Abstract
Aim
This study reviewed the literature on the postoperative complications following laparoscopic-assisted anorectoplasty (LAARP).
Methods
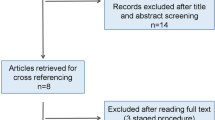
A Medline and Embase search was performed for the terms “anorectal malformation” (ARM) “laparoscopic” and “complication”. Articles without English full text, review articles, systematic reviews, case reports, case series < 5 cases and duplicate articles were excluded. Two reviewers independently performed the eligibility assessment and data extraction. Data were collected for type of malformation, surgical technique, postoperative complications and functional outcomes
Results
The search retrieved 108 articles, of which 38 met the inclusion criteria and offered 1058 patients for analysis. Rectoprostatic and rectobladder neck fistula were the most common types of ARM in males, whereas it was the common cloaca in females. Analysis of complications demonstrated rectal prolapse (n = 149; 14.08%) being the most prominent, followed by urethral diverticulum (n = 32; 3.02%), anal stenosis (n = 37; 3.49%), recurrent fistula (n = 7; 0.66%) and rectal stricture (n = 4; 0.37%). Krickenbeck classification was used for functional assessment in 638 patients, with fecal soiling grade 2 or > 2 in 79. Data on functional outcome specific to the type of malformation was available for 246 patients: fecal soiling grade 2 or > 2 in 15/94 (15.95%) with rectoprostatic fistula, 26/73 (35.61%) with rectobladder neck fistula, 6/47 (12.76%) with common cloaca, and 1/22 (4.54%) with no fistula.
Conclusion
Rectal prolapse, posterior urethral diverticulum and anal stenosis are the most common complications after LAARP. Inconsistent and non-uniform functional assessment and non-availability of information about the sacrum and spine make it difficult to analyze the functional outcome following LAARP.

Similar content being viewed by others
References
DeVries PA, Peña A (1982) Posterior sagittal anorectoplasty. J Pediatr Surg 17:638–643. https://doi.org/10.1016/s0022-3468(82)80126-7
Georgeson KE, Inge TH, Albanese CT. Laparoscopically assisted anorectal pull-through for high imperforate anus--a new technique. J Pediatr Surg. 2000 ;35 :927–30; discussion 930–1. doi: https://doi.org/10.1053/jpsu.2000.6925.
Han Y, Xia Z, Guo S, Yu X, Li Z (2017) Laparoscopically assisted anorectal pull-through versus posterior sagittal anorectoplasty for high and intermediate anorectal malformations: a systematic review and meta-analysis. PLoS ONE 12(1):e0170421. https://doi.org/10.1371/journal.pone.0170421
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med 151:W65–W94
Iwanaka T, Arai M, Kawashima H, Kudou S, Fujishiro J, Matsui A, Imaizumi S (2003) Findings of pelvic musculature and efficacy of laparoscopic muscle stimulator in laparoscopy-assisted anorectal pull-through for high imperforate anus. Surg Endosc 17:278–281. https://doi.org/10.1007/s00464-002-9054-9
Tei E, Yamataka A, Segawa O, Kobayashi H, Lane GJ, Tobayama S, Kameoka S, Miyano T (2003) Laparoscopically assisted anorectovaginoplasty for selected types of female anorectal malformations. J Pediatr Surg 38:1770–1774. https://doi.org/10.1016/j.jpedsurg.2003.08.018
Kudou S, Iwanaka T, Kawashima H, Uchida H, Nishi A, Yotsumoto K, Kaneko M (2005) Midterm follow-up study of high-type imperforate anus after laparoscopically assisted anorectoplasty. J Pediatr Surg 40:1923–1926. https://doi.org/10.1016/j.jpedsurg.2005.08.008
Ichijo C, Kaneyama K, Hayashi Y, Koga H, Okazaki T, Lane GJ, Kurosaki Y, Yamataka A. Midterm postoperative clinicoradiologic analysis of surgery for high/intermediate-type imperforate anus: prospective comparative study between laparoscopy-assisted and posterior sagittal anorectoplasty. J Pediatr Surg. 2008;43:158–62; discussion 162–3. doi: https://doi.org/10.1016/j.jpedsurg.2007.09.037.
