Abstract
Background & aims
Pilot studies have indicated a therapeutic role for an apheresis device (Adacolumn) that selectively adsorbs leukocytes in patients with inflammatory bowel diseases. It may also exert immunoregulatory effects contributing to its clinical efficacy. This study aimed to correlate the clinical response to leukocyte apheresis with the expression of key cytokines in mucosal tissue, in peripheral leukocytes, and in plasma.
Methods
Ten patients (seven with Crohn’s disease and three with ulcerative colitis, median age: 31 years) with mild to moderately chronic activity were recruited to an open study. Patients were refractory to or had a relapse despite conventional treatment including azathioprine. Leukocyte apheresis was performed once a week for five consecutive weeks. Clinical efficacy was assessed on week 7 and after 12 months. Colonoscopy with multiple biopsies was performed at the start of the study and after 7 weeks for semiquantitative immunohistochemical analyses of cytokines. Cytokine levels in blood and the proportion of cytokine producing CD4+ and CD8+ lymphocytes were determined.
Results
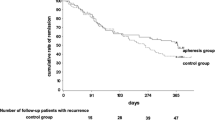
The apheresis procedures were well tolerated and no major adverse events were encountered. The median clinical activity score decreased from 12 to 7 on week 7 (P=0.031, n=9) and to 4 after 12 months (P=0.004, n=9). Five patients were in clinical remission at the 12th month. Tissue interferon (IFN)-γ-positive T-cells decreased in clinical responders (P=0.027) after apheresis. In parallel, significantly lower levels of IFN-γ-producing lymphocytes were detected in peripheral blood. IFN-γ-positive cells in pretreatment biopsies completely disappeared or decreased in posttreatment biopsies sampled on week 7 in responders (P=0.027) and appeared to predict the maintenance of long-term remission or response after 12 months.
Conclusions
Leukocyte apheresis is a novel and safe nonpharmacological adjunct therapy that may prove useful in steroid refractory or dependent patients when conventional drugs have failed. Down-regulation of IFN-γ in mucosal biopsies and in peripheral leukocytes may be a predictive marker for sustained, long-term response.



Similar content being viewed by others
References
Podolsky DK (2002) Inflammatory bowel diseases. N Engl J Med 347:417–429
Sandler RS, Loftus EV (2004) Epidemiology of inflammatory bowel diseases. In: Sartor RB, Sandborn WJ (eds) Kirsners’ Inflammatory bowel diseases. Saunders, Edinburgh, pp 245–262
Ahmad T, Pesi C, Jewell D, Colombel JF (2004) Clinical relevance of advances in genetics and pharmacogenetics of IBD. Gastroenterol 126:1533–1549
Sartor RB (2004) Therapeutic manipulation of the enteric microflora in inflammatory bowel diseases: antibiotics, probiotics and prebiotics. Gastroenterol 126:1620–1633
Rachmilewitz D (1989) Coated mesalazine (5-aminosalicylic acid) versus sulphasalazine in the treatment of active ulcerative colitis. Br Med J 298:82–86 (on behalf of an international study group)
Hanauer SB (2004) Medical therapy of ulcerative colitis 2004. Gastroenterol 126:1582–1592
Egan LJ, Sandborn WJ (2004) Advances in the treatment of Crohn’s disease. Gastroenterol 126:1574–1581
Panaccione R, Fedorak RN (2003) Primer of current therapies in inflammatory bowel disease. In: Satsangi J et al (eds) Inflammatory bowel disease. Churchill Livingstone, London, pp 320–331
van Dullemen HM, van Deventer SJ, Hommes DW, Bijil HA, Woody J (1995) Treatment of Crohn’s disease with anti-tumour necrosis factor chimeric monoclonal antibody (cA2). Gastroenterol 109:129–135
Lichtiger S, Present DH, Kornbluth A et al (1994) Cyclosporine A I severe ulcerative colitis refractory to steroid treatment. N Engl J Med 330:1841–1845
