Abstract
Introduction
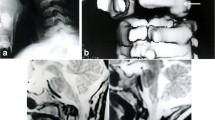
The initial treatment of bony lesions at the craniocervical junction consisted of posterior decompression with enlargement of the foramen and removal of the posterior arch of the atlas and axis vertebra. This was regardless of the site of compression. Needless to say, the results were poor when an irreducible ventral lesion at the craniocervical junction caused compression of the cervicomedullary area. It was predictable that an adverse outcome would occur in approximately 35–40% of patients treated with dorsal decompression with a fixed anterior abnormality at the craniovertebral junction. Thus, it became essential to identify the causes of failure and recognize the pathology as well as attempt to improve the treatment. The need to identify natural history led to a prospective database. This database now lists 5,300 patients who were analyzed. Of these, 2,000 were children and this has been reviewed here.
Craniovertebral abnormalities in children
Review of symptoms showed that children with craniovertebral abnormalities present with failure to thrive, weakness, basilar migraine, dysphagia, sleep apnea, scoliosis, and the cervical central cord syndrome. Torticollis was seen in the very young.
Imaging techniques and treatment for craniovertebral abnormalities
New imaging techniques were utilized as they became available. Unexplained neurological symptoms and signs associated with craniovertebral abnormalities in children required angiography which was performed with dynamic motion studies. All children with reducible craniocervical abnormalities underwent stabilization. In irreducible abnormalities, decompression was paramount with a fusion to be done immediately. The decompression was accomplished in the direction in which encroachment occurred.
Treatment algorithm and classification
A treatment algorithm was formulated as a result of this database and a classification of the craniovertebral abnormalities; that holds good for the entire spectrum.








Similar content being viewed by others
References
Barucha EP, Dastur HM (1964) Craniovertebral anomalies. Brain 87:469–480
Bell C (1830) The nervous system of the human body. Longman and Co., London, pp 403–406 Ch 118
Chamberlain WE (1938/1939) Basilar impression (platybasia). Yale J Biol Med 11:487
Dastur DK, Wadia NH, Desai AD, Sinh G (1965) Medullospinal compression due to atlanto-axial dislocation and sudden haematomyelia during decompression. Brain 88:897–924
Fang HSY, Ong AB (1962) Direct anterior approach to the upper cervical spine. J Bone Jt Surg (AM) 44:1588–1604
Ford FR (1952) Syncope, vertigo and disturbance of vision resulting from intermittent obstruction of the vertebral arteries due to defect in the odontoid process and excessive mobility of the second cervical vertebra. Bull Johns Hopkins Hosp 91:168–173
Ganguly DN, Roy KK (1964) A study on the craniovertebral joint in the man. Anat Anz 114:433–452
Gladstone J, Erickson-Powell W (1914–1915) Manifestation of occipital vertebra and fusion of atlas with occipital bone. J Anat Physiol 49:190–199
Greenberg AD (1930) Atlanto-axial dislocations. Brain 91:655–684 1968
Grisel P (1930) Enucleation de l’atlas et torticollis nasopharyngien. Presse Med 38:50–56 Paris
Lanier RR Jr (1939) Anomalous cervico-occipital skeleton in man. Anat Rec 73:189–207
List CF (1941) Neurologic syndromes accompanying developmental anomalies of occipital bone, atlas and axis. Arch Neurol Psychiat 45:577–616
Menezes AH (1995) Primary craniovertebral anomalies and the hindbrain herniation syndrome (Chiari I): Data base analysis. Pediatr Neurosurg 23:260–269
Menezes AH (1996) Rheumatological disorders. In: Menezes AH, Sonntag VKH (eds) Principles of spinal surgery. McGraw-Hill, New York, pp 705–722
Menezes AH (2003) Acquired abnormalities of the craniovertebral junction. In: Winn HR (ed) Youman’s neurological surgery. Saunders, Philadelphia, pp 4569–4585
Menezes AH (2005) Conception to implication: craniocervical junction database and treatment algorithm. Clin Neurosurg 52:154–162
Menezes AH, Graf CJ, Hibri N (1980) Abnormalities of the craniovertebral junction with cervicomedullary compression. Child’s Brain 7(l):15–30
Menezes AH, VanGilder JC, Clark CR, el-houry G (1985) Odontoid upward migration in rheumatoid arthritis. An analysis of 45 patients with cranial settling. J Neurosurg 63:500–509
Parke WW (1978) The vascular relations of the upper cervical vertebrae. Orthop Clin North Amer 9:879–889
Robertson SC, Menezes AH (1998) Occipital calvarial bone graft in posterior occipitocervical fusion. Spine 23:249–255
Ryken TC, Menezes AH (1999) Inflammatory bowel disease and the craniocervical junction. Neurosurg Focus 6(6):e10
Sawin PD, Menezes AH (1998) A comparative analysis of fusion rates and donor site morbidity for autogenic rib and iliac crest bone grafts in posterior cervical fusions. J Neurosurg 88:255–265
Schiff DCM, Parke WW (1972) The arterial blood supply of the odontoid process (Dens). Anat Rec 172:399–400
Selecki BR (1969) The effects of rotation of the atlas on the axis. Experimental work. Med J Aust 1:1012
VanGilder JC, Menezes AH, Dolan K (1987) Textbook: craniovertebral junction abnormalities. Futura, Mount Kisco, pp 1–255
Wadia NH (1967) Myelopathy complicating congenital atlanto-axial dislocation (A study of 28 cases). Brain 90:449–474
Zunkeler B, Schelper R, Menezes AH (1996) Periodontoid calcium pyrophosphate dihydrate deposition disease: “pseudogout” mass lesions of the craniocervical junction. J Neurosurg 85:803–809
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Menezes, A.H. Craniovertebral junction database analysis: incidence, classification, presentation, and treatment algorithms. Childs Nerv Syst 24, 1101–1108 (2008). https://doi.org/10.1007/s00381-008-0605-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-008-0605-9