Abstract
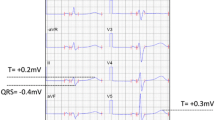
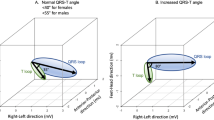
We assessed the relationship between J waves and the ventricular morphology and function using cardiac magnetic resonance imaging (MRI). The 12-lead electrocardiograms (ECGs) of 105 consecutive patients who underwent cardiac MRI were reviewed, and those with signs of arrhythmogenic right ventricular cardiomyopathy, complete left bundle branch block, complete right bundle branch block, or chronic atrial fibrillation, where the J wave is difficult to distinguish, were excluded. The ECGs of the remaining 68 patients were analyzed for the presence of J waves. Ventricular morphologic abnormalities were identified on MRI, based on the largest short-axis diameter in the right and left ventricles (d-RVmax/d-LVmax), the area (a-RVmax/a-LVmax), and the ratio RV/LVmax. The percentage contraction of the RV (PC-RV) was used as a measure of ventricular function. Thirty-two patients (47.0 %) had J waves defined as QRS-ST junction elevation >0.1 mV from baseline in the inferior/lateral leads (J group; 56 ± 15 years; 19 males). Thirty-six patients (53.0 %) did not present J waves (NJ group; 58 ± 15 years; 27 males). The d-RVmax and a-RVmax in the J group were larger than those in the NJ group (41 ± 5.2 vs 36 ± 6.6 mm, P = 0.002 and 14 ± 2.9 vs 12 ± 3.4 cm2, P = 0.022, respectively). The RV/LVmax ratio in the J group was larger than that in the NJ group (0.83 ± 0.15 vs 0.68 ± 0.15, P < 0.001). The PC-RV in the J group was smaller than that in the NJ group (0.28 ± 0.14 vs 0.36 ± 0.15, P = 0.013). J-wave amplitude was correlated positively with d-RVmax (P = 0.010) and negatively with PC-RV (P = 0.005). These results suggested that J waves are associated with right ventricular morphologic and functional abnormalities.









Similar content being viewed by others
References
Haissaguerre M, Derval N, Sacher F, Jesel L, Deisenhofer I, de Roy L, Pasquie JL, Nogami A, Babuty D, Yli-Mayry S, De Chillou C, Scanu P, Mabo P, Matsuo S, Probst V, Le Scouarnec S, Defaye P, Schlaepfer J, Rostock T, Lacroix D, Lamaison D, Lavergne T, Aizawa Y, Englund A, Anselme F, O’Neill M, Hocini M, Lim KT, Knecht S, Veenhuyzen GD, Bordachar P, Chauvin M, Jais P, Coureau G, Chene G, Klein GJ, Clementy J (2008) Sudden cardiac arrest associated with early repolarization. N Engl J Med 358:2016–2023
Haruta D, Matsuo K, Tsuneto A, Ichimaru S, Hida A, Sera N, Imaizumi M, Nakashima E, Maemura K, Akahoshi M (2011) Incidence and prognostic value of early repolarization pattern in the 12-lead electrocardiogram. Circulation 123:2931–2937
Olson KA, Viera AJ, Soliman EZ, Crow RS, Rosamond WD (2011) Long-term prognosis associated with J-point elevation in a large middle-aged biracial cohort: the ARIC study. Eur Heart J 32:3098–3106
Rosso R, Glikson E, Belhassen B, Katz A, Halkin A, Steinvil A, Viskin S (2011) Distinguishing “benign” from “malignant early repolarization”: the value of the ST-segment morphology. Heart Rhythm 9:225–229
Tikkanen JT, Anttonen O, Junttila MJ, Aro AL, Kerola T, Rissanen HA, Reunanen A, Huikuri HV (2009) Long-term outcome associated with early repolarization on electrocardiography. N Engl J Med 361:2529–2537
Haissaguerre M, Sacher F, Nogami A, Komiya N, Bernard A, Probst V, Yli-Mayry S, Defaye P, Aizawa Y, Frank R, Mantovan R, Cappato R, Wolpert C, Leenhardt A, de Roy L, Heidbuchel H, Deisenhofer I, Arentz T, Pasquie JL, Weerasooriya R, Hocini M, Jais P, Derval N, Bordachar P, Clementy J (2009) Characteristics of recurrent ventricular fibrillation associated with inferolateral early repolarization role of drug therapy. J Am Coll Cardiol 53:612–619
Rosso R, Adler A, Halkin A, Viskin S (2011) Risk of sudden death among young individuals with J waves and early repolarization: putting the evidence into perspective. Heart Rhythm 8:923–929
