Abstract
Purpose
Growth retardation is a severe morbidity in infants with congenital diaphragmatic hernia (CDH). This study aimed to determine when catch-up growth starts in infants with CDH and to determine the adequate amount of nutrition required during catch-up growth.
Methods
This was a multicenter retrospective cohort study involving neonates with isolated CDH (born 2006–2010; n = 98). Weight gain velocity (WGV) was calculated using body weight Z-scores. The minimum required weight gain was defined as WGV ≥ 0. Patients were dichotomized into severe and non-severe cases according to diaphragmatic defects.
Results
Average monthly WGV changed from < 0 to ≥ 0 at 2 months of age. Total caloric intake at 2 months of age was lower when the WGV between 1 and 3 months was < 0 in both severe cases [122 (95% confidence interval (CI) 116–128) vs. 97 (95% CI 84–110) kcal/kg/day, p = 0.02] and non-severe cases [115 (95% CI 110–120) vs. 99 (95% CI 87–111) kcal/kg/day, p < 0.001)].
Conclusion
Catch-up growth started at approximately 2 months of age. During this period, total caloric intake of > 122 kcal/kg/day was needed to avoid decreases in the body weight Z-score in severe cases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Congenital diaphragmatic hernia (CDH) remains a challenging condition encountered by neonatologists and pediatric surgeons. Not only in the acute phase but also in later life, survivors often suffer from various morbidities. Growth retardation was observed in 21–69% of CDH survivors showing Z-scores of < − 2.0 for body weight-for-age at 1 year of age [1,2,3]. Growth retardation has been linked to poor neurodevelopment in both preterm [4] and term infants [5].
We previously reported that the independent risk factors for growth retardation in CDH survivors were not only low birth weight, but also the need for home oxygen treatment (HOT) [1]. This result supports the idea that infants with CDH consume more calorie than normal infants due to respiratory distress, and they need more energy to gain enough body weight [6]. It follows that infants with severe respiratory condition need more energy to grow adequately. Nevertheless, the amount of nutrition for adequate growth has not been elucidated.
Weight growth velocity (WGV) is one of the useful indices for assessing infantile growth. WGV is a commonly used measure in growth and nutrition research in very-low-birth-weight infants, and it is also useful for the non-constant change in body weight [7]. Gien et al. calculated the overall WGV from birth to discharge among CDH infants and reported that WGV during hospitalization was evidently lower in CDH infants than in normal infants. The slope of WGV, however, was not constant; there were often periods of negative WGV in the acute phase, followed by periods of positive WGV [8]. Leeuwen et al. performed anthropometric measurements among infants with CDH at 3, 6, and 12 months of age and reported that catch-up growth occurred during infancy [2]. These findings suggest that early adequate nutritional support would be crucial during catch-up growth. Nevertheless, it remains unknown when catch-up growth begins and how we should manage it.
Therefore, the purposes of this study were (1) to determine when catch-up growth starts in infants with CDH and (2) to assess the adequate amount of nutrition required during the catch-up growth.
Methods
Patient sample
A nationwide multicenter retrospective observational study of neonatal CDH was conducted by the Japanese Congenital Diaphragmatic Hernia Study Group in 2011 [9]. Data from 614 patients with CDH in 72 institutions were collected between January 2006 and December 2010. Subsequently, an additional survey focusing on nutritional management was conducted by five high-volume centers that declared their intention to participate in the study. This study included patients who survived to discharge in the five participating institutions between 2006 and 2010. Patients who had chromosome abnormalities, severe cardiac malformation, or very low birth weights were excluded.
Variables
Data on body weight and nutrition were extracted from medical records. Body weights, measured at 1, 2, and 3 months and at 1.5 and 3 years of age, were used to indicate growth. The daily doses and types of nutrition at 1, 2, and 3 months of age were also retrieved from the medical records. Daily caloric intakes of enteral nutrition (EN) were calculated, using 0.66 kcal/mL and 0.67 kcal/mL when mother’s milk or formula milk was given, respectively. When patients were fed on demand, the daily dose of EN was estimated to be 180 mL/kg/day. The daily amounts of glucose and protein in parenteral nutrition (PN) were retrieved from the prescription. The total amount of nutrition was defined to be simply the addition of PN to EN.
