cells of four patients were investigated together. Two models were investigated for both data sets: (1) experimental set 1 (pH 6.1 + CO2) versus control set (pH 7.4) and (2) experimental set 2 (pH 6.1) versus control set (pH 7.4). The time effect in the ANOVA analysis was modelled with five levels identifying the control with time 0 h and including four time points for the experimental sets (0.5, 1, 2, and 5 h). Four pairwise comparisons were performed between the control and each time point of the experimental set using a Bonferroni-adjusted significance level of 0.0125 (= 0.05/4).
In the analysis of tumour cell lines, the PCR was replicated twice for PAI and uPA. These two replications were considered as a random factor nested under the fixed factor cell line. For tPA, the PCR was not replicated, thus, effects of the cell line and the variability produced by the replication of the PCR could not be separated and the cell line was modelled as a random factor. In the analysis of mesothelial cells, the patient was analogously considered as a random factor. All possible fixed and random interaction terms were included in the analysis. Triplets were measured for each PCR and time point (three readings). The ANOVA models were based on the logarithmic expression values. The expression ratio between two groups averaged over the cell lines or patients was estimated by taking the exponential of the mixed model estimates for the logarithmic differences.
Results
Mesothelial cells
Cultured cells appeared in a flat “cobblestone” pattern and grew to a confluence of 75% of the dish surface within 1 week. Cells cultured on plastic slides were immunoreactive using antibodies detecting CK8, CK18, and CK19 which are known to be characteristic for mesothelial cells (data not shown) [39]. The cells did not reveal any staining when using the anti-fibroblast antibody (Dianova100, clone 5B5, MO877, Glostrup, Denmark) [38].
No significant differences were found in the expression of PAI-1, tPA and uPA between experimental set 2 (pH 6.1) and set 1 (pH 6.1 + CO2) compared to the control sets (pH 7.4; data not shown).
Colon carcinoma cell lines
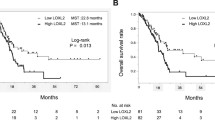
PAI-1 expression increased markedly in all colon carcinoma cell lines (HT116, SW48 and WiDr) in both experimental sets 2 (pH 6.1) and 1 (pH 6.1 + CO2) within 5 h of incubation compared to the control set (pH 7.4; Fig. 1). The increase of PAI-1 expression in experimental set 1 (pH 6.1 + CO2) was inhibited noticeably at every point in time compared to experimental set 2 (pH 6.1). Insufflation with CO2 diminished the expression of PAI-1 compared to experimental set 2 (pH 6.1, without CO2).
Variance analysis of the pooled colon carcinoma cell lines revealed significant differences (p < 0.0125) in PAI-1 expression during an observation period from 2 h (p = 0.0013) to 5 h (p = 0.0018) in experimental set 2 (pH 6.1) compared to the control set (pH 7.4). There was a significant increase in PAI-1 expression after 5 h incubation in set 1 (pH 6.1 + CO2) compared to the control set (pH 7.4) as well (p = 0.0001; Table 1). Whereas PAI-1 expression in set 1 (pH 6.1 + CO2) did not increase significantly before 5 h, the absence of CO2 resulted in a significant increase as early as 2 h.
Moreover, uPA expression increased in experimental set 2 (pH 6.1) after 5 h incubation compared to the control set (pH 7.4; Fig. 2). This increase was not observed in set 1. Here, no change in uPA expression was observed compared to the control set.
Variance analysis of pooled cancer cell lines revealed a significant increase in uPA expression in set 2 after 5 h (p = 0.0039; Table 2). No significant changes were observed in set 1. Here, insufflation with CO2 inhibited the expression of the plasmin activator uPA.
The tPA expression of the colon carcinoma cell lines in experimental sets 1 and 2 did not exhibit any significant differences when compared to the control set (data not shown).
Furthermore, none of the analyses demonstrated systematically different expression curves for the three tumour cell lines since no interaction between time and cell line was observed.
