Abstract
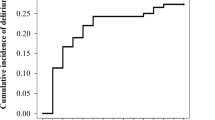
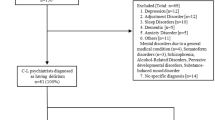
Some patients admitted to intensive care units (ICU) would develop delirium, which is associated with poor prognosis. The purpose of this retrospective study was to identify factors associated with ICU delirium in patients with acute myocardial infarction (AMI). We included 753 AMI and divided those into the ICU-delirium group (n = 110) and the non-ICU-delirium group (n = 643) according to the presence of ICU delirium. The ICU delirium was evaluated by confusion assessment method for the intensive care unit. Patient characteristics and clinical outcomes were compared between the 2 groups, and factors associated with ICU delirium were sought by multivariate analysis. The prevalence of female sex was significantly higher in the ICU-delirium group (43.6%) than in the non-ICU-delirium group (20.2%) (p < 0.001). The incidence of in-hospital death was significantly higher in the ICU-delirium group (17.3%) than in the non-ICU-delirium group (0.5%) (p < 0.001). The multivariate logistic regression analysis revealed that age [every 10 years increase: odds ratio (OR) 1.439, 95% confidence interval (CI) 1.127–1.837, p = 0.004], female sex (OR 2.237, 95%CI 1.300–3.849, p = 0.004), triple vessel disease (OR 2.317, 95%CI 1.365–3.932, p = 0.002), body mass index < 18.5 kg/m2 (OR 2.910, 95%CI 1.410–6.008, p = 0.004), use of mechanical support (OR 2.812, 95%CI 1.500–5.270, p = 0.001), respiratory failure (OR 5.342, 95%CI 3.080–9.265, p < 0.001), and use of continuous renal replacement therapy (OR 5.901, 95%CI 2.520–13.819, p < 0.001) were significantly associated with ICU delirium. In conclusion, ICU delirium was associated with in-hospital death. Older age, female sex, triple vessel disease, leanness, use of mechanical support, respiratory failure, and continuous renal replacement therapy were significantly associated with the occurrence of ICU delirium.

Similar content being viewed by others
Abbreviations
- AMI:
-
Acute myocardial infarction
- PCI:
-
Percutaneous coronary intervention
- ICU:
-
Intensive care unit
- CAM-ICU:
-
Confusion assessment method for the intensive care unit
References
Ford ES, Ajani UA, Croft JB, Critchley JA, Labarthe DR, Kottke TE, Giles WH, Capewell S (2007) Explaining the decrease in U.S. deaths from coronary disease. N Engl J Med 356(23):2388–2398
Johansson S, Rosengren A, Young K, Jennings E (2017) Mortality and morbidity trends after the first year in survivors of acute myocardial infarction: a systematic review. BMC Cardiovasc Disord 17(1):53
Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, de Ferranti S, Despres JP, Fullerton HJ, Howard VJ, Huffman MD, Judd SE, Kissela BM, Lackland DT, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Matchar DB, McGuire DK, Mohler ER, 3rd, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Willey JZ, Woo D, Yeh RW, Turner MB, American Heart Association Statistics C, Stroke Statistics S (2015) Heart disease and stroke statistics–2015 update: a report from the American Heart Association. Circulation 131(4):e29-322
Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S, Hindricks G, Kastrati A, Lenzen MJ, Prescott E, Roffi M, Valgimigli M, Varenhorst C, Vranckx P, Widimsky P, Group ESCSD (2018) 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European society of cardiology (ESC). Eur Heart J 39(2):119–177
Miki R, Takeuchi M, Imai T, Seki T, Tanaka S, Nakamura M, Kawakami K (2019) Association of intensive care unit admission and mortality in patients with acute myocardial infarction. J Cardiol 74(2):109–115
