Abstract
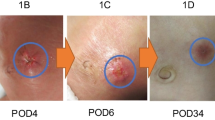
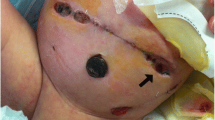
The degree of viscero-abdominal disproportion often makes single-stage reduction difficult in large abdominal wall defects, without risking respiratory or hemodynamic compromise. As a consequence, clinicians have adopted a number of different methods to control these defects. Repair may be in the neonatal period, or later in life. Delayed repairs require epithelialization of the gastroschisis or omphalocele. Definitive repair may be in single or multiple stages. This paper describes four children in whom negative pressure wound therapy (NPWT) was used to facilitate closure of these complex defects.


Similar content being viewed by others
References
Levy S, Tsao K, Cox CS Jr, Phatak UR, Lally KP, Andrassy RJ (2013) Component separation for complex congenital abdominal wall defects: not just for adults anymore. J Pediatr Surg 48(12):2525–2529. doi:10.1016/j.jpedsurg.2013.05.067
van Eijck FC, Aronson DA, Hoogeveen YL, Wijnen RM (2011) Past and current surgical treatment of giant omphalocele: outcome of a questionnaire sent to authors. J Pediatr Surg 46(3):482–488. doi:10.1016/j.jpedsurg.2010.08.050
Foroutan H, Jenabali Jahromi B, Dastgheyb N, Najafi S (2013) A new method of repairing giant omphaloceles with bilateral mesh grafts lateral to the rectus abdominis muscles. Ann Colorectal Res 1(1):32–36. doi:10.5812/acr.11475
Choi WW, McBride CA, Kimble RM (2011) Negative pressure wound therapy in the management of neonates with complex gastroschisis. Pediatr Surg Int 27(8):907–911. doi:10.1007/s00383-011-2868-6
Morris MW Jr, Westmoreland T, Sawaya DE, Blewett CJ (2013) Staged closure with negative pressure wound therapy for gastroschisis with liver herniation: a case report. J Pediatr Surg 48(5):E13–15. doi:10.1016/j.jpedsurg.2013.03.005
Krug E, Berg L, Lee C, Hudson D, Birke-Sorensen H, Depoorter M, Dunn R, Jeffery S, Duteille F, Bruhin A, Caravaggi C, Chariker M, Dowsett C, Ferreira F, Martinez JM, Grudzien G, Ichioka S, Ingemansson R, Malmsjo M, Rome P, Vig S, Runkel N, Martin R, Smith J (2011) Evidence-based recommendations for the use of negative pressure wound therapy in traumatic wounds and reconstructive surgery: steps towards an international consensus. Injury 42(Suppl 1):S1–12. doi:10.1016/S0020-1383(11)00041-6
Davies MW, Kimble RM, Woodgate PG (2002) Ward reduction without general anaesthesia versus reduction and repair under general anaesthesia for gastroschisis in newborn infants. Cochrane Database Syst Rev 3:CD003671. doi:10.1002/14651858.CD003671
Sakata S, Das GR, Leditschke JF, Kimble RM (2009) Extensive necrotising fasciitis in a 4-day-old neonate: a successful outcome from modern dressings, intensive care and early surgical intervention. Pediatr Surg Int 25(1):117–119. doi:10.1007/s00383-008-2289-3
Leppaniemi A, Tukiainen E (2013) Reconstruction of complex abdominal wall defects. Scand J Surg 102(1):14–19
Kilbride KE, Cooney DR, Custer MD (2006) Vacuum-assisted closure: a new method for treating patients with giant omphalocele. J Pediatr Surg 41(1):212–215. doi:10.1016/j.jpedsurg.2005.10.003
Adetayo OA, Aka AA, Ray AO (2012) The use of intra-abdominal tissue expansion for the management of giant omphaloceles: review of literature and a case report. Ann Plast Surg 69(1):104–108. doi:10.1097/SAP.0b013e31822128f5
Kaabachi O, Berg A, Laguenie G, Adamsbaum C, Bargy F, Helardot PG (1998) Budd–Chiari syndrome following repair of a giant omphalocele. Eur J Pediatr Surg 8(6):371–372. doi:10.1055/s-2008-1071236
Conflict of interest
The authors declare that they have no conflict of interest. No funding was sought or granted in the conduct of this study.
Ethical standard
This project has prior approval from the Children’s Health Services Queensland Human Research Ethics Committee and has therefore been conducted in concordance with the principles of the Declaration of Helsinki. Consent has been obtained from parents for inclusion of their children’s stories and images within this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
McBride, C.A., Stockton, K., Storey, K. et al. Negative pressure wound therapy facilitates closure of large congenital abdominal wall defects. Pediatr Surg Int 30, 1163–1168 (2014). https://doi.org/10.1007/s00383-014-3545-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-014-3545-3