Abstract
Introduction
The inflammatory myofibroblastic tumor (IMT) is a very rare lesion with an incidence of less than 0.1% of total neoplasms and with main affection in the lungs. Involvement in the central nervous system is extremely rare, but with a much more aggressive course than IMT diagnosed in the rest of the body. We report the 2 cases presented in our neurosurgery department to date; both were treated satisfactorily without intercurrences in 10 years of follow-up.
Historical background
The World Health Organization described the IMT as a distinctive lesion composed of myofibroblastic spindle cells accompanied by an inflammatory infiltrate of plasma cells, lymphocytes, and eosinophils.
Clinical presentation
Clinical manifestations of patients with CNS IMT vary and may consist of headache, vomiting, seizures, and blindness. Seizures are the most common symptom in patients with focal lesions.
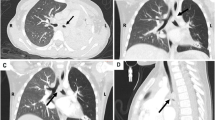
Diagnosis
The true origin of this entity remains to be elucidated, but to date, etiologies ranging from chromosomal alterations to autoimmune or postinfectious mechanisms have been described. Due to its rarity and non-specificity in imaging, the final diagnosis of IMT in the brain parenchyma relies on pathological examination.
Management
Treatment options are controversial and include total or subtotal removal, high-dose steroids, and radiation therapy. In the last decade, the development of ALK Tyrosine Kinase Inhibitors allows the possibility of chemotherapy in those patients harboring ALK mutations.
Conclusion
IMT is a rare tumor that can exceptionally be found in the CNS. The cause is still unknown although the different studies focus on a neoplastic origin. The diagnosis is based in the use of different modalities of imaging and with histological confirmation. Optimal management is gross total resection whenever possible, is the only established curative treatment. Further research with longer follow-up is needed to clarify the natural history of this rare tumor.






Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available due to the sensitive nature of the information and because the participants are underage but are available from the corresponding author on reasonable request.
Code availability
Not applicable.
References
Ma L, Wang K, Liu W-K, Zhang Y-k (2009) Is radical surgery necessary to head and neck inflammatory myofibroblastic tumor (IMT) in children? Childs Nerv Syst 25:285–291
Dalton B, Thomas P, Sharp N, Manalang M, Fisher J, Moir C, St Peter S, Iqbal C (2016) Inflammatory myofibroblastic tumors in children. J Pediatr Surg 51:541–544
Sakurai H, Hasegawa T, Watanabe Si et al (2004) Inflammatory myofibroblastic tumor of the lung. Eur J Cardiothorac Surg 25(2):155–9
Pettinato G, Manivel JC, De rosa N, Dehner LP (1990) Inflammatory myofibroblastic tumor (plasma cell granuloma): clinicopathologic study of 20 cases with immunohistochemical and ultrastructural observations. Am J Clin Pathol 94(5):538–546
Coffin CM, Fletcher JA (2002) Inflammatory myofibroblastic tumor. In: Fletcher CD, Unni KK, Mertens F (eds) World Health Organization classification of tumours. Pathology and genetics of tumours of soft tissue and bone. IARC Lyon pp. 91–93
Cannella DM, Prezyna AP, Kapp JP (1988) Primary intracranial plasma-cell granuloma. Case report J Neurosurg 69:785–788
Meis JM, Enzinger FM (1991) Inflammatory fibrosarcoma of the mesentery and retroperitoneum. A tumor closely simulating inflammatory pseudotumor. Am J Surg Pathol 15:1146–1156
Pimentel J, Costa A, Távora L (1993) Inflammatory pseudotumor of the choroid plexus. Case report J Neurosurg 79:939–942
Tang TT, Segura AD, Oechler HW, Harb JM, Adair SE, Gregg DC, Camitta BM, Franciosi RA (1990) Inflammatory myofibrohistiocytic proliferation simulating sarcoma in children. Cancer 65(7):1626–1634
