Abstract
Purpose
Autologous bio-engineered dermo-epidermal skin substitutes (DESS) represent an alternative therapeutic option for a definitive treatment of skin defects in human patients. Largely, the interaction of host immune cells with transplanted DESS is considered to be essential for the granulation tissue formation, graft take, and its functionality. The aim of this study was to compare the spatiotemporal distribution and density of host-derived monocytes/macrophages and granulocytes in vascularized (vascDESS) versus non-vascularized DESS (non-vascDESS) in a rat model.
Methods
Keratinocytes and the stromal vascular fraction (SVF) were derived from human skin or human adipose tissue, respectively. Human SVF containing both endothelial and mesenchymal/stromal progenitors was used to develop a vascularized collagen type I-based dermal component in vitro. The donor-matched, monolayer-expanded adipose stromal cells lacking endothelial cells were used as a negative control. Subsequently, human keratinocytes were seeded on top of hydrogels to build dermo-epidermal skin grafts. After transplantation onto full-thickness skin wounds on the back of immuno-incompetent rats, grafts were excised and analyzed after 1 and 3 weeks. The expression of distinct inflammatory cell markers specific for host-derived monocytes/macrophages (CD11b, CD68) or granulocytes (HIS48) was analyzed by immunofluorescence microscopy.
Results
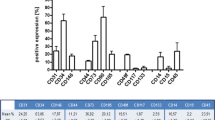
All skin grafts were infiltrated by host-derived monocytes/macrophages (CD11b+, CD68+) and granulocytes (HIS48+) between 1–3 week post-transplantation. When compared to non-vascDESS, the vascDESS showed an increased granulocyte infiltration at all time points analyzed with the majority of cells scattered throughout the whole dermal part. Whereas a moderate number of rat monocytes/macrophages (CD11b+, CD68+) were found in vascDESS at 1 week, only a few cells were detected in non-vascDESS. We observed a time-dependent decrease of monocytes/macrophages in all transplants at 3 weeks.
Conclusions
These results demonstrate a distinct spatiotemporal distribution of monocytes/macrophages as well as granulocytes in our transplants that closely resemble the one observed during physiological wound healing. The differences identified between vascDESS and non-vascDESS may indicate that human endothelial cells lining blood capillaries of vascDESS accelerate infiltration of monocytes and leukocytes.




Similar content being viewed by others
References
Loss M, Wedler V, Kunzi W, Meuli-Simmen C, Meyer VE (2000) Artificial skin, split-thickness autograft and cultured autologous keratinocytes combined to treat a severe burn injury of 93% of TBSA. Burns 26:644–652
Klar AS, Bottcher-Haberzeth S, Biedermann T, Schiestl C, Reichmann E, Meuli M (2014) Analysis of blood and lymph vascularization patterns in tissue-engineered human dermo-epidermal skin analogs of different pigmentation. Pediatr Surg Int 30:223–231
Klar AS, Guven S, Biedermann T, Luginbuhl J, Bottcher-Haberzeth S, Meuli-Simmen C, Meuli M, Martin I, Scherberich A, Reichmann E (2014) Tissue-engineered dermo-epidermal skin grafts prevascularized with adipose-derived cells. Biomaterials 35:5065–5078
Marino D, Luginbuhl J, Scola S, Meuli M, Reichmann E (2014) Bioengineering dermo-epidermal skin grafts with blood and lymphatic capillaries. Sci Transl Med 6:221ra14
Bottcher-Haberzeth S, Klar AS, Biedermann T, Schiestl C, Meuli-Simmen C, Reichmann E, Meuli M (2013) “Trooping the color”: restoring the original donor skin color by addition of melanocytes to bioengineered skin analogs. Pediatr Surg Int 29:239–247
Bottcher-Haberzeth S, Biedermann T, Pontiggia L, Braziulis E, Schiestl C, Hendriks B, Eichhoff OM, Widmer DS, Meuli-Simmen C, Meuli M, Reichmann E (2013) Human eccrine sweat gland cells turn into melanin-uptaking keratinocytes in dermo-epidermal skin substitutes. J Invest Dermatol 133:316–324
Bottcher-Haberzeth S, Biedermann T, Schiestl C, Hartmann-Fritsch F, Schneider J, Reichmann E, Meuli M (2012) Matriderm(R) 1 mm versus Integra(R) Single Layer 1.3 mm for one-step closure of full thickness skin defects: a comparative experimental study in rats. Pediatr Surg Int 28:171–177
Biedermann T, Klar AS, Bottcher-Haberzeth S, Schiestl C, Reichmann E, Meuli M (2014) Tissue-engineered dermo-epidermal skin analogs exhibit de novo formation of a near natural neurovascular link 10 weeks after transplantation. Pediatr Surg Int 30:165–172
Biedermann T, Pontiggia L, Bottcher-Haberzeth S, Tharakan S, Braziulis E, Schiestl C, Meuli M, Reichmann E (2010) Human eccrine sweat gland cells can reconstitute a stratified epidermis. J Invest Dermatol 130:1996–2009
Nishio N, Okawa Y, Sakurai H, Isobe KI (2008) Neutrophil depletion delays wound repair in aged mice. Age 30:11–19
Singer AJ, Clark RA (1999) Cutaneous wound healing. N Engl J Med 341:738–746
Martin P, Leibovich SJ (2005) Inflammatory cells during wound, repair: the good, the bad and the ugly. Trends Cell Biol 15:599–607
Klar AS, Bottcher-Haberzeth S, Biedermann T, Michalak K, Kisiel M, Reichmann E, Meuli M (2014) Differential expression of granulocyte, macrophage, and hypoxia markers during early and late wound healing stages following transplantation of tissue-engineered skin substitutes of human origin. Pediatr Surg Int 30:1257–1264
Gurtner GC, Werner S, Barrandon Y, Longaker MT (2008) Wound repair and regeneration. Nature 453:314–321
Stroncek JD, Reichert WM (2008) Overview of wound healing in different tissue types. In: Reichert WM (ed) Indwelling neural implants: strategies for contending with the in vivo environment. CRC Press, Boca Raton
Anderson JM, Rodriguez A, Chang DT (2008) Foreign body reaction to biomaterials. Semin Immunol 20:86–100
McNally AK, Anderson JM (2011) Macrophage fusion and multinucleated giant cells of inflammation. Adv Exp Med Biol 713:97–111
Acknowledgements
This work was financially supported by the EU-FP6 project EuroSTEC (soft tissue engineering for congenital birth defects in children: contract: LSHB-CT-2006-037409), by the EU-FP7 project EuroSkinGraft (FP7/2007-2013: Grant Agreement Nr 279024), by the EU-FP7 (MultiTERM, Grant Agreement Nr 238551), and the Clinical Research Priority Programs (CRPP) of the Faculty of Medicine of the University of Zurich. We are particularly grateful to the Gaydoul Foundation and the sponsors of “DonaTissue” (Thérèse Meier and Robert Zingg) for their generous financial support and interest in our work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Klar, A.S., Biedermann, T., Simmen-Meuli, C. et al. Comparison of in vivo immune responses following transplantation of vascularized and non-vascularized human dermo-epidermal skin substitutes. Pediatr Surg Int 33, 377–382 (2017). https://doi.org/10.1007/s00383-016-4031-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-016-4031-x