Abstract
Introduction
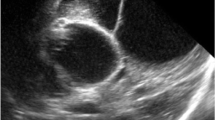
Pyogenic ventriculitis is a severe infection of the central nervous system with serious and often irreversible consequences in the quality of life of patients. Its treatment is difficult due to the impossibility of achieving sterility of cerebrospinal fluid (CSF) and the physiological characteristics promptly. Several treatment options have been described, from prolonged antibiotic treatments to placement of ventricular drains with continuous irrigation and puncture reservoirs. We propose an aggressive and minimally invasive treatment with neuroendoscopic lavage (NEL).
Methods
Retrospective and descriptive study. We analyzed the NEL performed in our hospital for pyogenic ventriculitis between 2011 and 2020. A total of 16 patients were found; 2 of them lost follow-up, so they were not included. All patients had a diagnosis of pyogenic ventriculitis, either due to the macroscopic characteristics of the CSF or due to imaging criteria. Between 1 and 3 NEL were performed per patient until obtaining sterility and normalization of protein and cell counts of CSF.
Results
The average age was 38 months (2 months to 16 years). Ten patients were female and 4 were male. Sixty-four percent of germs in cultures corresponded to gram-negative and polymicrobial flora. The average number of days until the first sterile CSF post-NEL was 3.8 days (0 to 10 days). The NEL produced a significant improvement in the characteristics of the CSF compared to the pre-NEL. The mean pre-NEL of CSF protein levels was 907 mg/dl (123–4510 mg/dl) compared with the post-NEL of 292 mg/dl (38–892 mg/dl) with a p-value = 0.0076. Regarding cellularity, statistically significant results were also achieved (p-value = 0.0011) with a pre-surgical cellularity of 665 elements/mm3 (4–3090 elements/mm3) compared with 57 elements/mm3 (0–390 elements/mm3) post-NEL.
Of the patients, 85.7% had a shunt prior to the onset of ventriculitis and the average number of days until the new shunt was 36.56 days (17–79 days), with a total hospitalization days ranging from 22 to 170.
Conclusions
NEL allows rapid sterilization of CSF, decreasing the deleterious effect of infection in the CNS more rapidly compared to other types of conventional treatment.



Similar content being viewed by others
Data availability
Not applicable.
Code availability
Not applicable.
References
Inamasu J, Kuramae T, Tomiyasu K, Nakatsukasa M (2011) Fulminant ependymitis following intraventricular rupture of brain abscess. J Infect Chemother 17:534–537. https://doi.org/10.1007/s10156-010-0201-2
Carter JA, Neville BGR, Newton CRJC (2003) Neuro-cognitive impairment following acquired central nervous system infections in childhood: a systematic review. Brain Res Rev 43:57–69. https://doi.org/10.1016/S0165-0173(03)00192-9
Kanik A, Sirin S, Kose E et al (2015) Clinical and economic results of ventriculoperitoneal shunt infections in children. Turk Neurosurg 25:58–62. https://doi.org/10.5137/1019-5149.JTN.8540-13.2
Humphreys H, Jenks PJ (2015) Surveillance and management of ventriculitis following neurosurgery. J Hosp Infect 89:281–286
Tunkel AR, Hasbun R, Bhimraj A et al (2017) 2017 Infectious Diseases Society of America’s clinical practice guidelines for healthcare-associated ventriculitis and meningitis*. Clin Infect Dis 64:701–706. https://doi.org/10.1093/cid/cix152
Long W, Yuan J, Liu J et al (2018) Multidrug resistant brain abscess due to Acinetobacter baumannii ventriculitis cleared by intraventricular and intravenous tigecycline therapy: a case report and review of literature. Front Neurol 9 https://doi.org/10.3389/fneur.2018.00518
Sato M, Oikawa T, Sasaki T, Kodama N (1994) Brain abscess ruptured into the lateral ventricle: the usefulness of treatment by intraventricular irrigation with antibiotics. A case report Neurol Surg 22:689–693
Chan AK, Birk HS, Yue JK et al (2017) Bilateral external ventricular drain placement and intraventricular irrigation combined with concomitant serial prone patient positioning: a novel treatment for gravity-dependent layering in bacterial ventriculitis. Cureus 9:e1175. https://doi.org/10.7759/cureus.1175
Jin Whang C, Cauthen JC, Garcia Bengochea F (1974) Successful treatment of ventriculitis by continuous intraventricular irrigation with gentamicin solution. Surg Neurol 2:91–94
Wang JH, Lin PC, Chou CH et al (2014) Intraventricular antimicrobial therapy in postneurosurgical Gram-negative bacillary meningitis or ventriculitis: a hospital-based retrospective study. J Microbiol Immunol Infect 47:204–210. https://doi.org/10.1016/j.jmii.2012.08.028