Galindo J, Lassaletta L, Garcia E, Gavilan J, Allona M, Royo A, Patrón M (2008) Spontaneous hearing improvement in a patient with an inflammatory myofibroblastic tumor of the temporal bone. Skull Base (6):411–15
Jehangir M, Jang Ur A, Rehman I et al (April 20 2017) Synchronous inflammatory myofibroblastic tumor in lung and brain: a case report and review of literature. Cureus 9(4):e1183
Kato K, Moteki Y, Nakagawa M, Kadoyama S, Ujiie H (2011) Inflammatory myofibroblastic tumor of the cerebellar hemisphere. Neurol Med Chir 51(1):79–81
Lamant L, Meggetto F, Al Saati T, Brugieres L, de Paillerets BB, Dastugue N, Bernheim A, Rubie H, Terrier-Lacombe MJ, Robert A et al (1996) High incidence of the t(2;5)(p23;q35) translocation in anaplastic large cell lymphoma and its lack of detection in Hodgkin’s disease. Comparison of cytogenetic analysis, reverse transcriptase-polymerase chain reaction, and P-80 immunostaining. Blood 87:84–291
Morris SW, Kirstein MN, Valentine MB, Dittmer KG, Shapiro DN, Saltman DL, Look AT (1994) Fusion of a kinase gene, ALK, to a nucleolar protein gene, NPM, in non-Hodgkin’s lymphoma. Science 263(5151):1281–1284
Iwahara T, Fujimoto J, Wen D, Cupples R, Bucay N, Arakawa T, Mori S, Ratzkin B, Yamamoto T (1997) Molecular characterization of ALK, a receptor tyrosine kinase expressed specifically in the nervous system. Oncogene 14:439–449
Dirks WG, Fahnrich S, Lis Y, Becker E, MacLeod RA, Drexler HG (2002) Expression and functional analysis of the anaplastic lymphoma kinase (ALK) gene in tumor cell lines. Int J Cancer 100:49–56
Lawrence B, Perez-Atayde A, Hibbard MK, Rubin BP, Dal Cin P, Pinkus JL, Fletcher JA (2000) TPM3-ALK and TPM4-ALK oncogenes in inflammatory myofibroblastic tumors. Am J Pathol 157(2):377–84
Ono A, Murakami H, Serizawa M et al (2016) Drastic initial response and subsequent response to two ALK inhibitors in a patient with a highly aggressive ALK-rearranged inflammatory myofibroblastic tumor arising in the pleural cavity. Lung Cancer 99:151–154
Hallberg B, Palmer RH (2013) Mechanistic insight into ALK receptor tyrosine kinase in human cancer biology. Nat Rev Cancer 13(10):685–700
Coffin CM, Hornick JL, Fletcher CD (2007) Inflammatory myofibroblastic tumor: comparison of clinicopathologic, histologic, and immunohistochemical features including ALK expression in atypical and aggressive cases. Am J Surg Pathol 31:509–520
Arber DA, Kamel OW, van de Rijn M, Davis RE, Medeiros LJ, Jaffe ES, Weiss LM (1995) Frequent presence of the Epstein-Barr virus in inflammatory pseudotumor. Hum Pathol 26(10):1093–1098
Khatri A, Agrawal A, Sikachi R, Mehta D, Sahni S, Meema N (2018) Inflammatory myofiboblastic tumor of the lung. Adv Respir Med 2018(86):27–35
Schweckendiek D, Inci I, Schneiter D et al (2015) Inflammatory myofibroblastic tumor of the lung: two progressing pulmonary nodules in a 25-year-old adult with a moraxella catharalis infection. Ann Thorac Surg 100(6):e123–e124
Polo MF, Mastrandrea S, Santoru L et al (2015) Pulmonary inflammatory pseudotumor due to Coxiella burnetii. Case report and literature review. Microbes Infect 17(11–12):795–798
Evans J, Chan C, Gluch L et al (1999) Inflammatory pseudotumour secondary to actinomyces infection. Aust N Z J Surg 69(6):467–469
Park SH, Choe GY, Kim CW et al (1990) Inflammatory pseudotumor of the lung in a child with mycoplasma pneumonia. J Korean Med Sci 5(4):213–223
Mergan F, Jaubert F, Sauvat F et al (2005) Inflammatory myofibroblastic tumor in children: clinical review with anaplastic lymphoma kinase, Epstein-Barr virus, and human herpesvirus 8 detection analysis. J Pediatr Surg 40(10):1581–1586
Shlopov BV, French SW (2011) Inflammatory myofibroblastic tumor of the lung with unique histological pattern and association with Sjögren’s disease and systemic lupus erythematosus. Exp Mol Pathol 91(2):509–514
Chang Y, Horoupian DS, Lane B et al (1991) Inflammatory pseudotumor of the choroid plexus in Sjögren’s disease. Neurosurgery 29(2):287–290