Data of other clinical variables were extracted from the database that was previously constructed by the Japanese Congenital Diaphragmatic Hernia Study Group [1, 9]. The variables included sex, gestational age, birth weight, international classification of the diaphragmatic defect [10], Terui’s risk stratification of CDH severity using Apgar score at 1 min, best oxygenation index (calculated using the highest PaO2 from the preductal artery within 24 h after birth and ventilator settings) [11], total caloric intake at 1, 2, and 3 months of age, WGV, amount of PN at 1, 2, and 3 months of age, rate of PN use, rates of gastroesophageal reflux (GER) and chylothorax during hospitalization, tracheal intubation duration of ≥ 30 days (including tracheotomy), and need for HOT. A “large diaphragmatic defect” was defined as a diaphragmatic defect of > 50% of the portion of the chest wall devoid of the diaphragm tissue; this corresponds to the C + D international classification [10]. The patients were dichotomized into the following groups depending on the size of the diaphragmatic defect: severe cases with a large diaphragmatic defect and non-severe cases with a small diaphragmatic defect.
Weight gain velocity
The Z-scores for body weights were calculated according to the patients’ sex, using the average values and the standard deviations for weight at each month/year of age. These values were obtained from the national databases from 12,426 infants and 695,600 school children, respectively [12, 13]. WGV of each period was calculated by dividing changes in the Z-score for body weight by the number of month(s). WGV was used as an indicator of growth and comprised the primary outcome of this study. For instance, when WGV is zero, the patient grows along the line of the standard growth curve; when WGV is positive, the patient may be in catching-up process. The time when WGV changes from negative (< 0) to positive (≥ 0) was taken as the start of catch-up growth.
An exploratory analysis was conducted. WGV during the period of catch-up growth was calculated, and the patients were divided into two groups according to the presence of positive and negative WGV. To assess the risk of negative WGV, the variables were compared between the positive and negative WGV groups. To elucidate the adequate amount of nutrition during catch-up growth, the amount of nutrition between the positive and negative WGV groups was compared.
Statistical analysis
Summary statistics were expressed as frequencies and proportions for categorical data and a means ± standard deviations or 95% confidence intervals (CIs) for continuous variables. Statistical comparison between the two groups was tested using the unpaired t test or Mann–Whitney U test for continuous variables and the Chi-square test or Fisher's exact test for categorical variables. A mixed effects model for repeated measures was used to determine between-group differences in mean changes in Z-scores for body weight, WGV and total calorie.
p < 0.05 was defined as indicating statistical significance. All statistical analyses were performed using the JMP software program, version 12.01 (SAS Institute, Inc., Cary, NC, USA).
Ethical approval
The study design was approved by the Research Ethics Committee of the Graduate School of Medicine, Chiba University (no. 509), and the independent ethics committees of the four other participating institutions (no. 11017 in Osaka University, no. 25–222 in Kyusyu University, no. 2016–0416 in Nagoya University, and no. 468 in Osaka Women's and Children's Hospital). Written informed consent was not required, as this was a retrospective study with de-identified data. The details of the study were published on the institutional website, and individuals were guaranteed the right to decline participation in the study. The study was performed in accordance with the principles of the Declaration of Helsinki and the Ethical Guidelines for Medical and Health Research Involving Human Subjects of the Japanese government.
Results
Patient data
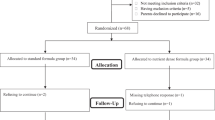
A total of 141 infants who were born with CDH and received treatment for the disease at the five participating institutions were included. Of them, 109 (77%) survived to discharge. Patients with chromosome abnormalities (n = 3), severe cardiac anomaly (n = 5), and very low birth weights (n = 3) were excluded. The remaining 98 patients were included in the present study.
