Abstract
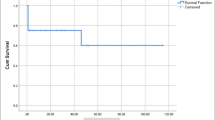
The purpose of this study is to access the outcomes of aortic bypass graft placement in children. This is a retrospective review of all children having aortic bypass graft placement for aortic arch obstruction for the first time between 1982 and 2013 at a single institution. The actuarial survival and the freedom from aortic arch reoperation were calculated and compared between the groups. Seventy consecutive children underwent aortic bypass graft placements. The median age and body weight at the operation were 14 days and 3.6 kg. There were 7 early deaths, 6 late deaths, and 7 heart transplants during the median follow-up of 10.8 years (0.0–31.5 years). The actuarial transplant free survival was 64.7 % at 20 years and the freedom from aortic arch reoperation was 50.5 % at 10 years. Between the children younger than 1 year old and older than 1 year old, there were significant differences in actuarial transplant free survival (56.4 vs. 100 % at 15 years, p = 0.0042) and in the freedom from aortic arch reoperation (18.7 vs. 100 % at 10 years, p < 0.001). The children who received aortic bypass graft larger than 16 mm in size had no aortic arch reoperation at 15 years. The aortic bypass graft placement for aortic arch obstruction can be done with low mortality and morbidity for children who can receive bypass graft larger than 16 mm in size. However, it should be avoided for the neonates and infants except selected situations.




Similar content being viewed by others
References
McCrindle BW, Tchervenkov CI, Konstantinov IE, Williams WG, Neirotti RA, Jacobs ML, Blackstone EH, Congenital Heart Surgeons Society (2005) Risk factors associated with mortality and interventions in 472 neonates with interrupted aortic arch: a Congenital Heart Surgeons Society study. J Thorac Cardiovasc Surg 129:343–350
Brown JW, Ruzmetov M, Hoyer MH, Rodefeld MD, Turrentine MW (2009) Recurrent coarctation: is surgical repair of recurrent coarctation of the aorta safe and effective? Ann Thorac Surg 88:1923–1930
Sturm JT, vanHeeckeren DW, Borkat G (1981) Surgical treatment of interrupted aortic arch in infancy with expanded polytetrafluoroethylene grafts: 2-year follow-up results. J Thorac Cardiovasc Surg 81:245–249
Shinkawa T, Jaquiss RBD, Imamura M (2012) Single institutional experience of interrupted aortic arch repair over 28 years. Interact CardioVasc Thorac Surg 14:551–555
Edie RN, Janani J, Attai LA, Malm JR, Robinson G (1975) Bypass grafts for recurrent or complex coarctations of the aorta. Ann Thorac Surg 20:558–566
Karl TR, Sano S, Brawn W, Mee RB (1992) Repair of hypoplastic or interrupted aortic arch via sternotomy. J Thorac Cardiovasc Surg 104:688–695
Connolly HM, Schaff HV, Izhar U, Dearani JA, Warnes CA, Orszulak TA (2001) Posterior pericardial ascending-to-descending aortic bypass: an alternative surgical approach for complex coarctation of the aorta. Circulation 104:I133–I137
Izhar U, Schaff HV, Mullany CJ, Daly RC, Orszulak TA (2000) Posterior pericardial approach for ascending aorta-to-descending aorta bypass through a median sternotomy. Ann Thorac Surg 70:31–37
Uppu SC, Shinkawa T, Imamura M (2012) Single institution experience with a right-sided interrupted aortic arch. Interact CardioVasc Thorac Surg 15:802–804
McKellar SH, Schaff HV, Dearani JA, Daly RC, Mullany CJ, Orszulak TA, Sundt TM 3rd, Connolly HM, Warnes CA, Puga FJ (2007) Intermediate-term results of ascending-descending posterior pericardial bypass of complex aortic coarctation. J Thorac Cardiovasc Surg 133:1504–1509
Kanter KR, Erez E, Williams WH, Tam VK (2000) Extra-anatomic aortic bypass via sternotomy for complex aortic arch stenosis in children. J Thorac Cardiovasc Surg 120:885–890
Miyazaki A, Sakaguchi H, Ohuchi H, Yasuda K, Tsujii N, Matsuoka M, Yamamoto T, Yazaki S, Tsuda E, Yamada O (2015) The clinical characteristics of sudden cardiac arrest in asymptomatic patients with congenital heart disease. Heart Vessels 30:70–80
Akintürk H, Michel-Behnke I, Valeske K, Mueller M, Thul J, Bauer J, Hagel KJ, Schranz D (2007) Hybrid transcatheter-surgical palliation: basis for univentricular or biventricular repair: the Giessen experience. Pediatr Cardiol 28:79–87
Acknowledgments
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Shinkawa, T., Chipman, C., Holloway, J. et al. Single center experience of aortic bypass graft for aortic arch obstruction in children. Heart Vessels 32, 76–82 (2017). https://doi.org/10.1007/s00380-016-0842-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-016-0842-x