Abstract
Background and aims
Little is known about the intestinal epithelial expression and secretion of CXCL10 (IP-10), a chemokine involved in recruiting T cells and monocytes. We aimed to study CXCL10 gene expression and regulation by the pro-inflammatory cytokines interleukin (IL)-1β, interferon (IFN)-γ and tumour necrosis factor (TNF)-α in intestinal epithelial cell lines.
Materials and methods
CXCL10 expression and secretion kinetics were assessed in Caco-2, HT-29 and DLD1 human colon epithelial cells, treated with IL-1β, TNF-α, IFN-γ alone or in combination with each other by real-time polymerase chain reaction (PCR), Northern blotting and enzyme-linked immunoabsorbent assay (ELISA). Transient transfections with TGL-IP10 (CXCL10 promoter) and TGL-IP10-κB2 mutant promoter and gelshifts and supershifts for nuclear factor (NF)-κB were also performed.
Results
Real-time PCRs and ELISA experiments revealed that IL-1β was the strongest and earliest inducer of CXCL10 messenger ribonucleic acid (mRNA) expression and protein secretion in Caco-2 cell line, whereas INF-γ had a delayed kinetics. There was a strong synergistic effect of either TNF-α or IL-1β with IFN-γ both on CXCL10 mRNA expression and protein secretion in all three cell lines. Real-time PCR and ELISA experiments using a specific NF-κB inhibitor and transfection experiments with a NF-κB-binding defective CXCL10 promoter construct revealed that the induction of CXCL10 by IL-1β and its synergism with IFN-γ is NF-κB dependent.
Conclusion
These data demonstrate that in colonic epithelial cells, depending on the cellular context and utilizing the NF-κB pathway, IL-1β alone and/or in synergism with IFN-γ may play a major role in the induction of CXCL10.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intestinal epithelial cells (IECs) form the first immunologic barrier of the organism while the villus surface is continuously in contact with various agents. IEC gene expression is tightly regulated to induce appropriate responses to pathogens and to avoid deleterious reactions to microbial flora. When stimulated with pro-inflammatory cytokines or infected with microbial pathogens, IECs may secrete chemokines, a set of low-molecular weight cytokines, directing migration and activation of leucocytes, which play a major role in the perpetuation of inflammatory processes [1–5]. The final composition of leucocytes present in the inflamed intestine is most likely due to both secreted chemokines and the relative expression of chemokine cell surface receptors on different cell types. Chemokine production by colonic epithelial cells is thought to contribute to the characteristic increased infiltration of selected populations of leucocyte cells in inflammatory bowel disease (IBD) [6, 7].
CXCL10 is a CXC chemokine, known to be secreted by endothelial cells [8], keratinocytes [9], eosinophils [10] and neutrophils [11]. It is also constitutively expressed by normal human colon epithelium [12] and chemoattracts activated T cells as well as monocytes by binding to the CXCR3 receptors present on the respective cells [13, 14]. While CXCL10 up-regulation may occur in acute inflammation in response to pathogens, it is also known to be permanently over-expressed in IBD patients [15, 16]. Blocking CXCL10 could prevent mice from acute colitis, suggesting this chemokine to play an important role in IBD pathogenesis [17]. Moreover, CXCL10 is believed to possess anti-tumoural properties by promoting anti-tumour T cell immunity [18, 19]. Knowledge of its regulation in colonic cell lines may therefore give also insight into the pathobiology of colorectal cancer.
Most previous studies on chemokine expression in IEC concentrated on CXCL8 (interleukin [IL]-8), a neutrophil chemoattractant [20, 21], but there were only few studies regarding the expression and secretion of CXCL10 in IECs [12]. Although it is well known that interferon (IFN)-γ is a major inducer of CXCL10 and that CXCL10 expression may be enhanced by pathogens and other inflammatory cytokines, the relative contribution of cytokines on CXCL10 induction, their synergistic action and the kinetics of cytokine-induced CXCL10 expression in intestinal epithelial cells has not been fully elucidated. Especially, the role of IL-1β in CXCL10 gene regulation in IECs and also in other cell types has not been fully evaluated so far. Intestinal mucosa is composed of cell populations in continuous change from a proliferative and undifferentiated stage in the basal parts of crypts to mature surface villus epithelial cells [22, 23]. Little is known about the alteration of immunological functions as IECs mature. It has been shown that cellular differentiation affects IEC responsiveness to IL-1β [24].
In the present study, we aimed to elucidate the role of the pro-inflammatory cytokines IL-1β, tumour necrosis factor (TNF)-α and IFN-γ, which have established role in IBD pathogenesis, in inducing CXCL10 gene expression in IEC lines. Especially, the role of IL-1β, one of the most abundantly expressed cytokines, both in normal and inflamed mucosa [25], in inducing CXCL10 expression by IECs and its possible signalling mechanisms was given importance. To consider possible influences of cellular differentiation on cytokine responsiveness, we performed studies on three different colonic epithelial cell lines. Our findings will get an insight into the role of intestinal epithelium in immune responses and in evaluating pathways, which might be targets of present and future pharmacotherapy of IBD and possibly colorectal cancer.
Materials and methods
Biological reagents
The recombinant cytokines IL-1β, TNF-α and IFN-γ were purchased from Roche applied science (Mannheim, Germany). An enzyme-linked immunosorbent assay (ELISA) kit for CXCL10 was purchased from RnD systems (Weisbaden, Germany). The nuclear factor (NF)-κB inhibitor BAY11-7082 was purchased from Calbiochem (San Diego, CA).
Cell culture and stimulation protocols
The human colon adenocarcinoma cell lines Caco-2, HT-29 and DLD1 were obtained from DSMZ (Braunschweig, Germany). Caco-2 cells were grown in Eagle’s minimal essential medium (BioWhittacker, Germany) containing 20% foetal calf serum (FCS) supplemented with 100 U/ml each of penicillin and streptomycin and 1% non-essential amino acids at 37°C and 5% CO2. HT29 and DLD1 were grown in Roswell Park Memorial Institute medium containing 10% FCS and 100 U/ml penicillin and streptomycin at 37°C and 5% CO2. Caco-2, HT29 and DLD-1 cells were plated into six-well plates at a density of 5 × 105 cells per well for real-time polymerase chain reactions (PCRs), ELISA, Northern blotting and electrophoresis mobility shift assay (EMSA) experiments unless until stated and grown till they reached 70–80% confluence. These cells were then stimulated with IL-1β (0.1, 0.5, 1, 2, 10 and 50 ng/ml), TNF-α (2, 10 and 50 ng/ml) and IFN-γ (2, 10 and 50 ng/ml) based on the type of experiments.
