Abstract
The high mortality in patients with congenital diaphragmatic hernia (CDH) has been attributed to pulmonary hypoplasia and persistent pulmonary hypertension (PPH). Endothelin-1 (ET-1), nitric oxide (NO), and calcitonin gene-related peptide (CGRP) have been reported to be important vasoactive mediators in the perinatal pulmonary circulation. The exact mechanism by which these vasoactive mediators interact to regulate the perinatal pulmonary vascular tone in CDH with PPH is not fully understood. We hypothesized that the altered pulmonary vascular reactivity in CDH is due to imbalance in vasoactive mediators. This study was designed to investigate mRNA expression of ET-1, eNOS, and CGRP in CDH lung in the perinatal period. A CDH model was induced in pregnant rats following administration of nitrofen. In control animals, the same dose of olive oil was given without nitrofen. Cesarean section was performed on day 21 of gestation. The newborn rats were intubated and ventilated, and ventilation was continued for 1–6 h. Left lungs were collected from both groups at 0, 1, and 6 h after ventilation (n=8 in each group). Reverse transcriptase-polymerase chain reaction on lung tissue was performed to evaluate the relative level of ET-1, eNOS, and CGRP mRNA expression. The results showed a significant increase in ET-1 mRNA in CDH lung at 1 and 6 h after ventilation compared with controls. In CDH lung, eNOS mRNA and CGRP mRNA levels were significantly increased at 1 h but were similar to control values at 6 h after ventilation. The increased expression of vasoconstrictor ET-1 mRNA and vasodilators eNOS mRNA and CGRP mRNA in the CDH lung at 1 h after ventilation suggests that pulmonary vascular tone is rapidly changing after birth. An imbalance in the production of vasoconstrictors and vasodilators by the CDH lung may contribute to high pulmonary vascular resistance.
Similar content being viewed by others
Introduction
The mortality rate for newborn infants with congenital diaphragmatic hernia (CDH) is still high despite significant advances in neonatal resuscitation and intensive care [1]. Hypoplastic lung and persistent pulmonary hypertension (PPH) are the principle causes of the high morbidity and mortality in infants with CDH. PPH in the newborn is characterized by elevated pulmonary vascular resistance resulting in right-to-left shunting across the foramen ovale and ductus arteriosus with severe hypoxemia. Studies in experimental models of PPH have suggested that high pulmonary vascular resistance is partly due to structural changes in the pulmonary vasculature and to an imbalance in responsiveness to vasodilator and vasoconstrictor stimuli [2–6].
Several vasoactive mediators have been implicated in the development of pulmonary hypertension in nitrofen-induced CDH models [7–9]. Endothelin-1 (ET-1), which is produced by vascular endothelial cells and some leukocytes, is a potent vasoconstrictor and mitogen for vascular smooth muscle cells [10–14]. Increased ET-1 levels have been noted in and postulated to contribute to the pathophysiology of pulmonary disease, including primary pulmonary hypertension, asthma, and inflammatory lung disease [15–17]. Nitric oxide (NO) is a major vasodilator of the cardiovascular system. NO is synthesized from arginine by NO synthases (NOS). The endothelial constitutive NOS (eNOS) is the major NOS isoform expressed in the cardiovascular system. eNOS expression occurs mainly in vascular endothelium and plays an important role in regulating vascular tone [18, 19]. Calcitonin gene-related peptide (CGRP), an active product of pulmonary endocrine cells, is also a pulmonary vasodilator [20]. A recent study from our laboratory demonstrated increased CGRP mRNA and immunoreactivity in CDH lung in rats [7].
The exact mechanism by which these vasoactive mediators interact to regulate perinatal pulmonary vascular tone in CDH with PPH is not fully understood. We hypothesized that the altered pulmonary vascular reactivity in CDH is due to an imbalance in vasoactive mediators. We therefore designed the present study to examine mRNA expression of ET-1, eNOS, and CGRP in the CDH lung compared with the normal lung under ventilation in the perinatal period.
Materials and methods
Creation of CDH
Adult Sprague-Dawley rats were bred after overnight controlled matings. Observation of positive smears was considered proof of pregnancy; the day of observation was determined day 0. Water and food were supplied ad libitum. At day 9.5 of pregnancy (term=22 days), 100 mg nitrofen (WAKO Chemical, Osaka, Japan) dissolved in olive oil was given as a single dose via a stomach tube under short anesthesia. In control animals, the same dose of olive oil was given without nitrofen. Cesarean section was performed on day 21 of gestation.