Ozaki Y, Hara H, Onuma Y, Katagiri Y, Amano T, Kobayashi Y, Muramatsu T, Ishii H, Kozuma K, Tanaka N, Matsuo H, Uemura S, Kadota K, Hikichi Y, Tsujita K, Ako J, Nakagawa Y, Morino Y, Hamanaka I, Shiode N, Shite J, Honye J, Matsubara T, Kawai K, Igarashi Y, Okamura A, Ogawa T, Shibata Y, Tsuji T, Yajima J, Iwabuchi K, Komatsu N, Sugano T, Yamaki M, Yamada S, Hirase H, Miyashita Y, Yoshimachi F, Kobayashi M, Aoki J, Oda H, Katahira Y, Ueda K, Nishino M, Nakao K, Michishita I, Ueno T, Inohara T, Kohsaka S, Ismail TF, Serruys PW, Nakamura M, Yokoi H, Ikari Y, Task Force on Primary Percutaneous Coronary Intervention of the Japanese Cardiovascular Interventional T (2022) CVIT expert consensus document on primary percutaneous coronary intervention (PCI) for acute myocardial infarction (AMI) update 2022. Cardiovasc Interv Ther 37(1):1–34
Priori SG, Blomstrom-Lundqvist C, Mazzanti A, Blom N, Borggrefe M, Camm J, Elliott PM, Fitzsimons D, Hatala R, Hindricks G, Kirchhof P, Kjeldsen K, Kuck KH, Hernandez-Madrid A, Nikolaou N, Norekval TM, Spaulding C, Van Veldhuisen DJ, Group ESCSD (2015) ESC guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: the task force for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death of the european society of cardiology (ESC). endorsed by: association for european paediatric and congenital cardiology (AEPC). Eur Heart J 36(41):2793–2867
McNicoll L, Pisani MA, Zhang Y, Ely EW, Siegel MD, Inouye SK (2003) Delirium in the intensive care unit: occurrence and clinical course in older patients. J Am Geriatr Soc 51(5):591–598
Ely EW, Shintani A, Truman B, Speroff T, Gordon SM, Harrell FE Jr, Inouye SK, Bernard GR, Dittus RS (2004) Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA 291(14):1753–1762
Girard TD, Jackson JC, Pandharipande PP, Pun BT, Thompson JL, Shintani AK, Gordon SM, Canonico AE, Dittus RS, Bernard GR, Ely EW (2010) Delirium as a predictor of long-term cognitive impairment in survivors of critical illness. Crit Care Med 38(7):1513–1520
Ely EW, Inouye SK, Bernard GR, Gordon S, Francis J, May L, Truman B, Speroff T, Gautam S, Margolin R, Hart RP, Dittus R (2001) Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). JAMA 286(21):2703–2710
Sawano M, Yamaji K, Kohsaka S, Inohara T, Numasawa Y, Ando H, Iida O, Shinke T, Ishii H, Amano T (2020) Contemporary use and trends in percutaneous coronary intervention in Japan: an outline of the J-PCI registry. Cardiovasc Interv Ther 35(3):218–226
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, White HD, Executive Group on behalf of the Joint European Society of Cardiology /American College of Cardiology /American Heart Association /World Heart Federation Task Force for the Universal Definition of Myocardial I (2018) Fourth universal definition of myocardial infarction (2018). J Am Coll Cardiol 72(18):2231–2264
Ohashi J, Sakakura K, Sasaki W, Taniguchi Y, Kani K, Yamamoto K, Tsukui T, Seguchi M, Wada H, Momomura SI, Fujita H (2021) Usefulness of 500-m walk electrocardiogram test on clinical outcomes in patients with ST-segment elevation myocardial infarction. Heart Vessels 36(1):48–57
Ishibashi S, Sakakura K, Asada S, Taniguchi Y, Jinnouchi H, Tsukui T, Yamamoto K, Seguchi M, Wada H, Fujita H (2021) Factors associated with difficulty in crossing the culprit lesion of acute myocardial infarction. Sci Rep 11(1):21403
Noguchi M, Sakakura K, Akashi N, Adachi Y, Watanabe Y, Taniguchi Y, Ibe T, Yamamoto K, Wada H, Momomura S-i, Fujita H (2019) The comparison of clinical outcomes between inferior ST-elevation myocardial infarction with right ventricular infarction versus without right ventricular infarction. Int Heart J 60(3):560–568