El-Debeiky MS, Safan HA, Shafei IA, Kader HA, Hay SA (2009) Long-term functional evaluation of fecal continence after laparoscopic-assisted pull-through for high anorectal malformations. J Laparoendosc Adv Surg Tech A 19(Suppl 1):S51–S54. https://doi.org/10.1089/lap.2008.0135.supp
Podevin G, Petit T, Mure PY, Gelas T, Demarche M, Allal H, Becmeur F, Varlet F, Philippe P, Weil D, Heloury Y (2009) Minimally invasive surgery for anorectal malformation in boys: a multicenter study. J Laparoendosc Adv Surg Tech A 19(Suppl 1):S233–S235. https://doi.org/10.1089/lap.2008.0137.supp
Bhandary KS, Kumaran V, Rajamani G, Kannan S, Mohan NV, Rangarajan R, Muthulingam V (2009) Laparoscopic assisted anorectal pull through: reformed techniques. J Indian Assoc Pediatr Surg 14:210–214. https://doi.org/10.4103/0971-9261.59604
Koga H, Miyano G, Takahashi T, Shimotakahara A, Kato Y, Lane GJ, Okazaki T, Yamataka A (2010) Comparison of anorectal angle and continence after Georgeson and Peña procedures for high/intermediate imperforate anus. J Pediatr Surg 45:2394–2397. https://doi.org/10.1016/j.jpedsurg.2010.08.041
Bailez MM, Cuenca ES, Di Benedetto V, Solana J. Laparoscopic treatment of rectovaginal fistulas. Feasibility, technical details, and functional results of a rare anorectal malformation. J Pediatr Surg. 2010;45:1837–42. doi: https://doi.org/10.1016/j.jpedsurg.2010.02.064.
Kimura O, Iwai N, Sasaki Y, Tsuda T, Deguchi E, Ono S, Furukawa T (2010) Laparoscopic versus open abdominoperineal rectoplasty for infants with high-type anorectal malformation. J Pediatr Surg 45:2390–2393. https://doi.org/10.1016/j.jpedsurg.2010.08.042
Bailez MM, Cuenca ES, Mauri V, Solana J, Di Benedetto V (2011) Outcome of males with high anorectal malformations treated with laparoscopic-assisted anorectal pull-through: preliminary results of a comparative study with the open approach in a single institution. J Pediatr Surg 46:473–477. https://doi.org/10.1016/j.jpedsurg.2010.08.007
Tong QS, Tang ST, Pu JR, Mao YZ, Wang Y, Li SW, Cao QQ, Ruan QL (2011) Laparoscopically assisted anorectal pull-through for high imperforate anus in infants: intermediate results. J Pediatr Surg 46:1578–1586. https://doi.org/10.1016/j.jpedsurg.2011.04.059
England RJ, Warren SL, Bezuidenhout L, Numanoglu A, Millar AJ (2012) Laparoscopic repair of anorectal malformations at the Red Cross War Memorial Children's Hospital: taking stock. J Pediatr Surg 47:565–570. https://doi.org/10.1016/j.jpedsurg.2011.08.006
Jung SM, Lee SK, Seo JM (2013) Experience with laparoscopic-assisted anorectal pull-through in 25 males with anorectal malformation and rectourethral or rectovesical fistulae: postoperative complications and functional results. J Pediatr Surg 48:591–596. https://doi.org/10.1016/j.jpedsurg.2012.08.001
Bischoff A, Peña A, Levitt MA (2013) Laparoscopic-assisted PSARP—the advantages of combining both techniques for the treatment of anorectal malformations with recto-bladder neck or high prostatic fistulas. J Pediatr Surg 48:367–371. https://doi.org/10.1016/j.jpedsurg.2012.11.019
Liem NT, Quynh TA (2012) Laparoscopic rectal pull-through for persistent cloaca: an easier approach for a complex anomaly. J Pediatr Surg 47:815–818. https://doi.org/10.1016/j.jpedsurg.2012.02.004
Yamataka A, Goto S, Kato Y, Koga H, Lane GJ, Okazaki T (2012) Fecal and urinary continence after scope-assisted anorectovaginoplasty for female anorectal malformation. Pediatr Surg Int 28:907–912. https://doi.org/10.1007/s00383-012-3141-3(PMID: 22940880)
Liem NT, Quynh TA (2013) Combined laparoscopic and modified posterior sagittal approach saving the external sphincter for rectourethral fistula: an easier and more physiologic approach. J Pediatr Surg 48:1450–1453. https://doi.org/10.1016/j.jpedsurg.2013.03.007
Japanese multicenter study group on male high imperforate anus. Multicenter retrospective comparative study of laparoscopically assisted and conventional anorectoplasty for male infants with rectoprostatic urethral fistula. J Pediatr Surg. 2013;48:2383–8. doi: https://doi.org/10.1016/j.jpedsurg.2013.08.010.