Twenty-five and 73 patients had severe and non-severe CDH, respectively. Demographic data of patients with severe and non-severe cases are presented in Table 1. Patients’ background (sex, gestational week, and birth weight) did not significantly differ between the two groups. Body weight Z-score at 2 months (− 2.897 ± 0.718 vs. − 2.218 ± 1.121, p < 0.01) and 3 months (− 2.852 ± 0.792 vs. − 1.789 ± 1.240, p < 0.001) was lower in the severe group than in the non-severe group. The potential risk factors for malnutrition did not significantly differ between the severe and non-severe groups. The rate of tracheal intubation for ≥ 30 days [13/25 (52%) vs. 13/73 (18%), p < 0.01] and the need for HOT [5/25 (20%) vs. 2/73 (3%), p = 0.01] significantly differed between the two groups.
Weight gain velocity
Table 1 shows that WGV between 1 and 2 months was lower in the severe group than in the non-severe group (− 0.45 ± 0.60 vs. 0.00 ± 0.09, p < 0.01). WGV between birth and 3 months was significantly different between the severe and non-severe group (− 0.72 ± 0.41 vs. − 0.42 ± 0.43, p < 0.01); however, there was no difference in WGV between birth and 1.5 years (− 0.03 ± 0.08 vs. 0.00 ± 0.07, p = 0.13).
Change in the body weight Z-score is shown in Fig. 1a. The average WGV changed from negative (< 0) to positive (≥ 0) at 2 months of age (WGV between 0 and 1 month, − 1.53/month; WGV between 1 and 2 months, − 0.20/month; WGV between 2 and 3 months, + 0.34/month; WGV between 3 months and 1.5 years, + 1.32/month; WGV between 1.5 and 3 years, + 0.03/month). Figure 1b shows the changes in the body weight Z-score in the dichotomized cohort of severe and non-severe cases. In the severe cases, the bottom of the Z-score was at least after 3 months of age, whereas the bottom of the Z-score in non-severe cases was after 2 months of age.
Risk of negative WGV
Changes in WGV from negative to positive were observed at 2 months of age. Thus, the risk of negative WGV between 1 and 3 months was assessed in severe and non-severe cases (Table 2). In severe cases, positive and negative WGV values between 1 and 3 months were 0.33 (95% CI − 0.03 to 0.66) and − 0.42 (95% CI − 0.57 to − 0.30), respectively (p < 0.001). In non-severe cases, positive and negative WGV values between 1 and 3 months were 0.39 (95% CI 0.30–0.48) and -0.27 (95% CI − 0.36 to − 0.18), respectively (p < 0.001). Total caloric intake at 2 months of age was lower in the negative WGV group than in the positive WGV group in both severe [122 (95% CI 116–128) vs. 97 (95% CI 84–110) kcal/kg/day, p = 0.02] and non-severe cases [115 (95% CI 110–120) vs. 99 (95% CI 87–111) kcal/kg/day, p < 0.001] (Fig. 2). In non-severe cases, the rate of chylothorax was higher in the negative WGV group than in the positive WGV group [8/46 (17%) vs. 12/24 (50%), p < 0.001].
Comparison of total caloric intake at 2 months of age between positive and negative weight gain velocity (WGV) groups in both severe and non-severe cases. WGV was calculated by dividing the changes in body weight Z-score between 1 and 3 months by 2 months. Whiskers represent 95% confidence intervals. *p < 0.01
Discussion
The principal findings of this study, in which the WGV of 98 infants with CDH was analyzed retrospectively, were as follows: (1) catch-up growth of infants with CDH started at approximately 2 months of age according to the body weight trajectory, (2) the risk of negative WGV between 1 and 3 months was lower total caloric intake at 2 months of age in both severe and non-severe cases, and (3) 122 kcal/kg/day of total caloric intake was needed at least to achieve positive WGV in severe cases.