RNA isolation, real-time PCR
Ribonucleic acid (RNA) was isolated by using Qiagen RNeasy mini kit according to the manufacturer’s protocol. The RNA concentrations were determined photometrically using a Gene Quant RNA/deoxyribonucleic acid (DNA) calculator (Pharmacia, Freiburg, Germany). RNA was subsequently used for real-time PCR and Northern blot analysis. Reverse transcription of messenger RNA (mRNA) was performed using 1 μg of total cellular RNA. To determine the mRNA expression of CXCL10, real-time PCR was carried out using gene-specific primers for human CXCL10 (Invitrogen GmbH, Karlsruhe) forward 5′-CCA GAA TCG AAG GCC ATC AA-3′, reverse 5′-CAT TTC CTT GCT AAC TGC TTT CAG-3′ and β-actin (Invitrogen GmbH) forward 5′-CTG GCA CCC AGC ACA ATG-3′, reverse 5′-CCG ATC CAC ACG GAG TAC TTG-3′ in an ABI Prism 7000 sequence detection system. PCR reaction was set up with Sybr® Green PCR Master mix (Invitrogen) containing 0.3 μmol/l primers each and 1 μl of RT-product in 25 μl volume. A two-step amplification protocol was chosen consisting of initial denaturation at 95°C for 10 min followed by 45 cycles with 15 s denaturation at 95°C and 30 s annealing/extension at 60°C. Finally, a dissociation protocol was performed to control specificity of amplification products.
Relative expression of CXCL10 was then calculated using the comparative threshold-cycle (CT) method. The amount of target mRNA in each sample was normalized to the amount of β-actin mRNA designated as calibrator, to give ΔCT (CT β-actin − CT CXCL10). The relative expression of CXCL10 was calculated as the \({{{\rm{CXCL10}}} \mathord{\left/ {\vphantom {{{\rm{CXCL10}}} {{\rm{\beta - actin}}}}} \right. \kern-\nulldelimiterspace} {{\rm{\beta - actin}}}}\;{\rm{ratio}} = 2^{\Delta {\rm{CT}}} \). MRNA expression is presented as fold increase calculated in relation to unstimulated cells after normalization to β-actin.
Transient transfections
Caco-2, HT29 and DLD1 cells were plated in 24-well plates, 24 h before transfection (Costar, Corning, NY), at a density of 50,000/well in 1 ml medium. After 24 h, the cells were transfected with 250 ng of respective plasmids along with 20 ng of renilla plasmid using the non-liposomal formulation FuGENE (Roche Molecular Biochemicals, Mannheim, Germany). On the day of transfection, fresh medium was added. FuGENE was added to the plasmid DNA at a ratio of 3 μl/μg DNA. FuGENE was prediluted in 100 μl serum-free medium and added drop-wise to the concentrated plasmid DNA. After 15–25 min at room temperature, the mixture was added to the cells. The plasmids TGL-IP10, TGL-IP10 κB2 Mut were kind gifts from Dr. Richard M. Ranshoff (Cleveland, OH) and were described elsewhere [26].
Luciferase assays
Twenty-four hours after transfection, cells were stimulated with IL-1β (0.1,1, 2, 10 and 50 ng/ml), TNF-α (2, 10 and 50 ng/ml), IFN-γ (2, 10 and 50 ng/ml), IL-1β (1 ng/ml) + TNFα (50 ng/ml), IL-1β (1 ng/ml) + IFN-γ (50 ng/ml) and TNFα (50 ng/ml) + IFN-γ (50 ng/ml) for 24 h, harvested and lysed, and luciferase was assayed by using a luciferase kit (Promega). Values were normalised to renilla luciferase.
Enzyme-linked immunosorbent assay
To study the synergistic effects of cytokines on CXCL10 secretion, supernatants were collected at 0, 3, 6, 12 and 24 h in Caco-2 and HT29 cells stimulated with IL-1β (1 ng/ml), TNF-α (50 ng/ml), IFN-γ (50 ng/ml), IL-1β (0.5 ng/ml) + TNFα (50 ng/ml), IL-1β (0.5 ng/ml) + IFN-γ (50 ng/ml) and TNFα (50 ng/ml) + IFN-γ (50 ng/ml) and stored at −70°C until measured. CXCL10 protein secretion was measured by ELISA according to the manufacturer’s protocol.
Preparation of nuclear extract
Caco-2 cells were grown for 24 h, pre-treated for 1 h with BAY 11-7082 (10 μM) and then stimulated with respective cytokines for 30 min. Cells were washed with 10 ml cold phosphate-buffered saline (PBS) twice, harvested, centrifuged at 1,000 × g for 5 min and resuspended in 1 ml of cold PBS. Centrifuged briefly, excess PBS was removed, and the pellet was resuspended in ice-cold extraction buffer (20 mM hydroxyethyl piperazineethanesulfonic acid [HEPES] pH 7.8, 10 mM KCL, 0.1 mM ethylenediamine tetraacetic acid [EDTA], 1 mM dithiothreitol and 0.5 mM phenylmethanesulphonylfluoride [PMSF]) by gentle pippeting. Cells were then kept on ice for 15 min, and 30 μl of 10% Nonidet NP-40 was added and vortexed briefly for 10 s. The lysed cell suspension was centrifuged for 30 s, and the supernatant was discarded. The pellet was resuspended in 50 μl extraction buffer containing 400 mM NaCl, agitated vigorously for 15 min at 4°C. Then, the cell suspension was centrifuged for 5 min at 4°C, and the supernatant containing the nuclear extract was collected and stored at −80°C until further use.