van der Zee DC, Dik P, Beek FJ (2013) Laparoscopy-assisted anorectal pull-through in anorectal malformations: a reappraisal. World J Surg 37:1934–1939. https://doi.org/10.1007/s00268-013-2017-6
Ming AX, Li L, Diao M, Wang HB, Liu Y, Ye M, Cheng W (2014) Long term outcomes of laparoscopic-assisted anorectoplasty: a comparison study with posterior sagittal anorectoplasty. J Pediatr Surg 49:560–563. https://doi.org/10.1016/j.jpedsurg.2013.11.060
Yang L, Tang ST, Li S, Aubdoollah TH, Cao GQ, Lei HY, Wang XX (2014) Two-stage laparoscopic approaches for high anorectal malformation: transumbilical colostomy and anorectoplasty. J Pediatr Surg 49:1631–1634. https://doi.org/10.1016/j.jpedsurg.2014.05.014
Wang C, Li L, Cheng W, Liu S, Diao M, Li X, Qiao G, Zhang Z, Chen Z (2015) A new approach for persistent cloaca: laparoscopically assisted anorectoplasty and modified repair of urogenital sinus. J Pediatr Surg 50:1236–1240. https://doi.org/10.1016/j.jpedsurg.2015.04.016
Minaev SV, Kirgizov IV, Gladkyy A, Shishkin I, Gerasimenko I (2017) Outcome of laparoscopic treatment of anorectal malformations in children. World J Surg 41:625–629. https://doi.org/10.1007/s00268-016-3699-3
Yazaki Y, Koga H, Ochi T, Okawada M, Doi T, Lane GJ, Yamataka A. Surgical management of recto-prostatic and recto-bulbar anorectal malformations. Pediatr Surg Int. 2016;32:939–44. https://doi.org/10.1007/s00383-016-3948-4
Diao M, Li L, Ye M, Guan KP, Wei YD, Cheng W (2016) Congenital anomaly rectified at birth: one-stage single-incision laparoscopic-assisted anorectoplasty for newborns with anorectal malformations and recto-urethral fistula. Surg Endosc 30:5156–5164. https://doi.org/10.1007/s00464-016-4841-x
Samuk I, Bischoff A, Hall J, Levitt M, Peña A (2016) Anorectal malformation with rectobladder neck fistula: a distinct and challenging malformation. J Pediatr Surg 51:1592–1596. https://doi.org/10.1016/j.jpedsurg.2016.06.001
Wang C, Li L, Diao M, Liu S, Zhang J, Chen Z, Li X, Cheng W (2016) Single-incision laparoscopic-assisted anorectoplasty for the management of persistent cloaca. J Laparoendosc Adv Surg Tech A 26:328–333. https://doi.org/10.1089/lap.2015.0296
Diao M, Li L, Guan KP, Zhang Z, Cheng W (2017) A novel laparoscopic technique for anorectal malformation with low recto-bulbar fistulae. Surg Endosc 31:4326–4330. https://doi.org/10.1007/s00464-017-5483-3(Epub 2017 Mar 13 PMID: 28289973)
Tainaka T, Uchida H, Tanaka Y, Hinoki A, Shirota C, Sumida W, Yokota K, Makita S, Oshima K, Chiba K, Ishimaru T, Kawashima H. Long-term outcomes and complications after laparoscopic-assisted anorectoplasty vs. posterior sagittal anorectoplasty for high- and intermediate-type anorectal malformation. Pediatr Surg Int. 2018;34:1111–1115. doi: https://doi.org/10.1007/s00383-018-4323-4.
Ren X, Xiao H, Li L, Diao M, Chen L, Zhou R, Li H, Li X, Cheng W (2018) Single-incision laparoscopic-assisted anorectoplasty versus three-port laparoscopy in treatment of persistent cloaca: a midterm follow-up. J Laparoendosc Adv Surg Tech A 28:1540–1547. https://doi.org/10.1089/lap.2018.0225
Xiao H, Huang R, Cui X, Chen L, Diao M, Li L (2018) Single-incision laparoscopic versus conventional laparoscopic surgery for rectobladderneck and rectoprostatic anorectal malformations. J Laparoendosc Adv Surg Tech A 28:1553–1557. https://doi.org/10.1089/lap.2018.0260
Xiao H, Chen L, Ren XH, Huang R, Diao M, Li L (2018) One-stage laparoscopic-assisted anorectoplasty for neonates with anorectal malformation and recto-prostatic or recto-bulbar fistula according to the krickenbeck classification. J Laparoendosc Adv Surg Tech A 28:1029–1034. https://doi.org/10.1089/lap.2017.0690
Xiao H, Huang R, Chen L, Diao M, Cheng W, Li L, Cui XD (2018) The midterm outcomes of 1-stage versus 3-stage laparoscopic-assisted anorectoplasty in anorectal malformations with rectoprostatic fistula and rectobulbar fistula: a retrospective cohort study. Medicine (Baltimore) 97:e11843. https://doi.org/10.1097/MD.0000000000011843