Rosso R, Kogan E, Belhassen B, Rozovski U, Scheinman MM, Zeltser D, Halkin A, Steinvil A, Heller K, Glikson M, Katz A, Viskin S (2008) J-point elevation in survivors of primary ventricular fibrillation and matched control subjects: incidence and clinical significance. J Am Coll Cardiol 52:1231–1238
Brugada P, Brugada J (1992) Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report. J Am Coll Cardiol 20:1391–1396
Kalla H, Yan GX, Marinchak R (2000) Ventricular fibrillation in a patient with prominent J (Osborn) waves and ST segment elevation in the inferior electrocardiographic leads: a Brugada syndrome variant? J Cardiovasc Electrophysiol 11:95–98
Kamakura S, Ohe T, Nakazawa K, Aizawa Y, Shimizu A, Horie M, Ogawa S, Okumura K, Tsuchihashi K, Sugi K, Makita N, Hagiwara N, Inoue H, Atarashi H, Aihara N, Shimizu W, Kurita T, Suyama K, Noda T, Satomi K, Okamura H, Tomoike H (2009) Long-term prognosis of probands with Brugada-pattern ST-elevation in leads V1–V3. Circ Arrhythm Electrophysiol 2:495–503
Sarkozy A, Chierchia GB, Paparella G, Boussy T, De Asmundis C, Roos M, Henkens S, Kaufman L, Buyl R, Brugada R, Brugada J, Brugada P (2009) Inferior and lateral electrocardiographic repolarization abnormalities in Brugada syndrome. Circ Arrhythm Electrophysiol 2:154–161
Gussak I, Antzelevitch C (2000) Early repolarization syndrome: clinical characteristics and possible cellular and ionic mechanisms. J Electrocardiol 33:299–309
Mehta M, Jain AC, Mehta A (1999) Early repolarization. Clin Cardiol 22:59–65
Yan GX, Antzelevitch C (1996) Cellular basis for the electrocardiographic J wave. Circulation 93:372–379
Watanabe H, Nogami A, Ohkubo K, Kawata H, Hayashi Y, Ishikawa T, Makiyama T, Nagao S, Yagihara N, Takehara N, Kawamura Y, Sato A, Okamura K, Hosaka Y, Sato M, Fukae S, Chinushi M, Oda H, Okabe M, Kimura A, Maemura K, Watanabe I, Kamakura S, Horie M, Aizawa Y, Shimizu W, Makita N (2011) Electrocardiographic characteristics and SCN5A mutations in idiopathic ventricular fibrillation associated with early repolarization. Circ Arrhythm Electrophysiol 4:874–881
Postema PG, van Dessel PF, Kors JA, Linnenbank AC, van Herpen G, Ritsema van Eck HJ, van Geloven N, de Bakker JM, Wilde AA, Tan HL (2010) Local depolarization abnormalities are the dominant pathophysiologic mechanism for type 1 electrocardiogram in Brugada syndrome a study of electrocardiograms, vectorcardiograms, and body surface potential maps during ajmaline provocation. J Am Coll Cardiol 55:789–797
Papavassiliu T, Wolpert C, Fluchter S, Schimpf R, Neff W, Haase KK, Duber C, Borggrefe M (2004) Magnetic resonance imaging findings in patients with Brugada syndrome. J Cardiovasc Electrophysiol 15:1133–1138
Takagi M, Aihara N, Kuribayashi S, Taguchi A, Kurita T, Suyama K, Kamakura S, Takamiya M (2003) Abnormal response to sodium channel blockers in patients with Brugada syndrome: augmented localised wall motion abnormalities in the right ventricular outflow tract region detected by electron beam computed tomography. Heart 89:169–174
Takagi M, Aihara N, Kuribayashi S, Taguchi A, Shimizu W, Kurita T, Suyama K, Kamakura S, Hamada S, Takamiya M (2001) Localized right ventricular morphological abnormalities detected by electron-beam computed tomography represent arrhythmogenic substrates in patients with the Brugada syndrome. Eur Heart J 22:1032–1041
Catalano O, Antonaci S, Moro G, Mussida M, Frascaroli M, Baldi M, Cobelli F, Baiardi P, Nastoli J, Bloise R, Monteforte N, Napolitano C, Priori SG (2009) Magnetic resonance investigations in Brugada syndrome reveal unexpectedly high rate of structural abnormalities. Eur Heart J 30:2241–2248