Electrophoretic mobility shift assay and super-shift assay
For binding reactions, 5 μg of nuclear extracts were incubated in 20 μl reaction mixture containing 40 mM HEPES pH 7.5, 50 mM NaCl, 1 mM EDTA, 1mM DithitreitolHSCl, 1 mM PMSF, 1.28 μg/ml pBluescript vector DNA as half of the reaction and the rest being nuclear extract plus other components. Oligonucleotide duplex probes (Promega) were end-labelled with T4 polynucleotide kinase and [γ32P] adenosine triphosphate; 1 × 104 cpm were then added to the reaction mixtures and incubated overnight at 4°C. Reaction products were analysed by non-denaturing electrophoresis in a 5% polycralamide gel with 0.5× Tris–borate–EDTA buffer at room temperature. Gels were then exposed directly to X-ray film at −70°C for autoradiography. For competition, unlabelled oligonucleotides were added in molar excess at room temperature for 15 min before adding radiolabelled probe. In super shift experiments, nuclear extracts were incubated with anti-p65 anti-body (Santa Cruz Biotechnology, Santa Cruz, CA) overnight at 4°C.
Statistical analysis
Statistical analyses were carried out using the Prism software packet (Version 3.0, Graphpad Software, San Diego, CA). Comparisons between two or more different treatment groups were made with the non-paired t test or analysis of variance (ANOVA) where appropriate. For time kinetics experiments, a two-way ANOVA test followed by the Bonferroni post-test was performed. In case of RNA expression, a log transformation was performed before. Statistical differences were regarded significant at a p level below 0.05. Data were expressed as means ± standard error of the mean (SEM).
Results
Differential expression of CXCL10 mRNA in intestinal epithelial cell lines under basal conditions
In the present study, the basal mRNA expression of CXCL10 in three different IECs, Caco-2, HT29 and DLD1 cells, were studied first. Real-time PCR experiments using gene-specific primers for CXCL10 revealed that the basal mRNA expression of CXCL10 was highest in Caco-2 followed by HT29 and DLD1 (Fig. 1).
Basal level expression of CXCL10 in IECs. Caco-2, HT29 and DLD1 cells were plated at a density of 5 × 105 cells in six well plates, grown for 24 h and total RNA from the cells was isolated. First-strand complementary DNA was prepared from 1 μg of total RNA. Real-time PCR was performed for CXCL10 and β-actin was used as an internal control. The bars indicate the mean of six individual experiments. Asterisk corresponds to p < 0.01
IL-1β, TNF-α and IFN-γ dose-dependent influence on CXCL10 gene expression in IECs
Caco-2, HT29 and DLD1 cells were tested for their ability to respond to pro-inflammatory cytokines by the induction of CXCL10 mRNA expression. Cells were stimulated for 4 h with various concentrations of cytokines, and CXCL10 expression was analysed by real-time PCR. In response to IFN-γ and TNF-α, Caco-2, HT29 and DLD1 cells showed a dose-dependent induction of CXCL10 mRNA (Fig. 2). Increased expression of CXCL10 mRNA was observed when 2 ng/ml IL-1β was used, while a higher concentration did not further enhance expression. Further, we checked the response of IECs to lower doses of IL-1β showing a dose response in the range of 0.1 to 1 ng/ml in the induction of CXCL10 mRNA. IL-1β at a concentration of 0.5 ng/ml was able to induce maximum expression of CXCL10 mRNA at 4 h (data not shown).
Dose-dependent expression of CXCL10 mRNA in IECs stimulated with cytokines. 5 × 105 cells were plated into six-well plates and grown for 24 h and then stimulated with IL-1β, TNF-α and IFN-γ at an increasing doses of 2, 10 and 50 ng/ml. The cells were harvested after 4 h, total RNA from the cells was isolated, and first-strand cDNA was prepared from 1 μg of total RNA. Real-time PCR was performed for CXCL10, and β-actin was used as an internal control. Graph represents the mean ± SEM of four individual experiments. All cytokine-stimulated expressions were significantly different from unstimulated controls (p < 0.05). Asterisk, no significant difference between different IL-1β concentrations (p < 0.05)
IL-1β, TNF-α and IFN-γ time-dependent influence on CXCL10 gene expression in IECs
Once we confirmed the responsiveness of IECs to pro-inflammatory cytokines, we next examined the mRNA kinetics of CXCL10 induced by the cytokines alone or in combination with each other. Each cell line had a different time course of response when stimulated with respective cytokines and their combinations (Fig. 3a–c). In Caco-2, stimulated with IL-1β or TNF-α, CXCL10 mRNA was induced within the first 40 min, and the induction reached to a peak after 4 h, while IFN-γ had a later initial effect inducing CXCL10 mRNA after 2 h and reached to a maximum at 8 h. Combination of IL-1β + IFN-γ had a stronger synergistic effect in the induction of CXCL10 mRNA within 20 min and reaching to maximum after 4 h, whereas TNF-α + IFN-γ synergistically led to a later induction of CXCL10 mRNA starting at 40 min but had a strong synergistic effect after 8 h when compared to IL-1β + IFN-γ (Fig. 3a). In HT29 (Fig. 3b) and DLD1 (Fig. 3c), CXCL10 mRNA time kinetics deviated from that in Caco-2 (Fig. 3a). CXCL10 mRNA was induced after 1 h of stimulation with the respective single cytokines in DLD1. In case of HT29, either TNF-α or IFN-γ alone led to delayed induction of CXCL10 mRNA after 1 h, whereas IL-1β alone led to an induction starting at 2 h. HT29 and DLD1 cells treated with combinations of IL-1β + IFN-γ showed a strong synergistic induction of CXCL10 mRNA within 40 min, whereas the TNF-α + IFN-γ combination led to an even stronger induction of CXCL10 mRNA within 20 min in HT29 and within 40 min in DLD1. IL-1β + TNFα in combination had no synergistic effect on CXCL10 mRNA induction in all the cell lines used for this study. The real-time PCR results could be confirmed by Northern blot analysis in Caco-2 and HT29 cells. However, the detection threshold was not low enough to display basal and single cytokine-induced CXCL10 mRNA (data not shown).
