Abstract
Background
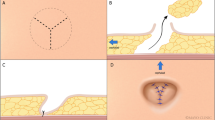
Closure of the skin defect in myelomeningocele repair determines the quality of the surgical result. In large myelomeningoceles, the direct closure or by skin undermining may not be possible. In these cases, the skin defect must be closed using flaps to provide a tension-free and successful closure.
Methods
In this procedure, after neurosurgical repair and closure of the placode, the defect surgically becomes an ovoid in shape. Then, this defect is closed by transposition of two dorsal intercostal artery perforator propeller flaps. The defect size was > 5 cm in diameter. The localization of the lesion was lumbosacral.
Result
A successful tension-free one-stage closure was obtained, without necrosis. Healing was uneventful without any complications and the coverage remained stable over 9 years with the child growth.
Conclusion
The dorsal intercostal artery perforator propeller flap enables the surgeon to achieve a tension-free defect closure of considerably large myelomeningocele defects. This type of closure provides a durable coverage and a soft tissue padding over the neural tissues that persist with the child growth. The dorsal intercostal artery perforator propeller flap seems to be a useful closure of large myelomeningocele defects.






Similar content being viewed by others
References
Reigel DH (1996) Myelomeningocele. In: Cheek WR (ed) Atlas of pediatric neurosurgery, 1st edn. W.B. Saunders, Philadelphia, p 1e9
Basterzi Y, Tenekeci G (2016) Dorsal intercostal artery perforator propeller flaps: a reliable option in reconstruction of large meningomyelocele defects. Ann Plast Surg 76(4):434e7
Isik D, Tekes L, Eseoglu M et al (2011) Closure of large myelomeningocele defects using dorsal intercostal artery perforator flap. Ann Plast Surg 67:159e63
Mutaf M, Sunay M, Bulut Ö (2008) The “reading man” procedure a new technique for the closure of circular skin defects. Ann Plast Surg 60:420e5
Mutaf M, Temel M, Günal E (2012) The reading man flap for closure of large meningomyelocele defects. J Plast Reconstr Aesthet Surg 65:578e83
Campobasso P, Pesce C, Costa L et al (2004) The use of Limberg skin flap for closure of large lumbosacral myelomeningoceles. Pediatr Surg Int 20:144e7
Lapid O, Rosenberg L, Cohen A (2001) Meningomyelocele reconstruction with bilobed flaps. Br J Plast Surg 54:570e2
McCraw JB, Penix JO, Freeman BG et al (1987) Soft-tissue repair of myelomeningocele defects using bilateral latissimus dorsi and trapezius musculocutaneous flaps. Ann Plast Surg 18:147e55
Sarifakioglu N, Bingul F, Terzioglu A et al (2003) Bilateral split latissimus dorsi V-Y flaps for closure of large thoracolumbar meningomyelocele defects. Br J Plast Surg 56:303e6
Isik D, Tekes L, Eseoglu M, Isik Y, Bilici S, Atik B (2011) Closure of large myelomeningocele defects using dorsal intercostal artery perforator flap. Ann Plast Surg 67(2):159-163
Duffy FJ Jr, Weprin BE, Swift DM (2004) A new approach to closure of large lumbosacral myelomeningoceles: the superior gluteal artery perforator flap. Plast Reconstr Surg 53:305e10
Mangels KJ, Tulipan N, Bruner JP et al (2000) Use of bipedicular advancement flaps for intrauterine closure of myeloschisis. Pediatr Neurosurg 32:52e6
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
N/A
Disclaimer
None of the authors has a financial interest in any of the products, devices or drugs mentioned in this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gutierrez-Ontalvilla, P., Blanco, E.L. & Miranda, P. Long-term follow-up of myelomeningocele defect closure with dorsal intercostal artery perforator propeller flaps. Childs Nerv Syst 35, 1219–1222 (2019). https://doi.org/10.1007/s00381-018-04030-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-018-04030-x