Abstract
Background
Intracranial germ cell tumors (GCTs) frequently take an insidious clinical course before diagnosis. To date, clinical latency has been discussed in the context of germinoma in the suprasellar area and basal ganglia.
Objective
In this study, we classified the clinical latency of intracranial GCTs into three categories and described their characteristics in order to understand the full spectrum of the phenomenon.
Methods
In a cohort of 181 patients with intracranial GCTs, 17 patients had a delayed diagnosis of more than 3 months (90 days) from the initial brain magnetic resonance imaging to the definitive GCT diagnosis. Clinical records and radiological data of the patients were reviewed.
Results
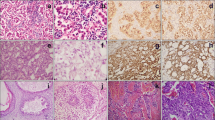
The patients with a delayed diagnosis were categorized into three groups according to their tumor location: suprasellar (nine patients), basal ganglia (six patients), and pineal (two patients). Initial symptomatology corresponded with the tumor location: central diabetes insipidus for the suprasellar group, hemiparesis for the basal ganglia group, and precocious puberty for the pineal group. The overall survival of patients with germinoma and delayed diagnosis was significantly shorter than that of patients who were diagnosed within 3 months (P = 0.002).
Conclusions
Clinical latency and delayed diagnosis are not restricted to germinomas in the suprasellar area and basal ganglia; they are canonical features of intracranial GCTs including pineal non-germinomatous GCTs. Early detection and proactive diagnosis of these tumors are required because diagnosis delay may negatively influence patient survival.






Similar content being viewed by others
References
Cho KT, Wang KC, Kim SK, Shin SH, Chi JG, Cho BK (2002) Pediatric brain tumors: statistics of SNUH, Korea (1959–2000). Childs Nerv Syst 18(1–2):30–37
Goodwin TL, Sainani K, Fisher PG (2009) Incidence patterns of central nervous system germ cell tumors: a SEER study. J Pediatr Hematol Oncol 31(8):541–544
Matsutani M, Sano K, Takakura K, Fujimaki T, Nakamura O, Funata N, Seto T (1997) Primary intracranial germ cell tumors: a clinical analysis of 153 histologically verified cases. J Neurosurg 86(3):446–455
Sonoda Y, Kumabe T, Sugiyama S, Kanamori M, Yamashita Y, Saito R, Ariga H, Takai Y, Tominaga T (2008) Germ cell tumors in the basal ganglia: problems of early diagnosis and treatment. J Neurosurg Pediatr 2(2):118–124
Crawford JR, Santi MR, Vezina G, Myseros JS, Keating RF, LaFond DA, Rood BR, MacDonald TJ, Packer RJ (2007) CNS germ cell tumor (CNSGCT) of childhood: presentation and delayed diagnosis. Neurology 68(20):1668–1673
Birnbaum T, Pellkofer H, Buettner U (2008) Intracranial germinoma clinically mimicking chronic progressive multiple sclerosis. J Neurol 255(5):775–776
Kato T, Sawamura Y, Tada M, Murata J, Abe H, Shirato H, Fujieda K (1998) Occult neurohypophyseal germinomas in patients presenting with central diabetes insipidus. Neurosurg Focus 5(1):e6
Phi JH, Kim SK, Lee J, Park CK, Kim IH, Ahn HS, Shin HY, Kim IO, Jung HW, Kim DG, Paek SH, Wang KC (2013) The enigma of bifocal germ cell tumors in the suprasellar and pineal regions: synchronous lesions or metastasis? J Neurosurg Pediatr 11(2):107–114
Phi JH, Cho BK, Kim SK, Paeng JC, Kim IO, Kim IH, Kim DG, Jung HW, Kim JE, Wang KC (2010) Germinomas in the basal ganglia: magnetic resonance imaging classification and the prognosis. J Neurooncol 99(2):227–236
Carel JC, Leger J (2008) Clinical practice. Precocious puberty. N Engl J Med 358(22):2366–2377
Dobrovoljac M, Hengartner H, Boltshauser E, Grotzer MA (2002) Delay in the diagnosis of paediatric brain tumours. Eur J Pediatr 161(12):663–667
Flores LE, Williams DL, Bell BA, O’Brien M, Ragab AH (1986) Delay in the diagnosis of pediatric brain tumors. Am J Dis Child 140(7):684–686
Edgeworth J, Bullock P, Bailey A, Gallagher A, Crouchman M (1996) Why are brain tumours still being missed? Arch Dis Child 74(2):148–151