Discussion
For the first time, this study investigates the changes in gene expression in the plasmin activator system of colon carcinoma cells as well as mesothelial cells under the conditions of CO2 pneumoperitoneum.
Interestingly, PAI-1 expression is significantly enhanced in colon carcinoma cells when exposed to pH 6.1 and a CO2 pressure of 10 mmHg within 5 h (Fig. 1). Without CO2 insufflation, the increase in PAI-1 expression is always greater. The same changes are observed for uPA expression. Here, the lower pH enhances uPA expression significantly compared to the control group. However, simultaneous exposure to CO2 has no effect on uPA expression. The acid pH seems to induce enhanced PAI-1 and uPA expression, but additional CO2 pressure inhibits this effect (Figs. 1 and 2). Variance analysis of the tumour cell lines revealed significant differences (p < 0.0125) with respect to PAI-1 expression in the analysed groups (pH 6.1 and pH 6.1 + CO2) compared to the control group (pH 7.4) within 2 h (Table 1). There is also a significant increase in uPA expression (Table 2) in the same tumour cell lines under acid conditions within a time interval of 5 h.
Therefore, it appears likely that the increase in PAI-1 and uPA expression is caused by acid pH 6.1, a value which matches the intraabdominal conditions during laparoscopic surgery with CO2 insufflation [26]. The inhibition of PAI-1 and uPA expression employing CO2 is confirmed by variance analysis. Additional experiments are warranted to establish the molecular mechanisms of these findings. No significant differences were documented for the tPA expression of the tested colon carcinoma cell lines in the experimental sets 1 (pH 6.1 + CO2) and 2 (pH 6.1) compared to the control set.
In contrast to tumour cells, the expression of PAI-1, uPA, and tPA in the mesothelial cells revealed no significant differences when compared to the control. These results are confirmed by a prospective randomised study by Neudecker et al. [8] who did not observe any significant differences in uPA, tPA, and PAI-1 expression in peritoneal mesenthelium during laparoscopic colon resection when compared with conventional surgery.
PAI-1 as well as uPA is described to be an important promoter of tumour cell invasion and metastatic spread [40–42]. The antagonist PAI-1 protects the matrix framework, which is required for tumour cell adhesion and migration, against the proteolytic uPA [43, 44], as well as the tumour cells themselves against excessive degradation [45]. Similarly, the main mechanism of PAI-1 is independent of the direct function as an inhibitor of the protease uPA in the plasmin activator system [41, 42]. PAI-1 modulates the interaction between the uPA receptor CD87 coupled to tumour cells and vitronectin [40, 41] as well as the connection between vitronectin and the cellular integrin αvβ3 [42]. Therefore, tumour cell adhesion on the cellular matrix is impaired and as a result, tumour cell migration as well as metastatic progression is promoted [46]. Thus, our findings of enhanced expression of PAI-1 in colon cancer cell lines suggest an increase in the invasive potential of colon carcinoma cells under the conditions of prolonged laparoscopic surgery with CO2 insufflation.
Previous studies have emphasised the clear increase in PAI expression in colon carcinoma cells compared to unaffected epithelium [21, 23, 47, 48]. Sier et al. [48] demonstrated a tenfold increase in PAI-1 levels and a two- to threefold enhanced PAI-2 level for colonic adenocarcinoma compared to normal colon epithelium. Several authors confirmed a correlation between the level of PAI-1 expression and the prognosis of the 3-year survival rate of patients [17, 18]. Moreover, the PAI-1 expression correlates with the state of differentiation and the infiltration depth of the tumour [16].
Although randomised prospective long-term studies have not revealed any significant survival disadvantage for patients with colon carcinoma after laparoscopic colon carcinoma resection in comparison with conventional surgery, optimisation of the laparoscopic conditions is still desirable from an oncological point of view. Therefore, we hope that this study will encourage the consideration of potential hazards in the process of improving laparoscopic surgery.
