Abstract
Background
Incidental findings on neuroimaging in the pediatric population are an emerging treatment challenge. Treatment options for these incidental childhood brain mass lesions, which radiologically may be assumed to be low-grade gliomas (LGG), vary, ranging from careful conservative “wait and scan” treatment to surgical biopsy, gross total resection, and upfront radiation and/or chemotherapy. As malignant transformation of LGG in children is extremely rare, some series advocate careful conservative management of these lesions; however, universal treatment protocols are not totally agreed upon.
Illustrative case
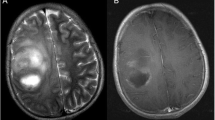
We present the case of a 10-year-old boy with a fronto-basal incidental cerebral mass lesion, suspected to be a low-grade glial neoplasm. Initially, magnetic resonance imaging (MRI) was done to rule out a pathology causing his growth to be delayed. A treatment with growth hormone was initiated. After close clinical and radiological follow-up of this asymptomatic lesion for 6 years, a minimal growth of the lesion was seen, which we decided to continue following. After 7 years, a clear growth with new contrast enhancement was seen on routine MRI. At this point, the lesion was surgically resected. The diagnosis was, surprisingly, glioblastoma multiforme (WHO grade IV, BRAF V-600E mutation).
Discussion
Malignant transformation of LGGs in children is a very rare phenomenon. This is to our knowledge the first well-documented case describing malignant transformation of a suspected benign pediatric cerebral mass lesion, which did not undergo radiation, in a patient without a cancer predisposition syndrome (e.g., neurofibromatosis), with the transformation occurring after such a long follow-up period. The management of these lesions is still controversial. Unfortunately, radiological risk factors for malignant transformation of such lesions in the pediatric age group are lacking.
Conclusion
Conservative treatment of incidental cerebral mass lesions in children seems a valid option. These lesions should probably be followed indefinitely, while carefully watching for changes in imaging characteristics.




Similar content being viewed by others
References
Graf WD, Kayyali HR, Alexander JJ, Simon SD, Morriss MC (2008) Neuroimaging-use trends in nonacute pediatric headache before and after clinical practice parameters. Pediatrics 122:e1001–e1005
Perret C, Boltshauser E, Scheer I, Kellenberger CJ, Grotzer MA (2011) Incidental findings of mass lesions on neuroimages in children. Neurosurg Focus 31:E20
Graf WD, Kayyali HR, Abdelmoity AT, Womelduff GL, Williams AR, Morriss MC (2010) Incidental neuroimaging findings in nonacute headache. J Child Neurol 25:1182–1187
Ali ZS, Lang SS, Sutton LN (2014) Conservative management of presumed low-grade gliomas in the asymptomatic pediatric population. World neurosurg 81:368–373
Brown PD, Wald JT, McDermott MW, Baumann GS, Cloughesy TF, Oncodiagnosis panel RSA (2003) Oncodiagnosis panel: 2002. Patient’s symptoms not related to the lesion seen in the MR images. Radiographics Rev Publ Radiol Soc North Am Inc 23:1591–1611
Bredlau AL, Constine LS, Silberstein HJ, Milano MT, Korones DN (2012) Incidental brain lesions in children: to treat or not to treat? J Neuro-Oncol 106:589–594
Roth J, Keating RF, Myseros JS, Yaun AL, Magge SN, Constantini S (2012) Pediatric incidental brain tumors: a growing treatment dilemma. J Neurosurg Pediatr 10:168–174
Berger MS, Deliganis AV, Dobbins J, Keles GE (1994) The effect of extent of resection on recurrence in patients with low grade cerebral hemisphere gliomas. Cancer 74:1784–1791
Jakola AS, Myrmel KS, Kloster R, Torp SH, Lindal S, Unsgard G et al (2012) Comparison of a strategy favoring early surgical resection vs a strategy favoring watchful waiting in low-grade gliomas. JAMA 308:1881–1888
Janny P, Cure H, Mohr M, Heldt N, Kwiatkowski F, Lemaire JJ et al (1994) Low grade supratentorial astrocytomas. Management and prognostic factors. Cancer 73:1937–1945
Keles GE, Lamborn KR, Berger MS (2001) Low-grade hemispheric gliomas in adults: a critical review of extent of resection as a factor influencing outcome. J Neurosurg 95:735–745