Mootha SL, Barkovich AJ, Grumbach MM, Edwards MS, Gitelman SE, Kaplan SL, Conte FA (1997) Idiopathic hypothalamic diabetes insipidus, pituitary stalk thickening, and the occult intracranial germinoma in children and adolescents. J Clin Endocrinol Metab 82(5):1362–1367
De Buyst J, Massa G, Christophe C, Tenoutasse S, Heinrichs C (2007) Clinical, hormonal and imaging findings in 27 children with central diabetes insipidus. Eur J Pediatr 166(1):43–49
Hamilton BE, Salzman KL, Osborn AG (2007) Anatomic and pathologic spectrum of pituitary infundibulum lesions. AJR Am J Roentgenol 188(3):W223–W232
Shin JH, Lee HK, Choi CG, Suh DC, Kim CJ, Hong SK, Na DG (2001) MR imaging of central diabetes insipidus: a pictorial essay. Korean J Radiol 2(4):222–230
Chung SJ, Lee SY, Shin CH, Yang SW (2007) Clinical, endocrinological and radiological courses in patients who was initially diagnosed as idiopathic central diabetes insipidus. Korean J Pediatr 50(11):1110–1115
Maghnie M, Cosi G, Genovese E, Manca-Bitti ML, Cohen A, Zecca S, Tinelli C, Gallucci M, Bernasconi S, Boscherini B, Severi F, Arico M (2000) Central diabetes insipidus in children and young adults. N Engl J Med 343(14):998–1007
Leger J, Velasquez A, Garel C, Hassan M, Czernichow P (1999) Thickened pituitary stalk on magnetic resonance imaging in children with central diabetes insipidus. J Clin Endocrinol Metab 84(6):1954–1960
Bettendorf M, Fehn M, Grulich-Henn J, Selle B, Darge K, Ludecke DK, Heinrich UE, Saeger W (1999) Lymphocytic hypophysitis with central diabetes insipidus and consequent panhypopituitarism preceding a multifocal, intracranial germinoma in a prepubertal girl. Eur J Pediatr 158(4):288–292
Cuccia V, Alderete D (2010) Suprasellar/pineal bifocal germ cell tumors. Childs Nerv Syst 26(8):1043–1049
Lafay-Cousin L, Millar BA, Mabbott D, Spiegler B, Drake J, Bartels U, Huang A, Bouffet E (2006) Limited-field radiation for bifocal germinoma. Int J Radiat Oncol Biol Phys 65(2):486–492
Lee L, Saran F, Hargrave D, Bodi I, Bassi S, Hortobagyi T (2006) Germinoma with synchronous lesions in the pineal and suprasellar regions. Childs Nerv Syst 22(12):1513–1518
Sudo A, Shiga T, Okajima M, Takano K, Terae S, Sawamura Y, Ohnishi A, Nagashima K, Saitoh S (2003) High uptake on 11C-methionine positron emission tomographic scan of basal ganglia germinoma with cerebral hemiatrophy. AJNR Am J Neuroradiol 24(9):1909–1911
Takeda N, Fujita K, Katayama S, Uchihashi Y, Okamura Y, Nigami H, Hashimoto K, Kohmura E (2004) Germinoma of the basal ganglia. An 8-year asymptomatic history after detection of abnormality on CT. Pediatr Neurosurg 40(6):306–311
Okamoto K, Ito J, Ishikawa K, Morii K, Yamada M, Takahashi N, Tokiguchi S, Furusawa T, Sakai K (2002) Atrophy of the basal ganglia as the initial diagnostic sign of germinoma in the basal ganglia. Neuroradiology 44(5):389–394
Ozelame RV, Shroff M, Wood B, Bouffet E, Bartels U, Drake JM, Hawkins C, Blaser S (2006) Basal ganglia germinoma in children with associated ipsilateral cerebral and brain stem hemiatrophy. Pediatr Radiol 36(4):325–330
Lee J, Lee BL, Yoo KH, Sung KW, Koo HH, Lee SJ, Choi JY, Lee KH, Lee JI, Shin HJ, Kim JH, Suh YL, Lee KH, Lee M (2009) Atypical basal ganglia germinoma presenting as cerebral hemiatrophy: diagnosis and follow-up with 11C-methionine positron emission tomography. Childs Nerv Syst 25(1):29–37
Oosterhuis JW, Stoop H, Honecker F, Looijenga LH (2007) Why human extragonadal germ cell tumours occur in the midline of the body: old concepts, new perspectives. Int J Androl 30(4):256–263
Acknowledgments
This study was supported by a grant from the Clinical Medical Scientist R&D Project, Ministry for Health, Welfare, and Family Affairs, Republic of Korea (grant no. A102053; to J.H. Phi).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Phi, J.H., Kim, SK., Lee, Y.A. et al. Latency of intracranial germ cell tumors and diagnosis delay. Childs Nerv Syst 29, 1871–1881 (2013). https://doi.org/10.1007/s00381-013-2164-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-013-2164-y