Growth retardation is one of the serious morbidities of infants with CDH. In our cohort, growth retardation was observed in 23% of the CDH survivors [1]. Various factors may be associated with poor growth during infancy, including the fact that patients with CDH are sometimes intolerant to EN due to cardiorespiratory instability, deep sedation, or restrictions in volume loading. GER, oral aversion, and allergies can also contribute to difficulties in enteral feeding [14, 15]. We previously reported that EN and supportive PN in the acute phase were essential for weight gain during infancy [16]. Furthermore, increase in the energy requirement may be an underestimated factor [17]. Halibourton et al. reported that 59% of patients with CDH were hypermetabolic with a high resting energy expenditure, and 30% more energy was needed for ideal body weight gain [6]. We previously reported that the need for HOT was an independent risk factor for growth retardation in CDH survivors [1]. These findings indicated that increased energy requirement in infants with CDH was a considerable risk factor of growth retardation. However, minimal evidence has been available mainly because a precise measurement of resting energy expenditure is difficult in infants. It is also difficult to define “adequate growth” in each individual. Halibourton et al. used different approaches to this issue. They showed that body mass index correlated with lung function in CDH survivors. This finding supports the hypothesis that increased respiratory effort results in slow growth. The hypothesis has not been proved completely because the correlation between lung function and resting energy expenditure was not observed in their study [18].
Catch-up growth is defined as an accelerated compensatory growth of an organism following a period of slowed development, particularly as a result of nutrient deprivation [19]. Catch-up growth during infancy can be directly related to improved neurodevelopment [4, 5]. Evidence, therefore, has been accumulated in preterm infants [20]. Furthermore, nutrient deprivation during the neonatal period is seen not only in preterm infants, but also in term infants requiring surgery and/or intensive care. Correia Martins et al. reported that earlier surgical closure of ventricular septal defects resulted in better acceleration of postoperative growth than later surgery [21]. However, there has been scarce evidence on catch-up growth in term infants who underwent other types of surgeries. To the best of our knowledge, this is the first report to provide new insights into catch-up growth in infants with CDH.
To assess the catch-up growth of infants with CDH, WGV based on the Z-score was used in the present study. This method has the following advantages: (1) the growth of each infant can be rigorously assessed through standardization rather than through the absolute value of body weight; (2) growth can be evaluated dynamically, rather than the value at one point, using the concept of velocity; and (3) the value of WGV calculated based on the Z-score can be easily interpreted, with 0 indicating growth along the line of the standard growth curve and the positive value indicating accelerated growth over the line of the standard growth curve.
We identified that catch-up growth starts at approximately 2 months of age in infants with CDH. Then, the risk of negative WGV around this period was assessed. To eliminate the bias of severity of CDH, the cohort was divided into two groups (severe and non-severe cases). We found that the lower amount of nutrition at 1 and 2 month(s) of age was the significant risk factor both in severe and non-severe groups. We also found that negative WGV between 1 and 3 months resulted in negative WGV between birth and 1.5 years of age in non-severe groups. These data indicated that the less amount of nutrition during infancy subsequently leads to less catch-up growth at least in non-severe cases. The reason why WGV between birth and 1.5 years in severe cases had no difference between cases with positive and negative WGV between 1 and 3 months was unclear. Various factors such as recurrence of CDH, severe GER or respiratory distress may affect the outcome.
By comparing the positive and negative WGV groups, finally, we found that 122 kcal/kg/day of total caloric intake was needed at least to achieve positive WGV in severe cases. However, the target amount of nutrition for adequate catch-up growth remains unclear. Haliburton et al. reported that a caloric intake of 125 kcal/kg/day at discharge from the hospital was required to achieve an adequate weight gain (25–35 g/day) [6]. Although it is unclear whether or not additional 3 kcal/kg/day is enough for adequate catch-up growth, 125 kcal/kg/day might be a potential target amount of nutrition. We have now established a nutritional support program involving a high concentration of milk; we are currently applying the program in the clinical setting. A key point is to evaluate the nutritional status of the individual repeatedly and increase the amount of nutrition until an adequate body weight gain can be ensured.