Time kinetics of CXCL10 mRNA expression in IECs stimulated with cytokines. a Caco-2, b HT29 and c DLD1 cells were plated at a density of 5 × 105 cells in six-well plates and grown for 24 h and then stimulated with respective cytokines and their combinations. Cells were harvested at different time points as indicated, and total RNA from the cells was isolated and first-strand cDNA was prepared from 1 μg of total RNA. Real-time PCR was performed for CXCL10, and β-actin was used as an internal control. Graphs represent the mean ± SEM of three to five experiments. IFN-γ led to a significant increase in CXCL10 expression from 2 h onwards. A significant increase (p < 0.05) from control was observed in all expect in those marked as N.S. (non-significant). Number sign indicates time points with significant differences (p < 0.05) of cytokine combinations or IL-1β compared to IFN-γ alone
IL-1β, TNF-α and IFN-γ time-dependent influence on CXCL10 protein secretion in IECs
To test whether cytokine stimulation of IECs would lead not only to the induction of CXCL10 mRNA but also to the synthesis and secretion of the protein, Caco-2, HT29 and DLD1 cells were incubated with respective cytokines (from 3 to 24 h), and secretion of CXCL10 was detected by ELISA. Under basal conditions, Caco-2 cells secreted 0.012 ± 0.003 ng/ml CXCL10. Treatment with IL-1β, TNF-α and IFN-γ led to a time-dependent increase in CXCL10 protein, with IL-1β being the most potent stimulus during the first 6 h (Fig. 4a). Of importance, after 12 h, CXCL10 secretion was stimulated strongly by IFN-γ. Co-incubation of Caco-2 with respective cytokines revealed a synergistic effect of IL-1β + IFN-γ and TNF-α + IFN-γ on CXCL10 secretion, reaching levels of 3.354 ± 0.690 and 7.808.1 ± 0.173 ng/ml after 24 h. The combination of IL-1β + TNF-α had no synergistic effect on CXCL10 secretion when compared to the respective cytokines alone. These time kinetic studies revealed that in Caco-2, IL-1β alone or in combination with IFN-γ induced the secretion of CXCL10 very early compared to the combination of TNF-α + IFN-γ, which induced a delayed but stronger synergistic secretion of CXCL10 protein, suggesting that in case of IL-1β + IFN-γ, a synergism could take place very early, e.g., at the level of intracellular signal cascades. In HT29 cultures, CXCL10 secretion was not detectable under basal condition. TNF-α or IFN-γ alone led to an induction of CXCL10 protein secretion within 3 h (0.0172 ± 0.005 and 0.011 ± 0.001 ng/ml), whereas IL-1β could not induce the secretion of CXCL10 protein. IL-1β, TNF-α and IFN-γ led to a time-dependent increase in CXCL10 concentrations in HT29 cell supernatants reaching maximum levels of 0.039 ± 0.0057, 0.632 ± 0.0222 and 19.929 ± 0.838 ng/ml showing that IFN-γ is the strongest inducer of CXCL10 protein secretion when compared to other two cytokines in this cell line (Fig. 4b). The combinations of TNFα + IFN-γ and IL-1β + IFN-γ induced CXCL10 protein secretion to 1.822 ± 0.109 and 0.410 ± 0.027 ng/ml within 3 h and led to a maximum of 492.728 ± 83.776 and 87.158 ± 7.913 ng/ml after 24 h (Fig. 4b).
Time kinetics of CXCL10 protein secretion in Caco-2 and HT29 cells stimulated with cytokines. 5 × 105 cells were plated into six-well plates and grown for 24 h and then stimulated with IL-1β, TNF-α and IFN-γ as indicated. Supernatants were collected at respective time points from a Caco-2 and b HT29 cells and ELISA for CXCL10 protein was performed. Data represent means of three to five experiments ± SEM done in duplicates for each sample. Asterisk indicates time points with significant differences (p < 0.05) of cytokine combinations compared to IFN-γ alone
CXCL10 promoter activation by cytokines
TGL-IP10, a promoter-reporter containing 435 bp of human CXCL10 sequence upstream of the transcriptional start site, was used to evaluate the role of IL-1β, TNF-α and IFN-γ alone or in combination with each other in the transcription of CXCL10. When TGL-IP10-transfected Caco-2 cells were stimulated with single cytokines, IL-1β (1 ng/ml) led to a stronger induction (6.53 ± 1.65-fold increase) than TNF-α (50 ng/ml) and IFN-γ (50 ng/ml) alone (2.76 ± 0.53 and 3.14 ± 1.2-fold increase). The combination of IL-1β + IFN-γ showed a stronger synergistic induction (26.18 ± 11.68) than the combination of TNF-α + IFN-γ (13.97 ± 3.25-fold increase) (Fig. 5a). In HT29 cells, when stimulated with single cytokines, IFN-γ (50 ng/ml) led to a maximum induction (6.52 ± 0.58-fold increase), followed by TNF-α (4.44 ± 0.16-fold increase) and IL-1β (1.43 ± 0.05-fold increase). The combination of IL-1β + IFN-γ synergistically led to 12.76 ± 3.21-fold induction, and TNF-α + IFN-γ led to 26.70 ± 7.5-fold induction of promoter activity (Fig. 5b). In DLD1 cells (Fig. 5c), IFN-γ (50 ng/ml) led to a maximum induction (8.06 ± 0.51-fold increase) of CXCL10 promoter activity followed by TNF-α (50 ng/ml) induction (3.59 ± 0.08-fold increase) and IL-1β (1 ng/ml) induction (2.32 ± 0.12-fold increase). The combination of IL-1β + IFN-γ led to a 40.72 ± 12.19-fold induction, and TNF-α + IFN-γ led to a 20.56 ± 6.27 fold induction. In all three cell lines, the combination of IL-1β + TNF-α had no synergistic effect on CXCL10 promoter activity.
Transient transfection analysis of TGL-IP10 in IECs. The CXCL10 promoter containing reporter construct, pTGL-IP10 and pRL-TK (renilla) plasmids, was transiently transfected into a Caco-2, b HT29 and c DLD1 cells. 24 h after transfection, cells were stimulated with cytokines as indicated for 24 h, harvested, and promoter activity was monitored by luciferase assay. Data were normalised with renilla luciferase values and included as fold increase vs control. Data represent the means ± SEM of three to five independent experiments done in duplicates for each sample. Asterisk indicates an induction significantly different (p < 0.05) from control (C). Significant differences between combinations of cytokines and the respective single cytokines are indicated with bars with a number sign (p < 0.05). N.S. is not significant
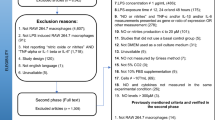
Evaluating the role of NF-κB in CXCL10 gene expression
To evaluate the possible role of NF-κB in cytokine-induced CXCL10 gene expression, experiments with a specific NF-κB inhibitor were performed. The effect of BAY 11-7082 on NF-κB inhibition was evaluated by reporter assays. BAY11-7082 was able to dose-dependently inhibit IL-1β-induced pNF-κB-SEAP gene reporter activity in Caco-2 cells (data not shown). Based on this experiment, we could determine that 10 μM of BAY11-7082 was sufficient to inhibit the NF-κB activation.