References
Jacobi CA, Sabat R, Bohm B, Zieren HU, Volk HD, Müller JM (1997) Pneumoperitoneum with carbon dioxide stimulates growth of malignant colonic cells. Surgery 121:72–78
Gutt CN, Kim ZG, Schemmer P, Krähenbühl L, Schmedt CG (2002) Impact of laparoscopic and conventional surgery on Kupffer cells, tumor-associated CD44 expression, and intrahepatic tumor spread. Arch Surg 137(12):1408–1412
Li WY, Chong SS, Huang EY, Tuan TL (2003) Plasminogen activator/plasmin system: a major player in wound healing? Wound Repair Regen 11:239–247
Volz J, Köster S, Weiss M, Schmidt R, Urbaschek R, Melchert F, Albrecht M (1996) Pathophysiologic features of a pneumoperitoneum at laparoscopy: a swine model. Am J Obstet Gynecol 174:132–140
Kopernik G, Avinoach E, Grossman Y, Levy R, Yulzari R, Rogachev B, Douvdevani A (1998) The effect of a high partial pressure of carbon dioxide environment on metabolism and immune functions of human peritoneal cells: relevance to carbon dioxide pneumoperitoneum. Am J Obstet Gynecol 179:1503–1510
Bergstrom M, Ivarsson ML, Holmdahl L (2002) Peritoneal response to pneumoperitoneum and laparoscopic surgery. Br J Surg 89:1465–1469
Nagelschmidt M, Gerbecks D, Minor T (2001) The impact of gas laparoscopy on abdominal plasminogen activator activity. Surg Endosc 15:585–588
Neudecker J, Junghans T, Ziemer S, Raue W, Schwenk W (2002) Effect of laparoscopic and conventional colorectal resection on peritoneal fibrinolytic capacity: a prospective randomized clinical trial. Int J Colorectal Dis 17:426–429
Pedersen H, Grondahl-Hansen J, Francis D, Osterlind K, Hansen HH, Dano K, Brunner N (1994) Urokinase and plasminogen activator inhibitor type 1 in pulmonary adenocarcinoma. Cancer Res 54:120–123
Kuhn W, Schmalfeldt B, Reuning U, Pache L, Berger U, Ulm K, Harbeck N, Spathe K, Dettmar P, Höfler H, Janicke F, Schmitt M, Graeff H (1999) Prognostic significance of urokinase (uPA) and its inhibitor PAI-1 for survival in advanced ovarian carcinoma stage FIGO IIIc. Br J Cancer 79:1746–1751
Köhler U, Hiller K, Martin R, Langanke D, Naumann G, Bilek K, Janicke F, Schmitt M (1997) Tumor-associated proteolytic factors uPA and PAI-1 in endometrial carcinoma. Gynecol Oncol 66:268–274
Foekens JA, Look MP, Peters HA, van Putten WL, Portengen H, Klijn JG (1995) Urokinase-type plasminogen activator and its inhibitor PAI-1: predictors of poor response to tamoxifen therapy in recurrent breast cancer. J Natl Cancer Inst 87:751–756
Nekarda H, Schmitt M, Ulm K, Wenninger A, Vogelsang H, Becker K, Roder JD, Fink U, Siewert JR (1994) Prognostic impact of urokinase-type plasminogen activator and its inhibitor PAI-1 in completely resected gastric cancer. Cancer Res 54:2900–2907
Heiss MM, Babic R, Allgayer H, Gruetzner KU, Jauch KW, Loehrs U, Schildberg FW (1995) Tumor-associated proteolysis and prognosis: new functional risk factors in gastric cancer defined by the urokinase-type plasminogen activator system. J Clin Oncol 13:2084–2209
Plebani M, Herszenyi L, Cardin R, Roveroni G, Carraro P, Paoli MD, Rugge M, Grigioni WF, Nitti D, Naccarato R (1995) Cysteine and serine proteases in gastric cancer. Cancer 76:367–375