Hatori M, Sakakura K, Taniguchi Y, Jinnouchi H, Tsukui T, Yamamoto K, Seguchi M, Wada H, Fujita H (2021) Factors associated with in-hospital death in patients with killip class 3 acute myocardial infarction. Int Heart J 62(4):756–763
Ban S, Sakakura K, Jinnouchi H, Taniguchi Y, Tsukui T, Watanabe Y, Yamamoto K, Seguchi M, Wada H, Fujita H (2021) Association of asymptomatic low ankle-brachial index with long-term clinical outcomes in patients after acute myocardial infarction. J Atheroscler Thromb 29(7):992–1000
Kobayashi S, Sakakura K, Jinnouchi H, Taniguchi Y, Tsukui T, Watanabe Y, Yamamoto K, Seguchi M, Wada H, Fujita H (2022) Comparison of door-to-balloon time and in-hospital outcomes in patients with ST-elevation myocardial infarction between before versus after COVID-19 pandemic. Cardiovasc Interv Ther 37(4):641–650
Gibson CM, de Lemos JA, Murphy SA, Marble SJ, McCabe CH, Cannon CP, Antman EM, Braunwald E, Group TS (2001) Combination therapy with abciximab reduces angiographically evident thrombus in acute myocardial infarction: a TIMI 14 substudy. Circulation 103(21):2550–2554
Tsukui T, Sakakura K, Taniguchi Y, Yamamoto K, Seguchi M, Jinnouchi H, Wada H, Fujita H (2020) Factors associated with poor clinical outcomes of ST-elevation myocardial infarction in patients with door-to-balloon time <90 minutes. PLoS ONE 15(10):e0241251
Akinwande M, Dikko H, Samson A (2015) Variance inflation factor: as a condition for the inclusion of suppressor variable (s) in regression analysis. Open J Stat 5:754–767
Jackel M, Zotzmann V, Wengenmayer T, Duerschmied D, Biever PM, Spieler D, von Zur MC, Stachon P, Bode C, Staudacher DL (2021) Incidence and predictors of delirium on the intensive care unit after acute myocardial infarction, insight from a retrospective registry. Catheter Cardiovasc Interv 98(6):1072–1081
Uguz F, Kayrak M, Cicek E, Kayhan F, Ari H, Altunbas G (2010) Delirium following acute myocardial infarction: incidence, clinical profiles, and predictors. Perspect Psychiatr Care 46(2):135–142
Eriksson M, Samuelsson E, Gustafson Y, Aberg T, Engstrom KG (2002) Delirium after coronary bypass surgery evaluated by the organic brain syndrome protocol. Scand Cardiovasc J 36(4):250–255
Litaker D, Locala J, Franco K, Bronson DL, Tannous Z (2001) Preoperative risk factors for postoperative delirium. Gen Hosp Psychiatry 23(2):84–89
Ljubisavljevic V, Kelly B (2003) Risk factors for development of delirium among oncology patients. Gen Hosp Psychiatry 25(5):345–352
Shiiba M, Takei M, Nakatsuru M, Bukawa H, Yokoe H, Uzawa K, Tanzawa H (2009) Clinical observations of postoperative delirium after surgery for oral carcinoma. Int J Oral Maxillofac Surg 38(6):661–665
Fong TG, Bogardus ST Jr, Daftary A, Auerbach E, Blumenfeld H, Modur S, Leo-Summers L, Seibyl J, Inouye SK (2006) Cerebral perfusion changes in older delirious patients using 99mTc HMPAO SPECT. J Gerontol A Biol Sci Med Sci 61(12):1294–1299
Haggstrom L, Welschinger R, Caplan GA (2017) Functional neuroimaging offers insights into delirium pathophysiology: a systematic review. Australas J Ageing 36(3):186–192
Oh ES, Sieber FE, Leoutsakos JM, Inouye SK, Lee HB (2016) Sex differences in hip fracture surgery: preoperative risk factors for delirium and postoperative outcomes. J Am Geriatr Soc 64(8):1616–1621
Wang H, Guo X, Zhu X, Li Y, Jia Y, Zhang Z, Yuan S, Yan F (2021) Gender differences and postoperative delirium in adult patients undergoing cardiac valve surgery. Front Cardiovasc Med 8:751421
Bellelli G, Zambon A, Volpato S, Abete P, Bianchi L, Bo M, Cherubini A, Corica F, Di Bari M, Maggio M, Manca GM, Rizzo MR, Rossi A, Landi F, Investigators GG (2018) The association between delirium and sarcopenia in older adult patients admitted to acute geriatrics units: results from the GLISTEN multicenter observational study. Clin Nutr 37(5):1498–1504