The induction of CXCL10 gene expression by cytokines was inhibited by addition of the NF-κB-specific inhibitor BAY11-7082 in Caco-2, HT29 and DLD1 cells, with a varying degree of inhibition in the individual cell lines. Inhibition of NF-κB led to almost complete inhibition (approximately 90–95% inhibition) of CXCL10 mRNA and protein secretion induced by cytokines in Caco-2 and DLD1 cells (Fig. 6a and c). In DLD1 cells, IL-1β (1 ng/ml) did not have any inducing effect on CXCL10 secretion. In HT29, inhibition of NF-κB had approximately 60–75% inhibitory effect on cytokine-induced CXCL10 mRNA expression and secretion (Fig. 6b).
Role of NF-κB in cytokine-induced CXCL10 mRNA expression by IECs. 5 × 105 cells were plated and grown for 24 h. Then, the cells were pre-treated with 10 μM of BAY 11-7082 for 1 h and then stimulated with respective cytokines and their combinations as stated in the figure for 2 and 24 h. After 2 h, cells were harvested for RNA isolation to perform real-time PCRs, and at 24 h, cell supernatants were collected and stored at −70°C until ELISA was performed for CXCL10. Data presented are the means ± SEM of three independent experiments done in duplicates for each sample in a Caco-2, b HT29 and c DLD1 cells. Significant CXCL10 inhibition by BAY 11-7082 is indicated by an asterisk (p < 0.05). N.S. is not significant
To further evaluate the role of NF-κB, transient transfections were done with a CXCL10 promoter construct bearing a mutated NFkB-binding site (TGL-IP10 κB2 Mut). In Caco-2 cells, TGL-IP10 κB2 Mut was not responsive to any of the cytokines and their combinations, suggesting that CXCL10 gene induction is strongly dependent on NF-κB in this cell line (Fig. 7a). In HT29 and DLD1 cells, the combination of TNF-α + IFN-γ led to 6.49 ± 2.13 and 4.87 ± 1.43-fold increase, and the combination of IL-1β + IFN-γ led to 2.26 ± 0.63 and 4.75 ± 0.53-fold increase of the TGL-IP10 κB2 Mut promoter activity (Fig. 7b and c), revealing that a smaller portion of CXCL10 gene expression might be regulated independently from NF-κB.
Transient transfection analysis of TGL-IP10 and TGL-IP10 κB2 mutant in IECs. TGL-IP-10 and TGL-IP10-κB2 Mut plasmid was transiently transfected into a Caco-2, b HT29 and c DLD1. 24 h after transfection, cells were stimulated with cytokines for 24 h, and promoter activity was monitored by luciferase assay. Data were normalised with renilla luciferase values. Data presented are the means ± SEM of three to five independent experiments done in duplicates for each sample. Significant differences vs controls (C) are indicated by an asterisk (p < 0.05). Significant differences of wild type vs mutant are indicated by a number sign (p < 0.05). N.S. is not significant
To confirm further our results from promoter and inhibitor studies, we did gel-shift and super shift assays to show that NF-κB is activated by cytokines and that the activated NF-κB complex contains the NF-κB functional sub-unit p65. In the nuclear extracts of Caco-2 cells, we could clearly see a shift in the samples treated with IL-1β, TNF-α alone or the combinations of IL-1β + IFN-γ and TNF-α + IFN-γ. The protein-DNA complex was efficiently competed by unlabelled κB oligonucleotides. There was no shift in the samples treated with the NF-κB inhibitor BAY11-7082, stating that the shift was indeed because of NF-κB binding. Furthermore, antibody super shift assay using anti-p65 antibody had clearly shown that the complex contains NF-κB functional sub-unit, p65 (Fig. 8).
Gel shift and super shift analysis for NF-κB. Caco-2 cells were seeded and grown for 24 h before pre-treating with BAY 11-7082 (10 μM) for 1 h and then stimulated with respective cytokines for 30 min; cells were then harvested, and nuclear extracts were prepared. 5 μg of nuclear extracts were used for gel shifts with a wild-type κB oligonucleotide. Super shifts were performed with anti-p65 antibody. Similar results were obtained in two separate experiments
Discussion
In addition to its many homeostatic functions such as barrier protection, mucus production and resorption, the intestinal epithelium plays an important role in regulating local inflammation and immune responses. The intestinal epithelium participates in inflammatory responses in part through the generation of numerous cytokines and chemokines that mediate recruitment and activation of inflammatory cells. The epithelium is involved in local cytokine networks allowing first response to noxious agents as well as cross-talk with immune cells to help provide an effective inflammatory response. These bi-directional inflammatory communications are necessary for normal host defence, but they also play an important role in the pathogenesis of IBD and might be also of importance in modulating anti-tumoural immunity in colonic malignancies. In this report, we demonstrate that pro-inflammatory cytokines, which may be produced by sub-mucosal immune cells, can differentially and co-ordinately regulate CXCL10 gene expression in IECs.
CXCL10 is one of several chemokines produced by IEC. Previous studies could show that IFN-γ in combination with TNF-α caused induction of RANTES (regulated upon activation, normal t-cell expressed, and secreted protein) and monocyte chemotactic protein-1 in colorectal tumour cell lines, while IFN-γ had no effect on CXCL8 (IL-8) secretion [27], the latter observation being confirmed in all three cell lines in the present study (data not shown).
Dwinell et al. [12] had previously shown that stimulation of IECs with TNF-α or IL-1α strongly potentiated IFN-γ-induced CXCL10. It is well known that among IL-1α and IL-1β, the latter is secreted and has an active role in inflammation. Importantly, IL-1β was shown to be over-expressed in IBD patients [25, 28]. This makes IL-1β an interesting cytokine to study its effect on CXCL10 gene regulation. Although the synergistic effects of TNF-α + IFN-γ on CXCL10 gene expression and the signalling mechanisms involved were studied in astrocytes [26] and their synergistic effect on inducible nitric oxide synthase expression in IECs and macrophages [29] had been studied in detail, the synergistic action of these cytokines on CXCL10 gene expression and the signalling mechanisms involved have not been evaluated in IECs. Especially, the role of IL-1β alone and its synergism with both TNF-α and IFN-γ on CXCL10 gene expression in IECs has been given no attention.