Loftus E, Sandborn W (2004) Balancing the risks and benefit of infliximab treatment of IBD. Gut 53:780–782
Siveke JT, Folwaczny (2004) Medical approaches and future options in chronic active ulcerative colitis. Int J Colorectal Dis 19:297–307
Rutgeerts PR, Asssche GV, Vermeire S (2004) Optimizing anti-TNF treatment in IBD. Gastroenterol 126:1593–1610
Cassatella MA (1995) The production of cytokines by polymorphonuclear neutrophils. Immunol Today 16:21–26
Nikolaus S, Bauditz J, Gionchetti P (1998) Increased secretion of pro-inflammatory cytokines by circulating polymorphonuclear neutrophils and regulation by interleukin-10 during intestinal inflammation. Gut 42:470–476
Saniabadi AR, Hanai H, Takeuchi K, Bjarnason I, Lofberg R (2003) Adacolumn, an adsorptive carrier based granulocyte and monocyte apheresis device for the treatment of inflammatory and refractory diseases associated with leukocytes. Ther Apher Dial 7:48–59
D’Arrigo C, Candal-Couto JJ, Greer M, Veale DJ, Woof JM (1994) Human neutrophil Fc receptor mediated adhesion under flow: a hallow fiber model of intravascular arrest. Clin Exp Immunol 100:173–179
Hiraishi K, Takeda Y, Shiobara N, Shibusawa H, Jimma F, Kashiwagi N, Saniabadi AR, Adachi M (2003) Studies on the mechanisms of leukocyte adhesion to cellulose acetate beads: an in vitro model to assess the efficacy of cellulose acetate carrier-based granulocyte and monocyte adsorptive apheresis. Ther Apher Dial 7:334–340
Ohara M, Saniabadi AR, Hirata I, Kasukawa R (1997) Granulocytapheresis in the treatment of patients with rheumatoid arthritis. Artif Organs 21:989–994
Kashiwagi N, Hirata I, Kasukawa R (1998) A role for granulocyte and monocyte apheresis in the treatment of rheumatoid arthritis. Ther Apher 2:134–141
Shimoyama T, Sawada K, Hiwatashi N, Sawada T, Saniabadi AR (2001) Safety and efficacy of granulocyte and monocyte adsorption apheresis in patients with active ulcerative colitis: a multicenter study. J Clin Apheresis 16:1–9
Hanai H, Watanabe F, Saniabadi A, Matsushita I, Takeuchi K, Iida T (2002) Therapeutic efficacy of granulocyte and monocyte adsorption apheresis in severe active ulcerative colitis. Dig Dis Sci 47:2349–2353
Matsui T, Nishimura T, Matake H, Ohta T, Sakurai T, Yao T (2003) Granulocytapheresis for Crohn’s Disease: a report on seven refractory patients. Am J Gastroenterol 511–512
Törkvist L, Thorlacius H, Sjöqvist U et al (1999) Low molecular weight heparin as adjuvant therapy in active ulcerative colitis. Aliment Pharmacol Ther 13(10):1323–1328 (Oct)
Danielsson Å, Löfberg R, Salde L, Schiöler R, Suhr O, Willén R (1992) A steroid enema, budesonide, lacking systemic effects for the treatment of distal ulcerative colitis and proctitis. Scand J Gastroenterol 27:9–12
Geboes K, Riddell RH, Öst Å, Jensfelt B, Persson T, Löfberg R (2000) A reproducible grading scale for histological assessment of inflammation in ulcerative colitis. Gut 47:404–409
Källström E, Roscher I, Andreasson A, Back O, van Hage-Hamsten M (2002) Decreased frequency of intracellular IFN-gamma producing T cells in whole blood preparations from patients with atopic dermatitis. Exp Dermatol 11(6):556–563 (Dec)
Schreiber S (2003) Overview of medical treatment. In: Satsangi J et al (eds) Inflammatory bowel disease. Churchill Livingstone, London, pp 297–299
Papadakis KA, Targan SR (2000) Role of cytokines in the pathogenesis of inflammatory bowel disease. Annu Rev Med 51:289–298
Böym A (1964) Separation of white blood cells. Nature 204:793
Lampinen M, Carlson M, Sangfelt P (2001) IL-5 and TNF-alpha participate in recruitment of eosinophils to intestinal mucosa in ulcerative colitis. Dig Dis Sci 46:2004–2009