Greaves D, Psaltis PJ, Davis DHJ, Ross TJ, Ghezzi ES, Lampit A, Smith AE, Keage HAD (2020) Risk factors for delirium and cognitive decline following coronary artery bypass grafting surgery: a systematic review and meta-analysis. J Am Heart Assoc 9(22):e017275
Trzepacz PT, Franco JG, Meagher DJ, Lee Y, Kim JL, Kishi Y, Furlanetto LM, Negreiros D, Huang MC, Chen CH, Kean J, Leonard M (2018) Delirium phenotype by age and sex in a pooled data set of adult patients. J Neuropsychiatry Clin Neurosci 30(4):294–301
Nam SY, Jeon SW, Kwon YH, Kwon OK (2021) Sex difference of mortality by age and body mass index in gastric cancer. Dig Liver Dis 53(9):1185–1191
Elgendy IY, Wegermann ZK, Li S, Mahtta D, Grau-Sepulveda M, Smilowitz NR, Gulati M, Garratt KN, Wang TY, Jneid H (2022) Sex differences in management and outcomes of acute myocardial infarction patients presenting with cardiogenic shock. JACC Cardiovasc Interv 15(6):642–652
Matetic A, Shamkhani W, Rashid M, Volgman AS, Van Spall HGC, Coutinho T, Mehta LS, Sharma G, Parwani P, Mohamed MO, Mamas MA (2021) Trends of sex differences in clinical outcomes after myocardial infarction in the United States. CJC Open 3(12 Suppl):S19–S27
Suzuki M, Nishihira K, Takegami M, Honda S, Kojima S, Takayama M, Sumiyoshi T, Ogawa H, Kimura K, Yasuda S, Investigators J (2020) Clinical profiles and outcomes in the treatment of acute myocardial infarction in Japan of aging society. Heart Vessels 35(12):1681–1688
Stehli J, Martin C, Brennan A, Dinh DT, Lefkovits J, Zaman S (2019) Sex differences persist in time to presentation, revascularization, and mortality in myocardial infarction treated with percutaneous coronary intervention. J Am Heart Assoc 8(10):e012161
Deng X, Qin P, Lin Y, Tao H, Liu F, Lin X, Wang B, Bi Y (2022) The relationship between body mass index and postoperative delirium. Brain Behav 12(4):e2534
Chen H, Mo L, Hu H, Ou Y, Luo J (2021) Risk factors of postoperative delirium after cardiac surgery: a meta-analysis. J Cardiothorac Surg 16(1):113
Moerer O, Schmid A, Hofmann M, Herklotz A, Reinhart K, Werdan K, Schneider H, Burchardi H (2002) Direct costs of severe sepsis in three German intensive care units based on retrospective electronic patient record analysis of resource use. Intensive Care Med 28(10):1440–1446
Sogayar AM, Machado FR, Rea-Neto A, Dornas A, Grion CM, Lobo SM, Tura BR, Silva CL, Cal RG, Beer I, Michels V, Safi J, Kayath M, Silva E (2008) A multicentre, prospective study to evaluate costs of septic patients in Brazilian intensive care units. Pharmacoeconomics 26(5):425–434
Acknowledgements
The authors acknowledge all staff in the catheter laboratory, cardiology units, and emergency and intensive care units in Saitama Medical Center, Jichi Medical University for their technical support in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
Dr. Sakakura has received speaking honoraria from Abbott Vascular, Boston Scientific, Medtronic Cardiovascular, Terumo, OrbusNeich, Japan Lifeline, Kaneka, and NIPRO. Dr. Jinnouchi has received speaking honoraria from Abbott Vascular. Prof. Fujita has served as a consultant for Mehergen Group Holdings, Inc.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Aono-Setoguchi, H., Sakakura, K., Jinnouchi, H. et al. Factors associated with intensive care unit delirium in patients with acute myocardial infarction. Heart Vessels 38, 478–487 (2023). https://doi.org/10.1007/s00380-022-02200-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-022-02200-1