Groups
Eight newborn rats in both control and CDH groups were sacrificed immediately after birth. These rats formed the no-ventilation group. Sixteen newborn rats in both control and CDH groups were intubated and ventilated. Eight each from the normal and CDH groups were the 1-h ventilation group, and eight each from the normal and CDH groups made up the 6-h ventilation group.
Intubation and ventilation
A transverse cervical incision was made, and the endotracheal cannula (24-g Teflon catheter) was passed down the trachea, keeping the circulation via the umbilical cord from the placenta. The endotracheal cannula was confirmed to be in the trachea after visualizing through the cervical incision. After ligation of the umbilical cord, the intubated animals were immediately transferred to a warm plate heated to 30°C, and the endotracheal tube was connected to a modified pressure-cycled ventilator (Siemens servo ventilator 900C). The ventilator settings were as follows: FiO2 1.0, frequency 60/min, I:E ratio 1:2, inspiratory peak pressure 12 cm H2O, PEEP 0 cm H2O. After confirmation that the movement of the lungs in the newborn rat was satisfactory, ventilation was continued for 1 or 6 h. The oxygenation of ventilated animals was confirmed by movement of the lungs and color of the skin. The animals were euthanized after ventilation. Diaphragmatic hernia was confirmed in the CDH group by thoracotomy. The left lung was dissected from the CDH and control groups.
The research project had been approved by the Department of Health, Ministry of Health, Ireland.
mRNA isolation
Left lungs (n=8 in each group) dissected microsurgically from the thoracic cavity were immediately snap-frozen and kept in a deep freezer (−70°C) until RNA extraction. Total RNA was extracted from each lung by using a commercially supplied solution, TRIZOL reagent (Life Technologies, Paisley, UK), according to recommended protocol. mRNA was isolated using streptavidin magnetic particles and biotin-labeled oligo (dT)20 probe (Boehringer Mannheim, Mannheim, Germany).
Reverse transcriptase-polymerase chain reaction
We have previously described the polymerase chain reaction (PCR) method [21, 22]; 0.2 μg of mRNA was applied to cDNA synthesis according to the recommended protocol (SuperScript Preamplification System for First Strand cDNA Synthesis, Life Technologies), which used random primers and 200 units of SuperScript II RNases H-reverse transcriptase in 20 μl of reaction volume. Positive controls for each specimen consisted of the constantly expressed housekeeping gene, β-actin. Negative controls consisted of reaction mixtures without reverse transcriptase for each specimen. The specific primer sets used in this study and the estimated size of the PCR products are listed in Table 1. The PCR mixture (total 50 μl) contained 20 pmol of each primer, 200 μM of each deoxyribonucleotide triphosphate, 5 μl of 10× PCR buffer, 2 units of AmpliTaq DNA polymerase (Perkin-Elmer, Norwalk, CT, USA), and 2 μl of cDNA solution. PCR for ET-1 (94°C 1 min, 57°C 1 min, 72°C 1 min, 38 cycles), eNOS (94°C 1 min, 60°C 1 min, 72°C 1 min, 30 cycles), CGRP (94°C 1 min, 60°C 1 min, 72°C 1 min, 35 cycles), and β-actin (94°C 40 s, 68°C 40 s, 72°C 90 s, 26 cycles) was performed in each case. These PCR conditions were confirmed to be within the exponential phase. The PCR products were electrophoresed on a 1.5% agarose gel and stained with ethidium bromide to visualize DNA bands. Semiquantitative analysis of the PCR products was similar to the methods described previously [23, 24]. The intensities of each band were analyzed using GDS 8000 Gel Documentation Systems (UVP, Upland, CA, USA). The images of each band were scanned over ultraviolet light at the same condition for all gels. Intensities of each band were measured using gel analysis software, Gelworks ID (UVP), for quantitation. Relative levels of ET-1, eNOS, and CGRP mRNA for each case were expressed as a ratio of the band intensity divided by that of β-actin.
Statistics
Results were expressed as mean ± SD. Data were analyzed by analysis of variance (ANOVA). The statistical significance between groups was determined by Fisher’s PLSD test. Statview software (Abacus Concepts, Barkeley, CA, USA) was used for all statistical work. A p-value of less than 0.05 was taken as significant.
Results
The PCR conditions described above successfully yielded the amplified fragments of expected size for ET-1 (499 bp), eNOS (432 bp), CGRP (365 bp), and β-actin (838 bp) in each sample (Fig. 1). Intensities of the bands corresponding to β-actin mRNA were similar among all the samples. No amplified products were observed in the gel lanes where reverse transcriptase was omitted.