Karaiskos I, Galani L, Baziaka F, Giamarellou H (2013) Intraventricular and intrathecal colistin as the last therapeutic resort for the treatment of multidrug-resistant and extensively drug-resistant Acinetobacter baumannii ventriculitis and meningitis: a literature review. Int J Antimicrob Agents 41:499–508
Al Shirawi N, Memish ZA, Cherfan A, Al Shimemeri A (2006) Post-neurosurgical meningitis due to multidrug-resistant Acinetobacter baumanii treated with intrathecal colistin: case report and review of the literature. J Chemother 18:554–558
Kumar A, Agrawal D, Sharma BS (2016) The role of endoscopic lavage in recalcitrant multidrug-resistant gram-negative ventriculitis among neurosurgical patients. World Neurosurg 93:315–323. https://doi.org/10.1016/j.wneu.2016.06.022
Gaderer C, Schaumann A, Schulz M, Thomale UW (2018) Neuroendoscopic lavage for the treatment of CSF infection with hydrocephalus in children. Child’s Nerv Syst 34:1893–1903. https://doi.org/10.1007/s00381-018-3894-7
Fortes Ferreira NPD, Otta GM, Do Amaral LLF, Da Rocha AJ (2005) Imaging aspects of pyogenic infections of the central nervous system. Top Magn Reson Imaging 16:145–154. https://doi.org/10.1097/01.rmr.0000189107.55275.f6
Marinelli L, Trompetto C, Cocito L (2014) Diffusion magnetic resonance imaging diagnostic relevance in pyogenic ventriculitis with an atypical presentation: a case report. BMC Res Notes 7:149. https://doi.org/10.1186/1756-0500-7-149
Hong JT, Son BC, Sung JH et al (2008) Significance of diffusion-weighted imaging and apparent diffusion coefficient maps for the evaluation of pyogenic ventriculitis. Clin Neurol Neurosurg 110:137–144. https://doi.org/10.1016/j.clineuro.2007.09.019
Qin G, Liang Y, Xu K et al (2020) Neuroendoscopic lavage for ventriculitis: case report and literature review. Neurochirurgie 66:127–132. https://doi.org/10.1016/j.neuchi.2019.12.005
Tabuchi S, Kadowaki M (2015) Neuroendoscopic surgery for ventriculitis and hydrocephalus after shunt infection and malfunction: preliminary report of a new strategy. Asian J Endosc Surg 8:180–184. https://doi.org/10.1111/ases.12162
Terada Y, Mineharu Y, Arakawa Y et al (2016) Effectiveness of neuroendoscopic ventricular irrigation for ventriculitis. Clin Neurol Neurosurg 146:147–151. https://doi.org/10.1016/j.clineuro.2016.05.010
Deopujari CE, Padayachy L, Azmi A et al (2018) Neuroendoscopy for post-infective hydrocephalus in children. Child’s Nerv Syst 34:1905–1914. https://doi.org/10.1007/s00381-018-3901-z
Wang F, Yao XY, Zou ZR et al (2017) Management of pyogenic cerebral ventriculitis by neuroendoscopic surgery. World Neurosurg 98:6–13. https://doi.org/10.1016/j.wneu.2016.10.103
Guanci MMK (2013) Ventriculitis of the central nervous system. Crit Care Nurs Clin North Am 25:399–406. https://doi.org/10.1016/j.ccell.2013.04.005
Fitzhardinge PM, Kazemi M, Ramsay M, Stern L (1974) Long-term sequelae of neonatal meningitis. Dev Med Child Neurol 16:3–10. https://doi.org/10.1111/j.1469-8749.1974.tb02704.x
Markantonis SL, Markou N, Fousteri M et al (2009) Penetration of colistin into cerebrospinal fluid. Antimicrob Agents Chemother 53:4907–4910. https://doi.org/10.1128/AAC.00345-09
Lang M, Habboub G, Moore NZ et al (2018) Neuroendoscopic evacuation of intraventricular empyema using a side-cutting aspiration device. J Clin Neurosci 47:323–327. https://doi.org/10.1016/j.jocn.2017.09.029
Tandean S, Hendriansyah L, Djokomuljanto S et al (2018) Neuroendoscopic aspiration and lavage of intraventricular empyema following shunt infection in infants. Pan Afr Med J 31:1–5. https://doi.org/10.11604/pamj.2018.31.15.16631
Chowdhry SA, Cohen AR (2013) Intraventricular neuroendoscopy: complication avoidance and management. World Neurosurg 79:S15.e1-S15.e10. https://doi.org/10.1016/j.wneu.2012.02.030
Lebel MH, McCracken GH (1989) Delayed cerebrospinal fluid sterilization and adverse outcome of bacterial meningitis in infants and children. Pediatrics 83:161–167. https://doi.org/10.1016/0278-2316(90)90008-4
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Garrahan’s Pediatric Hospital.
Consent to participate
The patient gave consent to use his information and images for research proposes.
Consent for publication
The patient gave consent to use his information and images for publication.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ochoa, A., Argañaraz, R. & Mantese, B. Neuroendoscopic lavage for the treatment of pyogenic ventriculitis in children: personal series and review of the literature. Childs Nerv Syst 38, 597–604 (2022). https://doi.org/10.1007/s00381-021-05413-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-021-05413-3