Abstract
Introduction
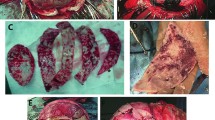
Cranial expansion has been the mainstay of initial management of children with Apert syndrome. Surgical timing is a balance between the risk of relapse if performed too early and the possibility of raised intracranial pressure and ossification defects if performed later. Primary occipital expansion has been proposed as a method to delay the timing of frontal surgery. We have applied the principal of spring expansion of patent sutures to expand the posterior cranial fossa without a cranial osteotomy.
Patients and methods
All new Apert syndrome patients seen during the 3-year period December 2004–December 2007 underwent initial occipital expansion without osteotomy using spring expansion of the patent lambdoid suture.
Results
Four new Apert syndrome patients underwent posterior spring expansion of the patent lambdoid suture. Good occipital expansion was achieved in all cases. Standard frontal advancement was performed 5–18 months later. No relapse after frontal advancement has been seen after mean follow-up of 41 months.
Conclusions
Spring expansion of the patent lambdoid suture is an alternative technique to expand the posterior cranial fossa. Compared to current techniques it has very low morbidity. Occipital expansion is thought to treat several of the mechanisms responsible for raised intracranial pressure in Apert syndrome. When performed at 6 months of age it has enabled us to delay the time at which we would normally perform frontal advancement surgery until a time when the surgical result is likely to be more stable.





Similar content being viewed by others
References
Davis C (2007) Recent developments in the treatment of craniosynostosis. ANZ J Surg 77(Suppl 1):A55
Davis C (2008) Modern functional and aesthetic treatment of craniosynostosis. ANZ J Surg 78(Suppl 1):A38
Lauritzen C, Davis C, Ivarsson A, Sanger C, Hewitt T (2008) The evolving role of springs in craniofacial surgery: the first one hundred clinical cases. Plast Reconstr Surg 121:545–554
Lauritzen C, Davis C, Sanger C (2007) Ten years experience with spring assisted cranioplasty in 150 patients. Abstract book. XII international congress of the International Society of Craniofacial Surgery. Bahia, Brazil. 23–25 August, p64
Lauritzen C, Friede H, Elander A (1996) Dynamic cranioplasty for brachycephaly. Plast Reconstr Surg 98:7–14
Guimaraes-Ferreira J, Gewalli F, Sahlin P, Friede H, Owman-Moll P, Olsson R, Lauritzen C (2001) Dynamic cranioplasty for brachycephaly in Apert syndrome: long term follow-up study. J Neurosurg 94:757–764
Davis C, Lauritzen C (2006) Distraction of patent cranial sutures. In: David D (ed) Craniofacial surgery. Proceedings of the XII international congress of the International Society of Craniofacial Surgery. Coolum, Australia: Monduzzi, pp 165–168
Arnaud E (2007) Spring-assisted skull expansion without osteotomies for bilateral cephalic flatness in infants. In: Wolfe A (ed) Craniofacial surgery. Proceedings of the XII international congress of the International Society of Craniofacial Surgery. Brazil: Monduzzi, pp 357–360
Sgouros S, Goldin JH, Hockley AD, Wake MJ (1996) Posterior skull surgery in craniosynostosis. Childs Nerv Syst 12:727–733
Renier D, Sainte-Rose C, Marchac D, Hirsch JF (1982) Intracranial pressure in craniostenosis. J Neurosurg 57:370–377
Gosain AK, McCarthy JG, Wisoff JH (1996) Morbidity associated with increased intracranial pressure in Apert and Pfeiffer syndromes: the need for long term evaluation. Plast Reconstr Surg 97:292–301
Marchac D (1978) Radical forehead remodeling for craniostenosis. Plast Reconstr Surg 61:823–835
Marchac D, Rennier D (1982) Craniofacial surgery for craniosynostosis. Little, Brown & Company, Boston
Mulliken JB, Bruneteau RJ (1991) Surgical correction of the craniofacial anomalies in Apert syndrome. Clin Plast Surg 18:277–289
Marsh JL, Galic M, Vannier MW (1991) Surgical correction of the craniofacial dysmorphology of Apert syndrome. Clin Plast Surg 18:251–275
Posnick J (2000) Apert Syndrome: evaluation and staging of reconstruction. In Craniofacial and Maxillofacial Surgery in Children and young adults. WB Saunders Company, Philadelphia