Endothelin-1, eNOS, CGRP, and β-actin mRNA expression in a representing sample in each case. Fragments of expected size for ET-1 (499 bp), eNOS (432 bp), CGRP (365 bp), and β-actin (838 bp) were successfully amplified. Intensities of the bands corresponding to β-actin mRNA were similar among the samples.
Relative levels of ET-1 mRNA continued to increase during ventilation both in CDH lung and controls (Table 2, Fig. 2). Relative levels of ET-1 mRNA were significantly increased in CDH lung compared with controls at birth and 1 and 6 h after ventilation, suggesting the presence of high levels of ET-1 in CDH lung (Table 2, Fig. 2).
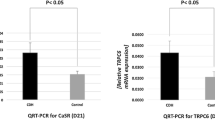
Relative levels of eNOS mRNA were significantly higher in CDH lung compared with controls at 1 h after ventilation (Table 2, Fig. 3). However, relative levels of eNOS mRNA in CDH lung after 6 h of ventilation were similar to controls (Table 2, Fig. 3).
Relative levels of CGRP mRNA were significantly increased in CDH lung compared with controls at birth and at 1 h after ventilation (Table 2, Fig. 4). Relative levels of CGRP mRNA after 6 h of ventilation were similar in CDH lung and controls (Table 2, Fig. 4).
Discussion
Immediately after birth, the pulmonary vasculature is rapidly remodeled to effect an abrupt reduction in pulmonary vascular resistance. In cases with CDH complicated by PPH, the pulmonary arteries fail to remodel after birth, and the vessels remain thick-walled. The pathogenesis of PPH is not clearly understood. Several vasoactive mediators have recently been suggested as playing a role in the pathogenesis of PPH [7–9, 20]. Little is known about local synthesis of vasoactive mediators in the CDH lung in the early postnatal period. In the present study, there was a significant increase in ET-1 mRNA, eNOS mRNA, and CGRP mRNA expression in the nitrofen-induced CDH lung 1 h after birth during ventilation. This upregulated synthesis of both vasoconstrictor ET-1 and vasodilators eNOS and CGRP in the CDH lung at 1 h after birth suggests that several vasoactive mediators are involved in regulating pulmonary vascular tone immediately after birth.
Studies in experimental models of PPH have suggested that high pulmonary vascular resistance is partly due to structural changes in the pulmonary vasculature and to an imbalance in production or responsiveness to vasodilator and vasoconstrictor stimuli [2–6]. In the present study, ET-1 mRNA expression in the CDH lung continued to increase after birth, and ET-1 mRNA levels were significantly higher at 6 h compared with 1 h after birth. However, the mNRA expression of both vasodilators eNOS and CGRP in CDH lung were significantly decreased at 6 h after birth compared with 1 h after birth. It is tempting to speculate that the imbalance in vasoconstrictor (ET-1) and vasodilator (NO and CGRP) synthesis in the hypoplastic CDH lung in the early postnatal period results in the failure of the vasculature to remodel. Upregulated synthesis of vasoconstrictors and downregulated synthesis of vasodilators, as seen in this animal model, may accelerate high pulmonary vascular resistance.
It is now quite clear from the clinical and experimental observations that the development of pulmonary hypertension is an important factor in the poor prognosis of CDH [1]. Various clinical trials have shown that the response to a variety of vasoactive agents, including inhaled NO, is highly unpredictable [25]. In many instances these vasoactive agents were given too late, coinciding with the clinical episodes of deterioration in CDH babies. Our experimental study clearly shows that the first hour after birth is the most critical time, during which rapid alterations in vasoconstrictors and vasodilators are occurring. Intervention at this stage may prevent the development of structural changes in the pulmonary vasculature and, thus, the progression to PPH.
