Abstract
Purpose
Cervical spine clearance in severely injured children after trauma is often difficult because of unique injury patterns, concerns about radiation exposure to growing tissue, and unfamiliarity with unstable cervical injuries. We prospectively assessed the utility of four radiographic modalities to clear the cervical spine in children after severe trauma.
Methods
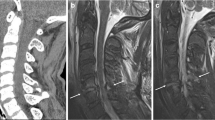
Twenty-four comatose, intubated children with severe traumatic injuries underwent radiographic evaluation to clear the cervical spine. Each patient had plain radiographs, flexion–extension radiographs under fluoroscopy, computed tomography (CT), and magnetic resonance (MR) imaging within 10 days of admission. Patients underwent cervical spine flexion–extension radiographs 2–3 months after trauma to detect late instability. Sensitivity and specificity for each radiographic modality was determined.
Results
Plain cervical spine radiographs demonstrated sensitivity of 100% and specificity of 95%; flexion–extension radiographs had “indeterminate” sensitivity and specificity of 100%. For CT, sensitivity was 100% and specificity was 95%, and for MR imaging, sensitivity was 100% and specificity was 74%.
Conclusions
There was a low prevalence of cervical instability in this high-risk group. Plain radiographs, flexion–extension radiographs, and CT all had high sensitivities and specificities. MR imaging had a high false-positive rate, making it sensitive but not specific. The data support using either CT or plain radiographs as the initial cervical spine screening study, but CT is recommended because of its superior ability to detect critical injuries. To definitively rule out ligamentous instability after a negative screening CT scan or cervical spine X-ray, these data support using flexion–extension X-rays with fluoroscopy and not MR imaging.


Similar content being viewed by others
References
Grabb PA (2002) Management of pediatric cervical spine and spinal cord injuries. Neurosurgery 50: S85–S99
Anderson RC, Kan P, Vanaman M, Rubsam J, Hansen KW, Scaife ER, Brockmeyer DL (2010) Utility of a cervical spine clearance protocol after trauma in children between 0 and 3 years of age. J Neurosurg Pediatr 5:292–296
Brunetti MA, Mahesh M, Nabaweesi R, Locke P, Ziegfeld S, Brown R (2011) Diagnostic radiation exposure in pediatric trauma patients. J Trauma 70(2):E24–E28
Committee on Trauma—American College of Surgeons (2008) ATLS Advanced Trauma Life Support Program for Doctors. American College of Surgeons, Chicago
Como JJ, Thompson MA, Anderson JS, Shah RR, Claridge JA, Yowler CJ, Malangoni MA (2007) Is magnetic resonance imaging essential in clearing the cervical spine in obtunded patients with blunt trauma? J Trauma 63:544–549
Como JJ, Diaz JJ, Dunham CM, Chiu WC, Duane TM, Capella JM, Holevar MR, Khwaja KA, Mayglothling JA, Shapiro MB, Winston ES (2009) Practice management guidelines for identification of cervical spine injuries following trauma: update from the eastern association for the surgery of trauma practice management guidelines committee. J Trauma 67:651–659
D'Alise MD, Benzel EC, Hart BL (1999) Magnetic resonance imaging evaluation of the cervical spine in the comatose or obtunded trauma patient. J Neurosurg 91:54–59
Davis JW, Kaups KL, Cunningham MA, Parks SN, Nowak TP, Bilello JF, Williams JL (2001) Routine evaluation of the cervical spine in head-injured patients with dynamic fluoroscopy: a reappraisal. J Trauma 50:1044–1047
Dunham CM, Brocker BP, Collier BD, Gemmel DJ (2008) Risks associated with magnetic resonance imaging and cervical collar in comatose, blunt trauma patients with negative comprehensive cervical spine computed tomography and no apparent spinal deficit. Crit Care 12:R89
Ghanta MK, Smith LM, Polin RS, Marr AB, Spires WV (2002) An analysis of Eastern Association for the Surgery of Trauma practice guidelines for cervical spine evaluation in a series of patients with multiple imaging techniques. Am Surg 68:563–567, discussion 567–568
Grogan EL, Morris JA Jr, Dittus RS, Moore DE, Poulose BK, Diaz JJ, Speroff T (2005) Cervical spine evaluation in urban trauma centers: lowering institutional costs and complications through helical CT scan. J Am Coll Surg 200:160–165
Harris TJ, Blackmore CC, Mirza SK, Jurkovich GJ (2008) Clearing the cervical spine in obtunded patients. Spine (Phila Pa 1976) 33:1547–1553
Hogan GJ, Mirvis SE, Shanmuganathan K, Scalea TM (2005) Exclusion of unstable cervical spine injury in obtunded patients with blunt trauma: is MR imaging needed when multi-detector row CT findings are normal? Radiology 237:106–113
