Abstract
Purpose
Severe acidosis is one of the strongest predictors of neurologic outcomes in full-term infants with suspected hypoxic-ischemic encephalopathy. However, the relative importance of acidosis as a predictor of outcomes in preterm infants is much less clear. The goals of the present study were to examine the association between postnatal acidosis and severe intraventricular hemorrhage (IVH) and to establish a new score model including acid-base status after birth for predicting the risk of this morbidity.
Methods
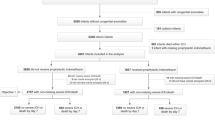
The study sample was very low birth weight (VLBW) infants in the Korean Neonatal Network (KNN) cohort registry, collected prospectively from January 2013 to December 2014. Infants with blood pH and base deficit (BD) values collected within the first hour after birth, and documentation of severe IVH, were included. Multivariate stepwise logistic regression analysis was used to determine the contribution of postnatal acidosis to predicting severe IVH in VLBW infants. In addition, a prediction model was developed.
Results
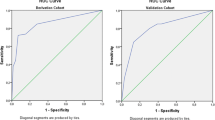
Data from 2518 VLBW infants were analyzed. Infants with postnatal acidosis had a higher incidence of severe IVH. The clinical model plus blood BD values improved predictive performance, compared with models using only perinatal data or blood pH.
Conclusions
A prediction model for severe IVH was developed using the KNN registry of VLBW infants. Immediate postnatal acidosis, defined based on blood BD, was associated with a higher-risk-adjusted incidence of severe IVH.


Similar content being viewed by others
References
Ambalavanan N, Carlo WA, Shankaran S, Bann CM, Emrich SL, Higgins RD, Tyson JE, O'Shea TM, Laptook AR, Ehrenkranz RA, Donovan EF, Walsh MC, Goldberg RN, Das A; National Institute of Child Health and Human Development Neonatal Research Network (2006) Predicting outcomes of neonates diagnosed with hypoxemic-ischemic encephalopathy. Pediatrics 118(5):2084–2093
Sarkar S, Bhagat I, Dechert R, Schumacher RE, Donn SM (2009) Severe intraventricular hemorrhage in preterm infants: comparison of risk factors and short-term neonatal morbidities between grade 3 and grade 4 intraventricular hemorrhage. Am J Perinatol 26(6):419–424
Ertan AK, Tanriverdi HA, Meier M, Schmidt W (2006) Perinatal risk factors for neonatal intracerebral hemorrhage in preterm infants. Eur J Obstet Gynecol Reprod Biol 127(1):29–34
Vogtmann C, Koch R, Gmyrek D, Kaiser A, Friedrich A (2012) Risk-adjusted intraventricular hemorrhage rates in very premature infants: towards quality assurance between neonatal units. Dtsch Arztebl Int 109(31–32):527–533
Randolph DA, Nolen TL, Ambalavanan N, Carlo WA, Peralta-Carcelen M, Das A, Bell EF, Davis AS, Laptook AR, Stoll BJ, Shankaran S, Higgins RD; Generic Database and Follow-Up Subcommittees for the Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network (2014) Outcomes of extremely low birthweight infants with acidosis at birth. Arch Dis Child Fetal Neonatal Ed 99(4):F263–F268
Malin GL, Morris RK, Khan KS (2010) Strength of association between umbilical cord pH and perinatal and long term outcomes: systematic review and meta-analysis. BMJ 13 c1471:340
Yeh P, Emary K, Impey L (2012) The relationship between umbilical cord arterial pH and serious adverse neonatal outcome: analysis of 51, 519 consecutive validated samples. BJOG 119(7):824–831
Lee JY, Kim HS, Jung E, Kim ES, Shim GH, Lee HJ, Lee JA, Choi CW, Kim EK, Kim BI, Choi JH (2010) Risk factors for periventricular-intraventricular hemorrhage in premature infants. J Korean Med Sci 25(3):418–424
Levene MI, Fawer CL, Lamont RF (1982) Risk factors in the development of intraventricular haemorrhage in the preterm neonate. Arch Dis Child 57(6):410–417
Vergani P, Patanè L, Doria P, Borroni C, Cappellini A, Pezzullo JC, Ghidini A (2000) Risk factors for neonatal intraventricular haemorrhage in spontaneous prematurity at 32 weeks gestation or less. Placenta 21(4):402–407