References
Puri P (1994) Congenital diaphragmatic hernia. Curr Prob Surg 31:785–859
Abman SH, Shanley PF, Accurso FJ (1989) Failure of postnatal adaptation of the pulmonary circulation after chronic intrauterine pulmonary hypertension in fetal lambs. J Clin Invest 83:1849–1858
Morin FC (1989) Ligating the ductus arteriosus before birth causes persistent pulmonary hypertension in the newborn lamb. Pediatr Res 25:245–250
Murphy JD, Rabinovitch M, Goldstein JD, Reid LM (1981) The structural basis of persistent pulmonary hypertension of the newborn infant. J Pediatr 98:962–967
Belik J, Halayko AJ, Rao K, Stephens NL (1993) Fetal ductus arteriosus ligation. Pulmonary vascular smooth muscle biochemical changes. Cric Res 72:588–596
McQueston JA, Kinsella JP, Ivy DD, McMurtry IF, Abnam SH (1995) Chronic pulmonary hypertension in utero impairs endothelin-dependent vasodolation. Am J Physiol 268:H288–H294
Yamataka T, Puri P (1996) Increased intracellular levels of calcitonin gene-related peptide-like immunoreactivity in pulmonary endocrine cells in an experimental model of congenital diaphragmatic hernia. Pediatr Surg Int 11:448–452
Okazaki T, Sharma HS, McCune SK, Tibboel D (1998) Pulmonary vascular balance in congenital diaphragmatic hernia: enhanced endothelin-1 gene expression as a possible cause of pulmonary vasoconstriction. J Pediatr Surg 33:81–84
North AJ, Moya FR, Mysore MR, Thomas VL, Wells LB, Wu LC, Shaul PW (1995) Pulmonary endothelial nitric oxide synthase gene expression is decreased in a rat model of congenital diaphragmatic hernia. Am J Respir Cell Molk Biol 13:676–682
Sessa WC, Kaw S, Hecker M, Vane JR (1991) The biosynthesis of endothelin-1 by human polymorphonuclear leukocytes. Biochem Biophys Res Commun 174:613–618
Yanagisawa M, Kurihara H, Kimura, Goto K, Masaki T (1988) A novel potent vasoconstrictor peptide produced by vascular endothelial cells. Nature 332:411–415
Ohlstein EH, Arleth A, Ezekiel M (1990) Biosynthesis and modulation of endothelin from bovine pulmonary arterial endothelial cells. Life Sci 46:181–188
Ehrenreich H, Anderson RW, Fox CH, Rieckmann P, Hoffman GS, Travis WD, Coligan JE, Kehrl JH, Fauci AS (1990) Endothelins, peptides with potent vasoactive properties, are produced by human macrophages. J Exp Med 172:1741–1748
Cale AR, Ricagna F, Wiklund L, McGregor CG, Miller VM (1994) Mononuclear cells from dogs with acute lung allograft rejection cause contraction of pulmonary arteries. Circulation 90:952–958
Giaid A, Michel RP, Stewart DJ, Corrin B, Hamid Q (1993) Expression of endothelin-1 in the lungs of patients with cryptogenic fibrosing alveolitis. Lancet 341:1550–1554
Giaid A, Yanagisawa M, Langleben D, Michel RP, Levy R, Shennib H, Kimura S, Makasi T, Duguid WP, Stewart DJ (1993) Expression of endothelin-1 in the lungs of patients with pulmonary hypertension. N Engl J Med 328:1732–1739
Vittori E, Marini M, Fasoli F, DeFranchis R, Mattoli S (1992) Decreased expression of endothelin in bronchial epithelial cells of asthmatic patients and effects of corticosteroids. Am Rev Respir Dis 146:1320–1325
Vallance P, Collier J (1994) Fortnightly review biology and clinical relevance of nitric oxide. BMJ 309:453–457
Mungrue IN, Bredt DS, Stewart DJ, Husain M (2003) From molecules to mammals: what’s NOS got to do with it? Acta Physiol Scand 179:123–135
Brain SD, Williams TJ, Tippins JR, Morris HR, MacIntyre I (1985) Calcitonin gene-related peptide is a potent vasodilator. Nature 313:54–56
Taira Y, Oue T, Shima H, Miyazaki E, Puri P (1998) Increased and procollagen expression in the lung of nitrofen induced diaphragmatic hernia in rats. J Pediatr Surg 34:715–719
Oue T, Taira Y, Shima H, Miyazaki E, Puri P (1998) Insulin-like growth factor I and II levels in hypoplastic lung in nitrofen induced diaphragmatic hernia in rats. Pediatr Surg Int 15:175–179
Nakayama H, Yokoi H, Fujita J (1992) Quantification of mRNA by non-radioactive RT-PCR and CCD imaging system. Nucl Acids Res 20:4939
Kaneto H, Morrissey J, McCracken R (1994) Enalapril reduces collagen type IV synthesis and expression of the interstitium in the obstructed rat kidney. Kidney Int 45:1637–1647
Roberts JD, Fineman JR, Morin FC 3rd, Shaul PW, Rimar S, Schreiber MD, Polin RA, Zwass MS, Zayek MM, Gross I, Heymann MA, Zapol WM (1997) Inhaled nitric oxide and persistent pulmonary hypertension of the newborn. N Engl J Med 336:605–610
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shinkai, T., Shima, H., Solari, V. et al. Expression of vasoactive mediators during mechanical ventilation in nitrofen-induced diaphragmatic hernia in rats. Ped Surgery Int 21, 143–147 (2005). https://doi.org/10.1007/s00383-004-1310-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-004-1310-8