Hosokawa A, Takahashi H, Akaike J, Okuda H, Murakami R, Kawahito Y, Tokuno T, Makiguchi Y, Sakamoto H, Hinoda Y, Imai K (1998) A case of Sjögren’s syndrome associated with inflammatory pseudotumor of the liver. Nihon Rinsho Meneki Gakkai Kaishi 21(5):226–33 Japanese
Eckstein RP, Hollings RM, Martin PA et al (1995) Pancreatic pseudotumor arising in association with Sjögren’s syndrome. Pathology 27(3):284–288
Zen Y, Kitagawa S, Minato H et al (2005) IgG4-positive plasma cells in inflammatory pseudotumor (plasma cell granuloma) of the lung. Hum Pathol 36:710–717
Bhagat P, Bal A, Das A, Singh N, Singh H (2013) Pulmonary inflammatory myofibroblastic tumor and IgG4-related inflammatory pseudotumor: a diagnostic dilemma. Virchows Arch 463:743–747
Zhu L, Li J, Liu C, Ding W, Lin F, Guo C, Liu L (2017) Pulmonary inflammatory myofibroblastic tumor versus IgG4- related inflammatory pseudotumor: differential diagnosis based on a case series. J Thorac Dis 9(3):598–609
Kamisawa T, Funata N, Hayashi Y et al (2003) A new clinicopathological entity of IgG4-related autoimmune disease. J Gastroenterol 38:982–984
Zhang Z, Fu W, Wang M, Niu L, Liu B, Jiao Y, Liu X. IgG4-related inflammatory pseudotumor of the brain parenchyma: a case report and literature review. Acta Neurol Belg 118(4):617–627
Regev K, Nussbaum T, Cagnano E, Giladi N, Karni A (2014) Central nervous system manifestation of IgG4-related disease. JAMA Neurol 71(6):767
Joshi D, Jager R, Hurel S, Pereira SP, Johnson GJ, Chapman M, Fowler R, Winstanley A, Losseff N (2015) Webster GJ (2015) Cerebral involvement in IgG4-related disease. Clin Med (Lond) 15(2):130–134
Okazaki K, Umehara H (2017) Current concept of IgG4-related disease. Curr Top Microbiol Immunol 401:1–17
Agrons GA, Rosado-de-Christenson ML, Kirejczyk WM et al (1998) Pulmonary inflammatory pseudotumor: radiologic features. Radiology 206(2):511–518
Karapolat S, Seyis KN, Ersoz S et al (2017) Lung image: inflammatory myofibroblastic tumor. Lung 195(3):387–388
Narla LD, Newman B, Spottswood SS et al (2003) Inflammatory pseudotumor. Radiographics 23(3):719–729
Häusler M, Schaade L, Ramaekers VT, Doenges M, Heimann G, Sellhaus B (2003) Inflammatory pseudotumors of the central nervous system: report of 3 cases and a literature review. Hum Pathol 34(3):253–62
Whitehead M, Grimm J, Nelson M (2012) Inflammatory myofibroblastic tumor. Radiology 264:912–916
Aubry A, Galiacy S, Allouche M (2019) Targeting ALK in cancer: therapeutic potential of proapoptotic peptides. Cancers 11:275
Jacob SV, Reith JD, Kojima AY, Williams WD, Liu C, Vila DL (2014) An unusual case of systemic inflammatory myofibroblastic tumor with successful treatment with ALK-inhibitor. Case Rep Pathol 2014:470340
Butrynski JE, D’Adamo DR, Hornick JL et al (2010) Crizotinib in ALK-rearranged inflammatory myofibroblastic tumor. N Engl J Med 363:1727–1733
Ogata M, Hatachi Y, Ogata T, Satake H, Imai Y, Yasui H (2019) Effectiveness of crizotinib for inflammatory myofibroblastic tumor with ALK mutation. Intern Med 58:1029–1032
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. The bibliographic research, summary of the case, and edition of images were carried out by Adalberto Ochoa and Santiago Cicutti. The first draft of the manuscript was made by Javier Gonzalez Ramos and the rest of the authors commented and made contributions to it. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Hospital de Pediatría Juan P. Garrahan.
Consent to participate
Informed consent was obtained from the patient in this study.
Consent for publication
Patient signed informed consent regarding publishing their data and photographs.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ramos, J.G., Ochoa, A., Cicutti, S. et al. Inflammatory myofibroblastic tumor of the lung involving the central nervous system in pediatric patients. Childs Nerv Syst 39, 1137–1145 (2023). https://doi.org/10.1007/s00381-023-05925-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-023-05925-0