Papadopoulou S, Scorilas A, Yotis J, Arnogianaki N, Plataniotis G, Agnanti N, Talieri M (2002) Significance of urokinase-type plasminogen activator and plasminogen activator inhibitor-1 (PAI-1) expression in human colorectal carcinomas. Tumour Biol 23:170–178
Loktionov A, Watson MA, Stebbings WS, Speakman CT, Bingham SA (2003) Plasminogen activator inhibitor-1 gene polymorphism and colorectal cancer risk and prognosis. Cancer Lett 189:189–196
Berger DH (2002) Plasmin/plasminogen system in colorectal cancer. World J Surg 26:767–771
Garcia-Avello A, Galindo-Alvarez J, Martinez-Molina E, Cesar-Perez J, Navarro JL (2001) Coagulative system activation and fibrinolytic system inhibition activities arise from tumoral draining vein in colon carcinoma. Thromb Res 104:421–425
Schwarte-Waldhoff I, Klein S, Blass-Kampmann S, Hintelmann A, Eilert C, Dreschers S, Kalthoff H, Hahn SA, Schmiegel W (1999) DPC4/SMAD4 mediated tumor suppression of colon carcinoma cells is associated with reduced urokinase expression. Oncogene 18:3152–3158
Miseljic S, Galandiuk S, Myers SD, Wittliff JL (1995) Expression of urokinase-type plasminogen activator and plasminogen activator inhibitor in colon disease. J Clin Lab Anal 9:413–417
Fujii T, Obara T, Tanno S, Ura H, Kohgo Y (1999) Urokinase-type plasminogen activator and plasminogen activator inhibitor-1 as a prognostic factor in human colorectal carcinomas. Hepatogastroenterology 46:2299–2308
Buo L, Lyberg T, Jorgensen L, Johansen HT, Aasen AO (1993) Location of plasminogen activator (PA) and PA inhibitor in human colorectal adenocarcinomas. APMIS 101:235–241
Herszenyi L, Plebani M, Carraro P, De Paoli M, Roveroni G, Cardin R, Tulassay Z, Naccarato R, Farinati F (1999) The role of cysteine and serine proteases in colorectal carcinoma. Cancer 86:1135–1142
Wildbrett P, Oh A, Naundorf D, Volk T, Jacobi CA (2003) Impact of laparoscopic gases on peritoneal microenvironment and essential parameters of cell function. Surg Endosc 17:78–82
Kuntz C, Wunsch A, Bodeker C, Bay F, Rosch R, Windeler J, Herfarth C (2000) Effect of pressure and gas type on intraabdominal, subcutaneous, and blood pH in laparoscopy. Surg Endosc 14:367–371
Simchowitz L (1985) Intracellular pH modulates the generation of superoxide radicals by human neutrophils. J Clin Invest 76:1079–1089
Shrode LD, Tapper H, Grinstein S (1997) Role of intracellular pH in proliferation, transformation, and apoptosis. J Bioenerg Biomembr 29:393–399
Lovisolo G, Distasi C, Antoniotti S, Munaron L (1997) Mitogens and calcium channels. New Physiol Sci 12:279–285
Tombaugh GC (1998) Intracellular pH buffering shapes activity-dependent Ca2+ dynamics in dendrites of CAI interneurons. J Neurophysiol 80:1702–1712
Allbritton NL, Meyer T (1993) Localized calcium spikes and propagating calcium waves. Cell Calcium 14:691–697
Berridge MJ (1995) Calcium signalling and cell proliferation. Bioassays 17:491–500
Clapham DE (1995) Calcium signaling. Cell 80:259–268
Hepler PK (1994) The role of calcium in cell division. Cell Calcium 16:322–330
Poenie M, Alderton J, Tsien RY, Steinhardt RA (1985) Changes of free calcium levels with stages of the cell division cycle. Nature 315:147–151
Tsien RW, Tsien RY (1990) Calcium channels, stores, and oscillations. Annu Rev Cell Biol 6:715–760