McCarthy DA, Rampton DS, Liu Y-C (1991) Peripheral blood neutrophils in inflammatory bowel disease: morphological evidence of in vivo activation in active disease. Clin Exp Immunol 86:489–493
Mahida YR (2000) The key role of macrophages in the immunopathogenesis of inflammatory bowel disease. Inflamm Bowel Dis 6:21–33
Meuret G, Bitzi A, Hammer B (1978) Macrophage turnover in Crohn’s disease and ulcerative colitis. Gastroenterol 74:501–503
Rugtveit J, Brandtzaeg P, Halstensen TS, Fausa O, Scott H (1994) Increased macrophage subsets in inflammatory bowel disease: apparent recruitment from peripheral blood monocytes. Gut 35:669–674
Brannigan AE, O’Connell PR, Hurley H (2000) Neutrophil apoptosis is delayed in patients with inflammatory bowel disease. Shock 13:361–366
Tibble JA, Sigthorsson G, Bridger D, Fagerhol MK, Bjarnason I (2000) Surrogate markers of intestinal inflammation are predictive of relapse in patients with inflammatory bowel disease. Gastroenterol 119:15–22
Hanai H, Watanabe F, Takeuchi K, Saniabadi A, Bjarnason I (2003) Leukocyte adsorptive apheresis for the treatment of active ulcerative colitis: a prospective uncontrolled pilot study. Clin Gastroenterol Hepatol 1:28–35
Lee, A, Whyte M, Haslett C (1993) Inhibition of apoptosis and prolongation of neutrophil functional longevity by inflammatory mediators. J Leukoc Biol 54:283–288
Kashiwagi N, Saniabadi A, Shimoyama T (2002) Immunomodulatory effects of granulocyte and monocyte adsorption apheresis as a treatment for patients with ulcerative colitis. Dig Dis Sci 47:1334–1341
Tsukada Y, Nakamura T, Iimura M, Iizuka BE, Hayashi N (2002) Cytokine profile in colonic mucosa of ulcerative colitis correlates with disease activity and response to granulocytapheresis. Am J Gastroenterol 97(11):2820–2828 (Nov)
Sawada K, Ohnishi K, Kosaka T, Chikano S, Yokota Y, Egashira A, Izava H, Yamamura M, Amano K, Satomi M, Shimoyama T (1997) Leucocytopheresis with leukocyte removal filter as new therapy for ulcerative colitis. Ther Apher 1(3):207–211 (Aug)
Liu Z, Geboes K, Colpaert S, D’Haens GR, Rutgeerts P, Ceuppens JL (2000) IL-15 is highly expressed in inflammatory bowel disease and regulates local T cell-dependent cytokine production. J Immunol 164(7):3608–3615 (Apr 1)
Autschbach F, Giese T, Gassler N, Sido B, Heuschen G, Heuschen U, Zuna I, Schulz P, Weckauf H, Berger I, Otto HF, Meuer SC (2002) Cytokine/chemokine messenger-RNA expression profiles in ulcerative colitis and Crohn’s disease. Virchows Arch 441:500–513
Rosenstiel P, Fantini M, Brautigam K, Kuhbacher T, Waetzig GH, Seegert D, Schreiber S (2003) TNF-α and IFN-γ regulate the expression of the NOD2 (CARD15) gene in human intestinal epithelial cells. Gastroenterol 124:1001–1009
Panes J (2001) Inflammatory bowel disease: pathogenesis and targets for therapeutic interventions. Acta Physiol Scand. 173:159–165
Acknowledgements
This work was supported by an unrestricted grant from Terumo Europe NV, and by grants from the Swedish Research Council, the Karolinska Institutet and the Otsuka Frankfurt Research Institute. We thank T. Nieminen, E. Lindroos, and I. Arestrom for their skillful technical assistance.
Author information
Authors and Affiliations
Corresponding author
Additional information
An invited commentary on this paper is available at http://dx.doi.org/10.1007/s00384-005-0082-5
Rights and permissions
About this article
Cite this article
Muratov, V., Lundahl, J., Ulfgren, A.K. et al. Down-regulation of interferon-γ parallels clinical response to selective leukocyte apheresis in patients with inflammatory bowel disease: a 12-month follow-up study. Int J Colorectal Dis 21, 493–504 (2006). https://doi.org/10.1007/s00384-005-0069-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-005-0069-2