Wong GB, Kakulis EG, Mulliken JB (2000) Analysis or fronto-orbital advancement for Apert, Crouzon, Pfeiffer and Saethre-Chotzen syndromes. Plast Reconstr Surg 105:2314–2323
Wall SA, Goldin JH, Hockley AD, Wake MJ, Poole MJ, Briggs M (1994) Fronto-orbital re-operation in craniosynostosis. Br J Plast Surg 47:180–184
Marchac D, Renier D, Jones BM (1991) Experience with the “Floating forehead”. Br J Plast Surg 41:1–15
McCarthy JG, Glasberg SB, Cutting CB (1995) Twenty-year experience with early surgery for craniosynostosis: II the craniofacial synostosis syndromes and pansynostosis—results and unsolved problems. Plast Reconstr Surg 96:284–295
Wagner JD, Cohen SR, Maher H, Dauser RC, Newman MH (1995) Critical analysis of results of craniofacial surgery for nonsyndromic bicoronal synostosis. J Craniofac Surg 6:32–37
Hayward R, Dunnaway D (2007) Has the Fronto-orbital advance passed its sell-by date in the management of syndromic craniosynostosis? In: Wolfe A (ed) Craniofacial surgery. Proceedings of the XII international congress of the International Society of Craniofacial Surgery. Monduzzi, Brazil, pp 287–289
Moore M, David D (1997) Fronto-orbital advancement for Apert syndrome in infancy—why? Asian J Surg 20:19–21
Thompson DN, Jones BM, Harkness W, Gonsalez S, Hayward R (1997) Consequences of cranial vault expansion surgery for craniosynostosis. Pediatr Neurosurg 26:296–303
Gosain AK, McCarthy JG, Glatt P, Staffenberg D, Hoffman RG (1995) A study of intracranial volume in Apert syndrome. Plast Reconstr Surg 95:284–295
Hayward R, Nishal KK (2004) Management of raised intracranial pressure. Chapter 8. In The clinical management of craniosynostosis. Clinics in Developmental Medicine No 163. Cambridge University Press
Hayward R (2005) Venous hypertension in craniosynostosis. Childs Nerv Syst 21:880–888
Taylor WJ, Hayward RD, Lasjaunias P (2001) Enigma of raised intracranial pressure in patients with complex craniosynostosis: the role of abnormal intracranial venous drainage. J Neurosurg 94:377–385
Liasis A, Nishal KNN, Leighton S, Yap S, Hayward RD, Dunnaway D (2005) Adenoid-tonsillectomy to treat visual dysfunction in a child with craniosynostosis. Pediatr Neurosurg 41:197–200
Marucci D (2008) Raised intracranial pressure in Apert syndrome. Paper presented at Royal Australasian College of Surgeons Annual Scientific Meeting, 16 May, Hong Kong
Fearon J, Swift D, Bruce DA (2001) New methods for the evaluation and treatment of craniofacial dysostosis-associated cerebellar tonsillar herniation. Plast Reconstr Surg 108:1855–1861
Sahuquillo J, Rubio E, Poca MA (1994) Posterior fossa reconstruction: a surgical technique for the treatment of Chiari I malformation and Chiari I/syringomyelia complex. Neurosurgery 35:874–884
Cinalli G, Chumas P, Arnaud E (1998) Occipital remodeling and suboccipital decompression in severe craniosynostosis associated with tonsillar herniation. Neurosurgery 42:66–71
Cinalli G, Spennato P, Sainte-Rose C et al (2005) Chiari malformation in craniosynostosis. Childs Nerv Sys 21:889–901
Jones B, Dunaway D, Hayward R (2004) Chapter 19: surgery. In: The clinical management of craniosynostosis. Clinics in Developmental Medicine No 163. Cambridge University Press
Renier D, Di Rocco F, Ven R et al (2009) Translambdoid spring-assisted expansion in infants. Poster. Abstracts book: International Society of Craniofacial Surgery XIII congress, 26–30 September p66
Jeelani N, Khan A, White A (2009) Spring assisted posterior vault distraction for raised intracranial pressure. Abstracts book: International Society of Craniofacial Surgery XIII congress, 26–30 September p40
Acknowledgments
Charles Davis learned the spring principles from Professor Claes Lauritzen during a Craniofacial Fellowship in Sweden in 2003/2004.
Financial disclosure and products
The authors of this manuscript have no financial interest in the technology or techniques used in this paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Davis, C., MacFarlane, M.R. & Wickremesekera, A. Occipital expansion without osteotomies in Apert syndrome. Childs Nerv Syst 26, 1543–1548 (2010). https://doi.org/10.1007/s00381-010-1144-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-010-1144-8