Johnson FE, Zhou M, Collins BT, Huang JS (2000) Mechanical deformation induces proliferation of human colorectal carcinoma cells. Int J Oncol 16:617–622
Ivarsson ML, Holmdahl L, Falk P, Mölne J, Risberg B (1998) Characterization and fibrinolytic properties of mesothelial cells isolated from peritoneal lavage. Scand J Clin Lab Invest 58(3):195–203
Bittinger F, Klein CL, Skarke C, Brochhausen C, Walgenbach S, Röhrig O, Köhler H, Kirkpatrick CJ (1996) PECAM-1 expression in human mesothelial cells: an in vitro study. Pathobiology 64(6):320–327
Kanse SM, Kost C, Wilhelm OG, Andreasen PA, Preissner KT (1996) The urokinase receptor is a major vitronectin-binding protein on endothelial cells. Exp Cell Res 224:344–353
Deng G, Royle G, Wang S, Crain K, Loskutoff DJ (1996) Structural and functional analysis of the plasminogen activator inhibitor-1 binding motif in the somatomedin B domain of vitronectin. J Biol Chem 271:12716–12723
Stefansson S, Lawrence DA (1996) The serpin PAI-1 inhibits cell migration by blocking integrin alpha V beta 3 binding to vitronectin. Nature 383:441–443
Schmitt M, Harbeck N, Thomssen C, Wilhelm O, Magdolen V, Reuning U, Ulm K, Höfler H, Janicke F, Graeff H (1997) Clinical impact of the plasminogen activation system in tumor invasion and metastasis: prognostic relevance and target for therapy. Thromb Haemost 78:285–296
Albo D, Berger DH, Vogel J, Tuszynski GP (1999) Thrombospondin-1 and transforming growth factor beta-1 upregulate plasminogen activator inhibitor type 1 in pancreatic cancer. J Gastrointest Surg 3:411–417
Grondahl-Hansen J, Christensen IJ, Rosenquist C, Brunner N, Mouridsen HT, Dano K, Blichert-Toft M (1993) High levels of urokinase-type plasminogen activator and its inhibitor PAI-1 in cytosolic extracts of breast carcinomas are associated with poor prognosis. Cancer Res 53:2513–2521
Liu G, Shuman MA, Cohen RL (1995) Co-expression of urokinase, urokinase receptor and PAI-1 is necessary for optimum invasiveness of cultured lung cancer cells. Int J Cancer 60:501–506
Sier CF, Vloedgraven HJ, Griffioen G, Ganesh S, Nagengast FM, Lamers CB, Verspaget HW (1995) Plasminogen activators and inhibitor type 1 in neoplastic colonic tissue from patients with familial adenomatous polyposis. Br J Cancer 71:393–396
Sier CF, Verspaget HW, Griffioen G, Verheijen JH, Quax PH, Dooijewaard G, De Bruin PA, Lamers CB (1991) Imbalance of plasminogen activators and their inhibitors in human colorectal neoplasia. Implications of urokinase in colorectal carcinogenesis. Gastroenterology 101:1522–1528
Acknowledgement
The authors would like to thank Andrew Entwistle for his critical review of this manuscript.
Authors’ disclosures
Dr. Petra Krause, Dr. Nina Bobisch, Dr. Paul Thelen, Dr. Karola Koehler, Dr. Sarah Koenig, Prof. Heinz Becker and Dr. Ingo Leister have no conflicts of interest or financial ties to disclose.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Krause, P., Bobisch, N.S., Thelen, P. et al. The plasminogen activator inhibitor system in colon cancer cell lines is influenced by the CO2 pneumoperitoneum. Int J Colorectal Dis 26, 37–43 (2011). https://doi.org/10.1007/s00384-010-1062-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-010-1062-y