Previously, it has been shown that IECs may express elevated levels of CXCL10 [12], and its expression is increased in the mucosa of patients with IBD [16]. A critical role for CXCL10 in IBD has also been shown in animal models [30, 31]. Apart from this, CXCL10 has been shown to be expressed constitutively in colorectal carcinomas and primary metastatic sites exerting anti-tumour activity by recruiting mononuclear cells via the CXCR3 receptor. However, at the same time, it has also been shown that CXCL10 promoted metastatic adhesion and tumour cell migration [32] so that care should be taken considering CXCL10 as an anti-tumoural therapy option.
In light of these findings, we assessed whether stimulation of IECs in culture by inflammatory mediators could induce CXCL10 gene expression. All three IEC lines we used expressed CXCL10 mRNA in a concentration-dependent manner when stimulated with IFN-γ and TNF-α alone. These data support a vast body of evidence that demonstrates that IFN-γ can induce CXCL10 expression in a variety of cells types, including granulocytes, T lymphocytes, bronchial epithelial cells and keratinocytes [33, 34], while TNF-α is a potent inducer for CXCL10 in hepatocytes [17]. Importantly, in addition to these data, we could also show that Caco-2 cells stimulated with IL-1β up-regulate CXCL10 mRNA to a significant level, whereas in HT29 and DLD1 cells, induction of CXCL10 mRNA was less pronounced.
A number of authors have reported functional synergy between TNF-α and IFN-γ in promoting gene expression for proteins such as RANTES, IFN regulatory factor 1 (IRF-1), MIG and intercellular adhesion molecule-1[35–38] in a variety of cell types and have demonstrated that this synergy depends on the co-existence of TNF-α-responsive NF-κB-binding sites and IFN-γ-responsive signal transducers and activators of transcription (STAT) protein-binding elements within the promoters of the genes of interest [35, 36]. In our study, when IFN-γ and TNF-α were combined, the accumulation of CXCL10 mRNA and protein was elevated compared to unstimulated cells or cells stimulated with either cytokine alone, implying a synergistic effect on transcription of the CXCL10 gene. A synergistic effect by these two cytokines on CXCL10 expression was also demonstrated in astrocytes, and this synergy has been shown to be at least in part dependent on NF-κB activation and binding to a NF-κB-binding site within the CXCL10 promoter [26].
The synergistic action of IL-1β with IFN-γ in IECs has not been characterised so far. Recently, Takami et al. [39] showed the synergistic induction of hepatocyte growth factor in human skin fibroblasts by IL-1β + IFN-γ+ IFN-γ [39]. We here report for the first time that in intestinal epithelial cell lines, IL-1β alone or in combination with IFN-γ induced CXCL10 gene expression. In Caco-2 cells, the combination led to an early synergistic induction of both CXCL10 mRNA and protein compared to the combination of IFN-γ+TNF-α. This early induction of CXCL10 mRNA and protein by IL-1β+IFN-γ in Caco-2 might be due to the early convergence of signalling pathways that activates transcription factors like NF-κB, IRF-1, STAT1 or other factors that mediate transcription factor interactions.
Transient transfections with human CXCL10 promoter [26], in Caco-2, HT29 and DLD1 cells, showed that the synergistic effect of IL-1β + IFN-γ and IFN-γ + TNF-α on CXCL10 gene expression in these cell lines was indeed because of the transcriptional synergy employed at the level of the CXCL10 promoter. A number of studies had revealed that cytokines like IL-1β, TNF-α or enteroinvasive bacteria and the bacterial cell wall product lipopolysaccharide induce the expression of several inflammatory genes through the transcription factor NF-κB in IECs [40–43]. To find out the signalling mechanism involved in CXCL10 gene expression in IECs, we explored the role of transcription factor NF-κB. Inhibition of NF-κB with BAY11-7082 clearly inhibited both CXCL10 mRNA and protein induced by single cytokine alone or in combinations in Caco-2, HT29 and DLD1 cells. Gel shift in Caco-2 could confirm that NF-κB is activated and binds to consensus κB oligonucleotides in cells treated with either IL-1β or TNF-α alone and in combination with IFN-γ. It was shown previously that the binding complex of NF-κB to the κB2-binding site of the CXCL10 promoter contains the homodimer of p65 [26]. In our study, super shift assays in Caco-2 cells treated with IL-1β alone or in combination with IFN-γ confirmed the presence of p65 in the complexes bound to the consensus κB oligo nucleotides. In addition to these experiments, transient transfection experiments with a κB2 mutant of the CXCL10 promoter [26] clearly showed that in Caco-2 cells, none of the cytokines and their combinations were able to induce the CXCL10 promoter activity. In HT29 cells, the combination of IFN-γ + TNF-α led to a weaker induction of TGL-IP10κB-2 mutant activity, whereas in DLD1cells, the combination of IL-1β + IFN-γ and IFN-γ + TNF-α led to a weak induction of TGL-IP10 κB-2 mutant activity. Based on these data, we can conclude that NF-κB plays a critical role in CXCL10 gene expression induced by cytokines in IECs, and this is mainly dependent on the κB-2 site present in its promoter. Moreover, IFN-γ-induced CXCL10 mRNA and protein secretion was inhibited upon NF-kB inhibition.
Although the present results may reflect only a small aspect in the overall concert of chemokines, it seems apparent that the basic regulatory principles elucidated here might be shared also by a number of other chemokine genes like that of CCL19, which has recently been shown to be regulated by multiple NF-κB and IRF family transcription factors in human monocyte-derived dendritic cells [44]. Recently, Hiroi M et.al. [45] showed that co-operation between IFN-γ induced STAT1, and the constitutively active or inducible NF-κB is necessary for the transcriptional activity of IFN-γ-inducible genes like MIG and CXCL10. Therefore, we suggest a similar mechanism for IFN-γ-induced CXCL10 in IECs.
The responsiveness to cytokines might depend on the state of differentiation. Schlottmann et. al. [46] recently showed that in contrast to HT29 where IFNγ up-regulated CXCL8 secretion, the same was unaffected in Caco-2 cells or even down-regulated in primary colonic epithelial cells. Future studies on chemokine regulation should therefore include primary cells, keeping well in mind that the presence of contaminating immune cells, culture conditions and cell stress during isolation may influence results.