In the present study, we had originally expected that severe cases would require more calories for positive WGV than non-severe cases; however, the obtained result was different, as there was no significant difference between severe and non-severe cases. This finding may be due to the fact that we assessed only the minimum amount of nutrition to prevent a further decrease in the body-weight Z-score. The adequate caloric intake for an adequate WGV possibly differed between these groups. Further studies are needed to validate this finding.
Interestingly, chylothorax was the risk factor for negative WGV only in the non-severe cases. Chylothorax is a significant postoperative complication that occurs in 5–6% of patients with CDH [22,23,24]; the rate of chylothorax was higher in more severe cases [24]. More than 80% of patients with CDH experiencing chylothorax were effectively treated by non-surgical management, including fasting and medication [24]. This fasting management may have a potential risk for malnutrition if the PN is not appropriately applied. Our data suggest that, even in non-severe cases, chylothorax is a considerable risk factor for growth retardation.
Our study had several limitations. First, because of the multicenter retrospective study design, the therapeutic strategies employed in the five participating institutions were not uniform, and they totally depended on the policies of the facility and decisions of the attending physicians. The strategies included treatment of CDH, nutritional management strategy, and follow-up programs. These may have resulted in a bias in the findings. Second, neither respiratory function nor resting energy expenditure was measured. The relationship between respiratory effort and growth, therefore, could not be discussed. Further prospective studies with more detailed data are warranted to validate our findings. Third, we only assessed the force feeding, and the daily dose of EN on demand was tentatively assigned as 180 mL/kg/day. These may have resulted in incorrectness of analysis. The present study will need to be supported by further prospective studies that assess the nutrition in more detail.
In conclusion, catch-up growth started at approximately 2 months of age. Insufficient WGV during this period resulted in inadequate catch-up growth. Total caloric intake of122 kcal/kg/day was needed to avoid a decrease in the body weight Z-score in severe cases. Given that the ideal nutritional management for adequate catch-up growth in infants with CDH remains unclear, further studies are needed to clarify this.
Code availability
The datasets during the current study are available from the corresponding author on reasonable request.
References
Terui K, Nagata K, Hayakawa M, Okuyama H, Goishi K, Yokoi A, Tazuke Y, Takayasu H, Yoshida H, Usui N (2016) Growth assessment and the risk of growth retardation in congenital diaphragmatic hernia: a long-term follow-up study from the Japanese Congenital Diaphragmatic Hernia Study Group. Eur J Pediatr Surg 26:60–66. https://doi.org/10.1055/s-0035-1566094
Leeuwen L, Walker K, Halliday R, Karpelowsky J, Fitzgerald DA (2014) Growth in children with congenital diaphragmatic hernia during the first year of life. J Pediatr Surg 49:1363–1366. https://doi.org/10.1016/j.jpedsurg.2014.02.081
Cortes RA, Keller RL, Townsend T, Harrison MR, Farmer DL, Lee H, Piecuch RE, Leonard CH, Hetherton M, Bisgaard R, Nobuhara KK (2005) Survival of severe congenital diaphragmatic hernia has morbid consequences. J Pediatr Surg 40:36–45. https://doi.org/10.1016/j.jpedsurg.2004.09.037