Sato Y, Kato K, Hashimoto M, Akiyama H, Matsumoto N, Takase H, Ogawa K, Sakamaki T, Yagi H, Kanmatsuse K (1996) Localized right ventricular structural abnormalities in patients with idiopathic ventricular fibrillation: magnetic resonance imaging study. Heart Vessels 11:100–103
Antzelevitch C, Yan GX (2010) J wave syndromes. Heart Rhythm 7:549–558
Franzen E, Mangold S, Erz G, Claussen CD, Niess AM, Kramer U, Burgstahler C (2012) Comparison of morphological and functional adaptations of the heart in highly trained triathletes and long-distance runners using cardiac magnetic resonance imaging. Heart Vessels. doi:10.1007/s00380-012-0289-7
Lee N, Das A, Banerjee RK, Gottliebson WM (2013) Comparison of stroke work between repaired tetralogy of Fallot and normal right ventricular physiologies. Heart Vessels 28:76–85
Antzelevitch C, Brugada P, Borggrefe M, Brugada J, Brugada R, Corrado D, Gussak I, LeMarec H, Nademanee K, Perez Riera AR, Shimizu W, Schulze-Bahr E, Tan H, Wilde A (2005) Brugada syndrome: report of the second consensus conference: endorsed by the Heart Rhythm Society and the European Heart Rhythm Association. Circulation 111:659–670
Morita H, Kusano KF, Miura D, Nagase S, Nakamura K, Morita ST, Ohe T, Zipes DP, Wu J (2008) Fragmented QRS as a marker of conduction abnormality and a predictor of prognosis of Brugada syndrome. Circulation 118:1697–1704
Lambiase PD, Ahmed AK, Ciaccio EJ, Brugada R, Lizotte E, Chaubey S, Ben-Simon R, Chow AW, Lowe MD, McKenna WJ (2009) High-density substrate mapping in Brugada syndrome: combined role of conduction and repolarization heterogeneities in arrhythmogenesis. Circulation 120:106–117
Abe A, Ikeda T, Tsukada T, Ishiguro H, Miwa Y, Miyakoshi M, Mera H, Yusu S, Yoshino H (2010) Circadian variation of late potentials in idiopathic ventricular fibrillation associated with J waves: insights into alternative pathophysiology and risk stratification. Heart Rhythm 7:675–682
Aizawa Y, Sato A, Watanabe H, Chinushi M, Furushima H, Horie M, Kaneko Y, Imaizumi T, Okubo K, Watanabe I, Shinozaki T, Fukuda K, Joo K, Haissaguerre M (2012) Dynamicity of the J-wave in idiopathic ventricular fibrillation with a special reference to pause-dependent augmentation of the J-wave. J Am Coll Cardiol 59:1948–1953
Aizawa Y, Tamura M, Chinushi M, Naitoh N, Uchiyama H, Kusano Y, Hosono H, Shibata A (1993) Idiopathic ventricular fibrillation and bradycardia-dependent intraventricular block. Am Heart J 126:1473–1474
Maruyama M, Atarashi H, Ino T, Kishida H (2002) Osborn waves associated with ventricular fibrillation in a patient with vasospastic angina. J Cardiovasc Electrophysiol 13:486–489
Sahara M, Sagara K, Yamashita T, Abe T, Kirigaya H, Nakada M, Iinuma H, Fu LT, Watanabe H (2002) J wave and ST segment elevation in the inferior leads: a latent type of variant Brugada syndrome? Jpn Heart J 43:55–60
McKenna WJ, Thiene G, Nava A, Fontaliran F, Blomstrom-Lundqvist C, Fontaine G, Camerini F (1994) Diagnosis of arrhythmogenic right ventricular dysplasia/cardiomyopathy. Task Force of the Working Group Myocardial and Pericardial Disease of the European Society of Cardiology and of the Scientific Council on Cardiomyopathies of the International Society and Federation of Cardiology. Br Heart J 71:215–218
Acknowledgments
We thank Dr Tetsuo Nomiyama and Dr Teruomi Tsukahara, of the Department of Public Health, Shinshu University, for their evaluation of the systematic bias by the Bland and Altman method.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Takeuchi, T., Tomita, T., Yoshie, K. et al. Electrocardiographic J waves are associated with right ventricular morphology and function: evaluation by cardiac magnetic resonance imaging. Heart Vessels 30, 98–107 (2015). https://doi.org/10.1007/s00380-013-0439-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-013-0439-6