Ment LR, Stewart WB, Duncan CC, Lambrecht R (1982) Beagle puppy model of intraventricular hemorrhage. J Neurosurg 57(2):219–223
Short BL, Walker LK, Traystman RJ (1994) Impaired cerebral autoregulation in the newborn lamb during recovery from severe, prolonged hypoxia, combined with carotid artery and jugular vein ligation. Crit Care Med 22(8):1262–1268
Bassan H, Gauvreau K, Newburger JW, Tsuji M, Limperopoulos C, Soul JS, Walter G, Laussen PC, Jonas RA, du Plessis AJ (2005) Identification of pressure passive cerebral perfusion and its mediators after infant cardiac surgery. Pediatr Res 57(1):35–41
Bassan H, Feldman HA, Limperopoulos C, Benson CB, Ringer SA, Veracruz E, Soul JS, Volpe JJ, du Plessis AJ (2006) Periventricular hemorrhagic infarction: risk factors and neonatal outcome. Pediatr Neurol 35(2):85–92
L evene MI, de Vries L (1984) Extension of neonatal intraventricular haemorrhage. Arch Dis Child 59(7):631–636
Vela-Huerta MM, Amador-Licona M, Medina-Ovando N, Aldana-Valenzuela C (2009) Factors associated with early severe intraventricular haemorrhage in very low birth weight infants. Neuropediatrics 40(5):224–227
Luque MJ, Tapia JL, Villarroel L, Marshall G, Musante G, Carlo W, Kattan J, Network NN (2014) A risk prediction model for severe intraventricular hemorrhage in very low birth weight infants and the effect of prophylactic indomethacin. J Perinatol 34(1):43–48
Kaiser JR, Gauss CH, Pont MM, Williams DK (2006) Hypercapnia during the first 3 days of life is associated with severe intraventricular hemorrhage in very low birth weight infants. J Perinatol 26(5):279–285
Synnes AR, Chien LY, Peliowski A, Baboolal R, Lee SK, Network CNICU (2001) Variations in intraventricular hemorrhage incidence rates among Canadian neonatal intensive care units. J Pediatr 138(4):525–531
Heuchan AM, Evans N, Henderson Smart DJ, Simpson JM (2002) Perinatal risk factors for major intraventricular haemorrhage in the Australian and New Zealand neonatal network, 1995-97. Arch Dis Child Fetal Neonatal Ed 86(2):F86–F90
Goldstein RF, Thompson RJ Jr, Oehler JM, Brazy JE (1995) Influence of acidosis, ypoxemia, and hypotension on neurodevelopmental outcome in very low birth weight infants. Pediatrics 95(2):238–243
Coskun Y, Isik S, Bayram T, Urgun K, Sakarya S, Akman I (2018) A clinical scoring system to predict the development of intraventricular hemorrhage (IVH) in premature infants. Childs Nerv Syst 34(1):129–136
Shah PS, Raju NV, Beyene J, Perlman M (2003) Recovery of metabolic acidosis in term infants with postasphyxial hypoxic-ischemic encephalopathy. Acta Paediatr 92(8):941–947
Saugstad OD, Rootwelt T, Aalen O (1998) Resuscitation of asphyxiated newborn infants with room air or oxygen: an international controlled trial: the Resair 2 study. Pediatrics 102(1):e1
Szpecht D, Szymankiewicz M, Nowak I, Gadzinowski J (2016) Intraventricular hemorrhage in neonates born before 32 weeks of gestation-retrospective analysis of risk factors. Childs Nerv Syst 32(8):1399–1404
Goswami I, Lodha A, Dalgleish S, Mohammad K (2017) Early onset Escherichia coli sepsis and severe intraventricular hemorrhage in extremely premature infants: cases series and literature review. Acad J Ped Neonatol 3(3):555612
Acknowledgements
This study was supported by the research program funded by the Korea Centers for Disease Control and Prevention (2016-ER6307-01) and statistical consultation was provided by a grant from the Korea Health Technology R&D Project from the Korea Health Industry Development Institute, funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI14C1062).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest or any financial relationships relevant to this article to disclose.
Rights and permissions
About this article
Cite this article
Lee, J., Hong, M., Yum, S.K. et al. Perinatal prediction model for severe intraventricular hemorrhage and the effect of early postnatal acidosis. Childs Nerv Syst 34, 2215–2222 (2018). https://doi.org/10.1007/s00381-018-3868-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-018-3868-9