Ehrenkranz RA, Dusick AM, Vohr BR, Wright LL, Wrage LA, Poole WK (2006) Growth in the neonatal intensive care unit influences neurodevelopmental and growth outcomes of extremely low birth weight infants. Pediatrics 117:1253–1261. https://doi.org/10.1542/peds.2005-1368
Heinonen K, Raikkonen K, Pesonen AK, Kajantie E, Andersson S, Eriksson JG, Niemelä A, Vartia T, Peltola J, Lano A (2008) Prenatal and postnatal growth and cognitive abilities at 56 months of age: a longitudinal study of infants born at term. Pediatrics 121:e1325–e1333. https://doi.org/10.1542/peds.2007-1172
Haliburton B, Chiang M, Marcon M, Moraes TJ, Chiu PP, Mouzaki M (2016) Nutritional intake, energy expenditure, and growth of infants following congenital diaphragmatic hernia repair. J Pediatr Gastroenterol Nutr 62:474–478. https://doi.org/10.1097/MPG.0000000000001000
Fenton TR, Anderson D, Groh-Wargo S, Hoyos A, Ehrenkranz RA, Senterre T (2018) An attempt to standardize the calculation of growth velocity of preterm infants-evaluation of practical bedside methods. J Pediatr 196:77–83. https://doi.org/10.1016/j.jpeds.2017.10.005
Gien J, Murthy K, Pallotto EK, Brozanski B, Chicoine L, Zaniletti I, Seabrook R, Keene S, Alapati D, Porta N, Rintoul N, Grover TR, Children’s Hospitals Neonatal Consortium CDH Study Group (2017) Short-term weight gain velocity in infants with congenital diaphragmatic hernia (CDH). Early Hum Dev 106–107:7–12. https://doi.org/10.1016/j.earlhumdev.2017.01.010
Nagata K, Usui N, Kanamori Y, Takahashi S, Hayakawa M, Okuyama H, Inamura N, Fujino Y, Taguchi T (2013) The current profile and outcome of congenital diaphragmatic hernia: a nationwide survey in Japan. J Pediatr Surg 48:738–744. https://doi.org/10.1016/j.jpedsurg.2012.12.017
Lally KP, Lasky RE, Lally PA, Bagolan P, Davis CF, Frenckner BP, Hirschl RM, Langham MR, Buchmiller TL, Usui N, Tibboel D, Wilson JM, Congenital Diaphragmatic Hernia Study Group (2013) Standardized reporting for congenital diaphragmatic hernia—an international consensus. J Pediatr Surg 48:2408–2415. https://doi.org/10.1016/j.jpedsurg.2013.08.014
Terui K, Nagata K, Kanamori Y, Takahashi S, Hayakawa M, Okuyama H, Inamura N, Yoshida H, Taguchi T, Usui N (2017) Risk stratification for congenital diaphragmatic hernia by factors within 24 hours after birth. J Perinatol 37:805–808. https://doi.org/10.1038/jp.2017.11
Japanese Ministry of Health, Labour and Welfare. Report of the national growth survey of normal Japanese infants, 0–5 years of age. https://www.mhlw.go.jp/toukei/list/73-22.html. Accessed 1 Dec 2019
Japanese Ministry of Education, Culture, Sports, Science and Technology. School health examination survey database. https://www.e-stat.go.jp/SG1/estat/NewList.do?tid=000001011648f. Accessed 1 Dec 2019
Terui K, Taguchi T, Goishi K, Hayakawa M, Tazuke Y, Yokoi A, Takayasu H, Okuyama H, Yoshida H, Usui N, Japanese Congenital Diaphragmatic Hernia Study Group (2014) Prognostic factors of gastroesophageal reflux disease in congenital diaphragmatic hernia: a multicenter study. Pediatr Surg Int 30:1129–1134. https://doi.org/10.1007/s00383-014-3594-7
Huston RK, Baxter LM, Larrabee PB (2009) Neonatal parenteral nutrition hypersensitivity: a case report implicating bisulfite sensitivity in a newborn infant. JPEN J Parenter Enteral Nutr 33:691–693. https://doi.org/10.1177/0148607109347643
Terui K, Usui N, Tazuke Y, Nagata K, Ito M, Okuyama H, Hayakawa M, Taguchi T, Sato Y, Yoshida H (2019) Impact of nutrition in the treatment of congenital diaphragmatic hernia. Pediatr Int 61:482–488. https://doi.org/10.1111/ped.13837