Taken together, our data suggest that while IFN-γ, TNF-α and IL-1β may work individually through disparate signalling pathways in CXCL10 gene regulation, a combination of these cytokines enhances transcription of the CXCL10 gene in an NF-κB-dependent manner. The fact that IL-1β via activation of NF-κB is able to mimic the effect of TNF-α in augmenting CXCL10 expression might be of importance in patients with IBD, who do not respond to anti TNF-α antibody therapy. In those cases, an additional inhibition of IL-1β might be desirable as a future therapy option in treating IBD.
References
Baggiolini M, Dewald B, Moser B (1994) Interleukin-8 and related chemotactic cytokines—CXC and CC chemokines. Adv Immunol 55:97–179
Baggiolini M, Dewald B, Moser B (1997) Human chemokines: an update. Annu Rev Immunol 15:675–705
Taub DD (1996) Chemokine–leukocyte interactions. The voodoo that they do so well. Cytokine Growth Factor Rev 7:355–376
Taub DD, Oppenheim JJ (1994) Chemokines, inflammation and the immune system. Ther Immunol 1:229–246
Adams DH, Lloyd AR (1997) Chemokines: leucocyte recruitment and activation cytokines. Lancet 349:490–495
Sierro F, Dubois B, Coste A, Kaiserlian D, Kraehenbuhl JP, Sirard JC (2001) Flagellin stimulation of intestinal epithelial cells triggers CCL20-mediated migration of dendritic cells. Proc Natl Acad Sci USA 98:13722–13727
Brand S, Sakaguchi T, Gu X, Colgan SP, Reinecker HC (2002) Fractalkine-mediated signals regulate cell-survival and immune-modulatory responses in intestinal epithelial cells. Gastroenterology 122:166–177
Marx N, Mach F, Sauty A, Leung JH, Sarafi MN, Ransohoff RM, Libby P, Plutzky J, Luster AD (2000) Peroxisome proliferator-activated receptor-gamma activators inhibit IFN-gamma-induced expression of the T cell-active CXC chemokines IP-10, Mig, and I-TAC in human endothelial cells. J Immunol 164:6503–6508
Boorsma DM, Flier J, Sampat S, Ottevanger C, de Haan P, Hooft L, Willemze R, Tensen CP, Stoof TJ (1998) Chemokine IP-10 expression in cultured human keratinocytes. Arch Dermatol Res 290:335–341
Dajotoy T, Andersson P, Bjartell A, Lofdahl CG, Tapper H, Egesten A (2004) Human eosinophils produce the T cell-attracting chemokines MIG and IP-10 upon stimulation with IFN-gamma. J Leukoc Biol 76:685–691
Gasperini S, Marchi M, Calzetti F, Laudanna C, Vicentini L, Olsen H, Murphy M, Liao F, Farber J, Cassatella MA (1999) Gene expression and production of the monokine induced by IFN-gamma (MIG), IFN-inducible T cell alpha chemoattractant (I-TAC), and IFN-gamma-inducible protein-10 (IP-10) chemokines by human neutrophils. J Immunol 162:4928–4937
Dwinell MB, Lugering N, Eckmann L, Kagnoff MF (2001) Regulated production of interferon-inducible T-cell chemoattractants by human intestinal epithelial cells. Gastroenterology 120:49–59
Luster AD, Ravetch JV (1987) Biochemical characterization of a gamma interferon-inducible cytokine (IP-10). J Exp Med 166:1084–1097
Farber JM (1997) Mig and IP-10: CXC chemokines that target lymphocytes. J Leukoc Biol 61:246–257
Banks C, Bateman A, Payne R, Johnson P, Sheron N (2003) Chemokine expression in IBD. Mucosal chemokine expression is unselectively increased in both ulcerative colitis and Crohn’s disease. J Pathol 199:28–35
Uguccioni M, Gionchetti P, Robbiani DF, Rizzello F, Peruzzo S, Campieri M, Baggiolini M (1999) Increased expression of IP-10, IL-8, MCP-1, and MCP-3 in ulcerative colitis. Am J Pathol 155:331–336
Sasaki S, Yoneyama H, Suzuki K, Suriki H, Aiba T, Watanabe S, Kawauchi Y, Kawachi H, Shimizu F, Matsushima K, Asakura H, Narumi S (2002) Blockade of CXCL10 protects mice from acute colitis and enhances crypt cell survival. Eur J Immunol 32:3197–3205
Yang X, Chu Y, Wang Y, Zhang R, Xiong S (2006) Targeted in vivo expression of IFN-g-inducible protein 10 induces specific antitumor activity. J Leukoc Biol 80:1434–1444
Narvaiza I, Mazzolini G, Barajas M, Duarte M, Zaratiegui M, Qian C, Melero I, Prieto J (2000) Intramural coinjection of two adenoviruses, one encoding the chemokine IFN-g-inducible protein-10 and another encoding IL-12, results in marked antitumoral synergy. J Immunol 164:3112–3122
Yang SK, Eckmann L, Panja A, Kagnoff MF (1997) Differential and regulated expression of C-X-C, C-C, and C-chemokines by human colon epithelial cells. Gastroenterology 113:1214–1223
Jung HC, Eckmann L, Yang SK, Panja A, Fierer J, Morzycka-Wroblewska E, Kagnoff MF (1995) A distinct array of proinflammatory cytokines is expressed in human colon epithelial cells in response to bacterial invasion. J Clin Invest 95:55–65
Wong MH, Stappenbeck TS, Gordon JI (1999) Living and commuting in intestinal crypts. Gastroenterology 116:208–210
Que FG, Gores GJ (1996) Cell death by apoptosis: basic concepts and disease relevance for the gastroenterologist. Gastroenterology 110:1238–1243
Bocker U, Schottelius A, Watson JM, Holt L, Licato LL, Brenner DA, Sartor RB, Jobin C (2000) Cellular differentiation causes a selective down-regulation of interleukin (IL)-1beta-mediated NF-kappaB activation and IL-8 gene expression in intestinal epithelial cells. J Biol Chem 275:12207–12213
Raddatz D, Bockemuhl M, Ramadori G (2005) Quantitative measurement of cytokine mRNA in inflammatory bowel disease: relation to clinical and endoscopic activity and outcome. Eur J Gastroenterol Hepatol 17:547–557