Keenan HT, Hollingshead MC, Chung CJ, Ziglar MK (2001) Using CT of the cervical spine for early evaluation of pediatric patients with head trauma. AJR Am J Roentgenol 177:1405–1409
King MA, Kanal KM, Relyea-Chew A, Bittles M, Vavilala MS, Hollingworth W (2009) Radiation exposure from pediatric head CT: a bi-institutional study. Pediatr Radiol 39:1059–1065
Laham JL, Cotcamp DH, Gibbons PA, Kahana MD, Crone KR (1994) Isolated head injuries versus multiple trauma in pediatric patients: do the same indications for cervical spine evaluation apply? Pediatr Neurosurg 21:221–226, discussion 226
Marion D, Domeier R, Dunham C, Luchette F, Haid R, Erwood S, for the Eastern Association for the Surgery of Trauma Practice Parameter Workgroup for Cervical Spine Clearance (1998) Practice parameters for identifying cervical spine injuries following trauma. Eastern Association for the Surgery of Trauma, Chicago
Menaker J, Philp A, Boswell S, Scalea TM (2008) Computed tomography alone for cervical spine clearance in the unreliable patient—are we there yet? J Trauma 64:898–903, discussion 903–904
Osenbach RK, Menezes AH (1992) Pediatric spinal cord and vertebral column injury. Neurosurgery 30:385–390
Pang D, Nemzek WR, Zovickian J (2007) Atlanto-occipital dislocation—part 2: the clinical use of (occipital) condyle-C1 interval, comparison with other diagnostic methods, and the manifestation, management, and outcome of atlanto-occipital dislocation in children. Neurosurgery 61:995–1015, discussion 1015
Pang D, Nemzek WR, Zovickian J (2007) Atlanto-occipital dislocation: part 1—normal occipital condyle-C1 interval in 89 children. Neurosurgery 61:514–521, discussion 521
Pasquale M, Fabian T (1998) Practice management guidelines for trauma from the Eastern Association for the Surgery of Trauma. J Trauma 44:941–956
Pieretti-Vanmarcke R, Velmahos GC, Nance ML, Islam S, Falcone RA Jr, Wales PW, Brown RL, Gaines BA, McKenna C, Moore FO, Goslar PW, Inaba K, Barmparas G, Scaife ER, Metzger RR, Brockmeyer DL, Upperman JS, Estrada J, Lanning DA, Rasmussen SK, Danielson PD, Hirsh MP, Consani HF, Stylianos S, Pineda C, Norwood SH, Bruch SW, Drongowski R, Barraco RD, Pasquale MD, Hussain F, Hirsch EF, McNeely PD, Fallat ME, Foley DS, Iocono JA, Bennett HM, Waxman K, Kam K, Bakhos L, Petrovick L, Chang Y, Masiakos PT (2009) Clinical clearance of the cervical spine in blunt trauma patients younger than 3 years: a multi-center study of the american association for the surgery of trauma. J Trauma 67:543–549, discussion 549–550
Prasad VS, Schwartz A, Bhutani R, Sharkey PW, Schwartz ML (1999) Characteristics of injuries to the cervical spine and spinal cord in polytrauma patient population: experience from a regional trauma unit. Spinal Cord 37:560–568
Rice HE, Frush DP, Farmer D, Waldhausen JH (2007) Review of radiation risks from computed tomography: essentials for the pediatric surgeon. J Pediatr Surg 42:603–607
Ruge JR, Sinson GP, McLone DG, Cerullo LJ (1988) Pediatric spinal injury: the very young. J Neurosurg 68:25–30
Scarrow AM, Levy EI, Resnick DK, Adelson PD, Sclabassi RJ (1999) Cervical spine evaluation in obtunded or comatose pediatric trauma patients: a pilot study. Pediatr Neurosurg 30:169–175
Sliker CW, Mirvis SE, Shanmuganathan K (2005) Assessing cervical spine stability in obtunded blunt trauma patients: review of medical literature. Radiology 234:733–739
Tomycz ND, Chew BG, Chang YF, Darby JM, Gunn SR, Nicholas DH, Ochoa JB, Peitzman AB, Schwartz E, Pape HC, Spiro RM, Okonkwo DO (2008) MRI is unnecessary to clear the cervical spine in obtunded/comatose trauma patients: the four-year experience of a level I trauma center. J Trauma 64:1258–1263
Acknowledgements
The authors wish to acknowledge the assistance of Kristin Kraus, MSc, in the preparation of this manuscript. They also wish to thank the members of the DSMB for their time, insight, and expertise in the fields of cervical and pediatric trauma: Ronald Apfelbaum, MD, J. Michael Dean, MD, MBA, and Armand Antommaria, MD, PhD.
Disclosures
The authors do not report any conflict of interest concerning the materials or methods used in this study or the findings specified in this paper. The technical fees for the MR imaging portion of the study were funded by a grant from Primary Children’s Foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Brockmeyer, D.L., Ragel, B.T. & Kestle, J.R.W. The pediatric cervical spine instability study. Childs Nerv Syst 28, 699–705 (2012). https://doi.org/10.1007/s00381-012-1696-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-012-1696-x