Fitting JW, Frascarolo P, Jéquier E, Leuenberger P (1990) Resting energy expenditure in interstitial lung disease. Am Rev Respir Dis 142:631–635. https://doi.org/10.1164/ajrccm/142.3.631
Haliburton B, Mouzaki M, Chiang M, Scaini V, Marcon M, Duan W, Wilson D, Chiu PP, Moraes TJ (2017) Pulmonary function and nutritional morbidity in children and adolescents with congenital diaphragmatic hernia. J Pediatr Surg 52:252–256. https://doi.org/10.1016/j.jpedsurg.2016.11.020
Cooke RJ (2010) Catch-up growth: implications for the preterm and term infant. Eur J Clin Nutr 64:S8–S10. https://doi.org/10.1038/ejcn.2010.40
Van de Pol C, Allegaert K (2020) Growth patterns and body composition in former extremely low birth weight (ELBW) neonates until adulthood: a systematic review. Eur J Pediatr. https://doi.org/10.1007/s00431-019-03552-z
Correia Martins L, Lourenço R, Cordeiro S, Carvalho N, Mendes I, Loureiro M, Patrício M, Anjos R (2016) Catch-up growth in term and preterm infants after surgical closure of ventricular septal defect in the first year of life. Eur J Pediatr 175:573–579. https://doi.org/10.1007/s00431-015-2676-4
Kamiyama M, Usui N, Tani G, Soh H, Kamata S, Nose K, Kubota A, Fukuzawa M (2010) Postoperative chylothorax in congenital diaphragmatic hernia. Eur J Pediatr Surg 20:391–394. https://doi.org/10.1055/s-0030-1261956
Mills J, Safavi A, Skarsgard ED, Canadian Pediatric Surgery Network (CAPSNet) (2012) Chylothorax after congenital diaphragmatic hernia repair: a population-based study. J Pediatr Surg 47:842–846. https://doi.org/10.1016/j.jpedsurg.2012.01.031
Levy SM, Lally PA, Lally KP, Tsao K, Congenital Diaphragmatic Hernia Study Group (2013) The impact of chylothorax on neonates with repaired congenital diaphragmatic hernia. J Pediatr Surg 48:724–729. https://doi.org/10.1016/j.jpedsurg.2012.11.035
Acknowledgements
This work was supported by a grant from the Ministry of Health, Labour and Welfare of Japan [grant number H24-Nanchi-Ippan-034, 2002].
Funding
This work was supported by a grant from the Ministry of Health, Labour and Welfare of Japan [grant number H24-Nanchi-Ippan-034, 2002].
Author information
Authors and Affiliations
Contributions
K.T. designed the study and wrote the initial draft of the manuscript. Y.T., K.N., M.I., H.O., M.H., T.T., Y.S., and H.Y. contributed to the analysis and interpretation of data and assisted in the preparation of the manuscript. All other authors have contributed to the data collection and interpretation as well as the critical review of the manuscript. The final version of the manuscript was approved by all authors.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest.
Ethics approval
The study design was approved by the Research Ethics Committee of the Graduate School of Medicine, Chiba University (no. 509), and the independent ethics committees of the four other participating institutions. The study was performed in accordance with the principles of the Declaration of Helsinki and the Ethical Guidelines for Medical and Health Research Involving Human Subjects.
Consent to participate
Signed informed consent was not required, as this was a retrospective study with de-identified data. The details of the study have been published on the institutional website and individuals have been guaranteed the right to decline participation in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Terui, K., Tazuke, Y., Nagata, K. et al. Weight gain velocity and adequate amount of nutrition for infants with congenital diaphragmatic hernia. Pediatr Surg Int 37, 205–212 (2021). https://doi.org/10.1007/s00383-020-04785-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-020-04785-y