Majumder S, Zhou LZ, Chaturvedi P, Babcock G, Aras S, Ranshoff RM (1998) p48/STAT-1a -containing complexes play a predominant role in induction of IFN-g-inducible protein, 10 kDa (IP-10) by IFN-g alone or in synergy with TNF-a. J Immunol 161:4736–4744
Warhurst AC, Hopkins SJ, Warhurst G (1998) Interferon gamma induces differential upregulation of alpha and beta chemokine secretion in colonic epithelial cell lines. Gut 42:208–213
Rogler G, Andus T (1998) Cytokines in inflammatory bowel disease. World J Surg 22:382–389
Saura M, Zaragoza C, Bao C, McMillan A, Lowenstein CJ (1999) Interaction of Interferon Regulatory Factor -1 and Nuclear Factor kB during activation of inducible nitric oxide synthase transcription. J Mol Biol 289:459–471
Ito R, Shin-ya M, Kishida T, Urano A, Takada R, Sakagami J, Imanishi J, Kita M, Ueda Y, Iwakura Y, Kataoka K, Okanoue T, Mazda O (2006) Interferon-gamma is causatively involved in experimental inflammatory bowel disease in mice. Clin Exp Immunol 146:330–338
Hyun JG, Lee G, Brown JB, Grimm GR, Tang Y, Mittal N, Dirisina R, Zhang Z, Fryer JP, Weinstock JV, Luster AD, Barrett T (2005) Anti-interferon-inducible chemokine, CXCL10, Reduces colitis by impairing T Helper-1 induction and recruitment in mice. Inflamm Bowel Dis 11:799–805
Zipin-Roitman A, Meshel T, Sagi-Assif O, Shalmon B, Avivi C, Pfeffer RM, Witz IP, Ben-Baruch A (2007) CXCL10 promotes invasion-related properties in human colorectal carcinoma cells. Cancer Res 67:3396–3405
Kanda N, Watanabe S (2002) Substance P enhances the production of interferon-induced protein of 10 kDa by human keratinocytes in synergy with interferon-gamma. J Invest Dermatol 119:1290–1297
Hardaker EL, Bacon AM, Carlson K, Roshak AK, Foley JJ, Schmidt DB, Buckley PT, Comegys M, Panettieri RA Jr., Sarau HM, Belmonte KE (2004) Regulation of TNF-alpha- and IFN-gamma-induced CXCL10 expression: participation of the airway smooth muscle in the pulmonary inflammatory response in chronic obstructive pulmonary disease. Faseb J 18:191–193
Ohmori Y, Schreiber RD, Hamilton TA (1997) Synergy between Interferon-g and tumor necrosis factor-a in transcriptional activation is mediated by cooperation between signal transducer and activator of transcription 1 and nuclear factor kB. J Biol Chem 272:14899–14907
Lee A, Hong J, Seo Y (2000) Tumour necrosis factor-alpha and Interferon gamma synergistically activates the RANTES promoter through nuclear factor kappa B and interferon regulatory factor-1(IRF-1) transcription factors. Biochem J 350:131–138
Pine R (1997) Convergence of TNFa and IFNg signalling pathways through synergistic induction of IRF-1/ISGF-2 is mediated by a composite GAS/kB element. Nucleic acid res 25:4346–4354
Czech W, Krutmann J, Budnik A, Schopf E, Kapp A (1993) Induction of intercellular adhesion molecule 1 (ICAM-1) expression in normal human eosinophils by inflammatory cytokines. J Invest Dermatol 100:417–423
Takami Y, Motoki T, Yamamoto I, Gohda E (2005) Synergistic induction of hepatocyte growth factor in human skin fibroblasts by the inflammatory cytokines interleukin-1 and interferon-[gamma]. Molec Cell Biol Res Commun 327:212–217
Elewaut D, DiDonato JA, Kim JM, Truong F, Eckmann L, Kagnoff MF (1999) NF-kappa B is a central regulator of the intestinal epithelial cell innate immune response induced by infection with enteroinvasive bacteria. J Immunol 163:1457–1466
Kim JM, Cho SJ, Oh YK, Jung HY, Kim YJ, Kim N (2002) Nuclear factor-kappa B activation pathway in intestinal epithelial cells is a major regulator of chemokine gene expression and neutrophil migration induced by Bacteroides fragilis enterotoxin. Clin Exp Immunol 130:59–66
Kim JA, Kim DK, Jin T, Kang OH, Choi YA, Choi SC, Kim TH, Nah YH, Choi SJ, Kim YH, Bae KH, Lee YM (2004) Acanthoic acid inhibits IL-8 production via MAPKs and NF-kappaB in a TNF-alpha-stimulated human intestinal epithelial cell line. Clin Chim Acta 342:193–202
Vallee S, Laforest S, Fouchier F, Montero MP, Penel C, Champion S (2004) Cytokine-induced upregulation of NF-kappaB, IL-8, and ICAM-1 is dependent on colonic cell polarity: implication for PKCdelta. Exp Cell Res 297:165–185
Pietila TE, Veckman V, Lehtonen A, Lin R, Hiscott J, Julkunen I (2007) Multiple NF-kB and IFN regulatory factor family transcription factors regulate CCL19 gene expression in human monocyte-derived dendritic cells. J Immunol 178:253–261
Hiroi M, Ohmori Y (2003) Constitutive nuclear factor kappaB activity is required to elicit interferon-gamma-induced expression of chemokine CXC ligand 9 (CXCL9) and CXCL10 in human tumour cell lines. Biochem J 376:393–402
Schlottmann K, Wachs FP, Grossmann J, Vogl D, Maendel M, Falk W, Scholmerich J, Andus T, Rogler G (2004) Interferon gamma downregulates IL-8 production in primary human colonic epithelial cells without induction of apoptosis. Int J Colorectal Dis 19:421–429
Acknowledgments
We would like to thank Dr. Richard M. Ranshoff (Cleveland, OH) for the kind gift of TGL-IP10 and TGL-IP10 κB2 mutant plasmids. This work was supported by the Deutsche Forschungsgemeinschaft Graduiertenkolleg 335.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Yeruva, S., Ramadori, G. & Raddatz, D. NF-κB-dependent synergistic regulation of CXCL10 gene expression by IL-1β and IFN-γ in human intestinal epithelial cell lines. Int J Colorectal Dis 23, 305–317 (2008). https://doi.org/10.1007/s00384-007-0396-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-007-0396-6