Smith JS, Chang EF, Lamborn KR, Chang SM, Prados MD, Cha S et al (2008) Role of extent of resection in the long-term outcome of low-grade hemispheric gliomas. J Clin Oncol Off J Am Soc Clin Oncol 26:1338–1345
Mistry M, Zhukova N, Merico D, Rakopoulos P, Krishnatry R, Shago M et al (2015) BRAF mutation and CDKN2A deletion define a clinically distinct subgroup of childhood secondary high-grade glioma. J Clin Oncol Off J Am Soc Clin Oncol 33:1015–1022
Winograd E, Pencovich N, Yalon M, Soffer D, Beni-Adani L, Constantini S (2012) Malignant transformation in pediatric spinal intramedullary tumors: case-based update. Child's Nerv Syst : ChNS : Off J Int Soc Pediatr Neurosurg 28:1679–1686
Shay V, Fattal-Valevski A, Beni-Adani L, Constantini S (2012) Diagnostic delay of pediatric brain tumors in Israel: a retrospective risk factor analysis. Child's Nerv Syst : ChNS : Off J Int Soc Pediatr Neurosurg 28:93–100
Ellis JA, Waziri A, Balmaceda C, Canoll P, Bruce JN, Sisti MB (2009) Rapid recurrence and malignant transformation of pilocytic astrocytoma in adult patients. J Neuro-Oncol 95:377–382
Stuer C, Vilz B, Majores M, Becker A, Schramm J, Simon M (2007) Frequent recurrence and progression in pilocytic astrocytoma in adults. Cancer 110:2799–2808
Pignatti F, van den Bent M, Curran D, Debruyne C, Sylvester R, Therasse P et al (2002) Prognostic factors for survival in adult patients with cerebral low-grade glioma. J Clin Oncol Off J Am Soc Clin Oncol 20:2076–2084
Aghi MK, Nahed BV, Sloan AE, Ryken TC, Kalkanis SN, Olson JJ (2015) The role of surgery in the management of patients with diffuse low grade glioma: a systematic review and evidence-based clinical practice guideline. J Neuro-Oncol 125:503–530
Soffietti R, Baumert BG, Bello L, von Deimling A, Duffau H, Frenay M et al (2010) Guidelines on management of low-grade gliomas: report of an EFNS-EANO Task Force. Eur J Neurol 17:1124–1133
Broniscer A (2015) Malignant transformation of low-grade gliomas in children: lessons learned from rare medical events. J Clin Oncol Off J Am Soc Clin Oncol 33:978–979
Unal E, Koksal Y, Cimen O, Paksoy Y, Tavli L (2008) Malignant glioblastomatous transformation of a low-grade glioma in a child. Child's Nerv Syst : ChNS : Off J Int Soc Pediatr Neurosurg 24:1385–1389
Pollack IF (2014) Management of low-grade gliomas in childhood. World Neurosurg 81:265–267
Ishibashi K, Inoue T, Fukushima H, Watanabe Y, Iwai Y, Sakamoto H et al (2016) Pediatric thalamic glioma with H3F3A K27M mutation, which was detected before and after malignant transformation: a case report. Child's Nerv Syst : ChNS : Off J Int Soc Pediatr Neurosurg 32:2433–2438
Patterson BC, Chen Y, Sklar CA, Neglia J, Yasui Y, Mertens A et al (2014) Growth hormone exposure as a risk factor for the development of subsequent neoplasms of the central nervous system: a report from the childhood cancer survivor study. J Clin Endocrinol Metab 99:2030–2037
Shen L, Sun CM, Li XT, Liu CJ, Zhou YX (2015) Growth hormone therapy and risk of recurrence/progression in intracranial tumors: a meta-analysis. Neurol Sci Off J Ital Neurol Soc Ital Soc Clin Neurophysiol 36:1859–1867
Pirotte BJ, Lubansu A, Massager N, Wikler D, Van Bogaert P, Levivier M et al (2010) Clinical interest of integrating positron emission tomography imaging in the workup of 55 children with incidentally diagnosed brain lesions. J Neurosurg Pediatr 5:479–485
Wisoff JH, Sanford RA, Heier LA, Sposto R, Burger PC, Yates AJ et al (2011) Primary neurosurgery for pediatric low-grade gliomas: a prospective multi-institutional study from the Children’s Oncology Group. Neurosurgery 68:1548–1554 discussion 54-5
Kruer MC, Kaplan AM, Etzl MM Jr, Carpentieri DF, Dickman PS, Chen K et al (2009) The value of positron emission tomography and proliferation index in predicting progression in low-grade astrocytomas of childhood. J Neuro-Oncol 95:239–245
Acknowledgments
We would like to thank Mrs. Adina Sherer for the medical editing of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Disclosure of funding
None.
Rights and permissions
About this article
Cite this article
Soleman, J., Roth, J., Ram, Z. et al. Malignant transformation of a conservatively managed incidental childhood cerebral mass lesion: controversy regarding management paradigm. Childs Nerv Syst 33, 2169–2175 (2017). https://doi.org/10.1007/s00381-017-3566-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-017-3566-z