Tran QA, Nguyen LT, Pham HD, Nguyen TTN, Nguyen XV (2019) Follow-up outcomes of laparoscopic-assisted anorectal pull through for anorectal malformations of high type. J Laparoendosc Adv Surg Tech A 29:1497–1500. https://doi.org/10.1089/lap.2018.0163
Ren X, Xu H, Jiang Q, Diao M, Li X, Li L (2019) Single-incision laparoscopic-assisted anorectoplasty for treating children with intermediate-type anorectal malformations and rectobulbar fistula: a comparative study. Pediatr Surg Int 35:1255–1263. https://doi.org/10.1007/s00383-019-04549-3
Gurusamy R, Raj SV, Maniam R, Regunandan SR (2017) Laparoscopic-assisted anorectoplasty: a single-center experience. J Indian Assoc Pediatr Surg 22:114–118. https://doi.org/10.4103/jiaps.JIAPS_266_16
Li S, Liu Y, Chang X, Li K, Yang D, Zhang X, Yang L, Pu J, Cao G, Tang ST (2019) Two-staged versus three-staged laparoscopic anorectoplasty for patients with rectoprostatic and bladder neck fistulas: a comparative study. J Laparoendosc Adv Surg Tech A 29:1486–1491. https://doi.org/10.1089/lap.2019.0020
Stephens FD, Smith ED, Paoul NW. New York, NY: Liss, 1988
Holschneider A, Hutson J, Peña A et al (2005) Preliminary report on the International Conference for the development of standards for the treatment of anorectal malformations. J Pediatr Surg 40:1521–1526
Koga H, Okazaki T, Yamataka A, Kobayashi H, Yanai T, Lane GJ, Miyano T (2005) Posterior urethral diverticulum after laparoscopic-assisted repair of high-type anorectal malformation in a male patient: surgical treatment and prevention. Pediatr Surg Int 21:58–60. https://doi.org/10.1007/s00383-004-1265-9
Peña A, Amroch D, Baeza C, Csury L, Rodriguez G (1993) The effects of the posterior sagittal approach on rectal function (experimental study). J Pediatr Surg 28:773–778. https://doi.org/10.1016/0022-3468(93)90323-d
Uchida H, Iwanaka T, Kitano Y, Kudou S, Ishimaru T, Yotsumoto K, Gotoh C, Yoshida M (2009) Residual fistula after laparoscopically assisted anorectoplasty: is it a rare problem? J Pediatr Surg 44:278–281. https://doi.org/10.1016/j.jpedsurg.2008.10.056
Rentea RM, Halleran DR, Vilanova-Sanchez A et al (2019) Diagnosis and management of a remnant of the original fistula (ROOF) in males following surgery for anorectal malformations. J Pediatr Surg 54:1988–1992. https://doi.org/10.1016/j.jpedsurg.2019.02.006
Alam S, Lawal TA, Peña A, Sheldon C, Levitt MA (2011) Acquired posterior urethral diverticulum following surgery for anorectal malformations. J Pediatr Surg 46:1231–1235. https://doi.org/10.1016/j.jpedsurg.2011.03.061
Peña A, Hong AR, Midulla P, Levitt M (2003) Reoperative surgery for anorectal anomalies. Semin Pediatr Surg 12:118–123. https://doi.org/10.1016/s1055-8586(02)00022-7
Hong YK, Onal B, Diamond DA, Retik AB, Cendron M, Nguyen HT (2011) Robot-assisted laparoscopic excision of symptomatic retrovesical cysts in boys and young adults. J Urol 186:2372–2378. https://doi.org/10.1016/j.juro.2011.07.113
Takazawa S, Uchida H, Kawashima H, Tanaka Y, Masuko T, Deie K, Amano H, Kobayashi K, Tada M, Iwanaka T (2014) Urethroscopic holmium: YAG laser ablation for acquired posterior urethral diverticulum after repair of anorectal malformations. Pediatr Surg Int 30:945–949. https://doi.org/10.1007/s00383-014-3569-8
Belizon A, Levitt M, Shoshany G, Rodriguez G, Peña A (2005) Rectal prolapse following posterior sagittal anorectoplasty for anorectal malformations. J Pediatr Surg 40:192–196. https://doi.org/10.1016/j.jpedsurg.2004.09.035
Holbrook C, Misra D, Zaparackaite I, Cleeve S (2017) Post-operative strictures in anorectal malformation: trends over 15 years. Pediatr Surg Int 33:869–873. https://doi.org/10.1007/s00383-017-4111-6
Peña A, Hong A (2000) Advances in the management of anorectal malformations. Am J Surg 180:370–376. https://doi.org/10.1016/s0002-9610(00)00491-8
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pathak, M., Saxena, A.K. Postoperative “complications" following laparoscopic-assisted anorectoplasty: A systematic review. Pediatr Surg Int 36, 1299–1307 (2020). https://doi.org/10.1007/s00383-020-04748-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-020-04748-3