Abstract
Purpose
We sought to characterize the adjusted outcomes of GreenLight photoselective vaporization of the prostate (PVP) in high-medical-risk (HMR) patients using data from the largest international database.
Methods
Data were obtained from the Global GreenLight Group (GGG) database which pools data of eight high-volume, experienced surgeons, from a total of seven international centers. Eligible study participants underwent GreenLight PVP using the XPS-180 W system between 2011 and 2019. HMR patients were defined as patients with ASA III or greater and were compared to non-HMR patients. Analyses were adjusted for patient age and prostate volume.
Results
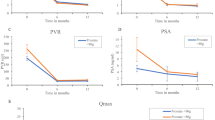
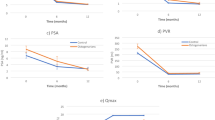
In the HMR group, patients on average were older and had smaller prostates than the non-HMR control group. Compared to non-HMR patients, transfusions occurred more frequently (2.6% vs. 0.14%, p < 0.01) and the odds of readmission were elevated [OR 2.0, (95% CI 1.4–2.8, p < 0.01)] among HMR patients. Twelve months postoperatively, HMR patients experience greater improvement in QoL than the control group [+ 0.54 (95% CI 0.07–1.0, p = 0.02)]. PVR also decreased 93.1 ml more in HMR than in non-HMR patients after 12 months (95% CI 33.6–152.6, p < 0.01).
Conclusion
We found that GreenLight PVP is safe and effective in improving functional outcomes in higher-risk patients with severe systemic disease compared to their lower-risk counterparts. Though absolute risks remain low, GreenLight PVP is associated with higher odds of transfusion and readmission in the high-risk cohort. The findings of our study reaffirm current guidelines that propose PVP as a viable treatment option for HMR patients.

Similar content being viewed by others
References
Berry SJ, Coffey DS, Walsh PC, Ewing LL (1984) The development of human benign prostatic hyperplasia with age. J Urol 132(3):474–479. https://doi.org/10.1016/S0022-5347(17)49698-4
Hutchison A, Farmer R, Verhamme K, Berges R, Navarrete RV (2007) The efficacy of drugs for the treatment of LUTS/BPH, a study in 6 European countries. Eur Urol 51(1):207–216. https://doi.org/10.1016/J.EURURO.2006.06.012
Welliver C, Essa A (2016) Sexual side effects of medical and surgical benign prostatic hyperplasia treatments. Urol Clin 43(3):393–404. https://doi.org/10.1016/J.UCL.2016.04.010
Lusty A, Siemens DR, Tohidi M, Whitehead M, Tranmer J, Nickel JC (2021) Cardiac failure associated with medical therapy of benign prostatic hyperplasia: a population based study. J Urol 205(5):1430–1437. https://doi.org/10.1097/JU.0000000000001561
Cindolo L, Pirozzi L, Fanizza C et al (2015) Drug adherence and clinical outcomes for patients under pharmacological therapy for lower urinary tract symptoms related to benign prostatic hyperplasia: population-based cohort study. Eur Urol 68(3):418–425. https://doi.org/10.1016/j.eururo.2014.11.006
Manfredi C, Arcaniolo D, Spatafora P et al (2021) Emerging minimally invasive transurethral treatments for benign prostatic hyperplasia: a systematic review with meta-analysis of functional outcomes and description of complications. Minerva Urol Nephrol. https://doi.org/10.23736/s2724-6051.21.04530-4
LaRussa S, Pantuck M, Vanden Burg RW, Gaffney CD, Askin G, McClure T (2021) Symptomatic improvement of lower urinary tract symptoms of benign prostatic hyperplasia: a comparative systematic review and meta-analysis of four different minimally invasive therapies. J Vasc Interv Radiol Published online. https://doi.org/10.1016/j.jvir.2021.06.019
Marchioni M, Cindolo L, Di NM et al (2019) Prostatic diseases and male voiding dysfunction major acute cardiovascular events after transurethral prostate surgery: a population-based analysis. Urology 131:196–203. https://doi.org/10.1016/j.urology.2019.05.014
Meskawi M, Hueber P-A, Valdivieso R et al (2019) Complications and functional outcomes of high-risk patient with cardiovascular disease on antithrombotic medication treated with the 532-nm-laser photo-vaporization Greenlight XPS-180 W for benign prostate hyperplasia. World J Urol 37:1671–1678. https://doi.org/10.1007/s00345-018-2560-8
Lee DJ, Rieken M, Halpern J et al (2016) Laser vaporization of the prostate with the 180-W XPS-greenlight laser in patients with ongoing platelet aggregation inhibition and oral anticoagulation. Urology 91:167–173. https://doi.org/10.1016/j.urology.2016.01.021
Rajih E, Tholomier C, Hueber PA et al (2017) Evaluation of surgical outcomes with photoselective GreenLight XPS laser vaporization of the prostate in high medical risk men with benign prostatic enlargement: a multicenter study. J Endourol 31:686–693. https://doi.org/10.1089/end.2016.0782
Bouhadana D, Nguyen D-D, Zhang X et al (2021) Safety and efficacy of TURP vs laser prostatectomy for the treatment of benign prostatic hyperplasia in multi-morbid and elderly individuals aged ≥ 75. World J Urol. https://doi.org/10.1007/S00345-021-03779-2
Law KW, Tholomier C, Nguyen D-D et al (2021) Global greenlight group: largest international Greenlight experience for benign prostatic hyperplasia to assess efficacy and safety. World J Urol. https://doi.org/10.1007/s00345-021-03688-4
Doyle DJ, Garmon EH (2021) American Society of Anesthesiologists Classification (ASA Class). StatPearls Publishing; 2018. Accessed July 28 https://www.ncbi.nlm.nih.gov/books/NBK441940/
Haeuser L, Herzog P, Ayub A et al (2021) Comparison of comorbidity indices for prediction of morbidity and mortality after major surgical procedures. Am J Surg. https://doi.org/10.1016/j.amjsurg.2021.04.007
LaBossiere JR, Wallis CJD, Herschorn S, Carr L, Saskin R, Nam R (2020) Surgical management of benign prostatic obstruction: 20-year population-level trends. Can Urol Assoc J 14(8):552–557. https://doi.org/10.5489/CUAJ.6224
Piotrowicz G, Syryło T, Jedynak R, Zieliński H (2018) Efficacy and safety of photoselective vaporization of the prostate with 120 W 532 nm laser in patients with benign prostatic hyperplasia on anticoagulation or antiplatelet therapy: observations on long-term outcomes. Photomed Laser Surg 36(5):273–283. https://doi.org/10.1089/pho.2017.4367
Eken A, Soyupak B (2018) Safety and efficacy of photoselective vaporization of the prostate using the 180-W GreenLight XPS laser system in patients taking oral anticoagulants. J Int Med Res 46(3):1230–1237. https://doi.org/10.1177/0300060517747489
Parsons J, Dahm P, Köhler T et al (2020) Surgical management of lower urinary tract symptoms attributed to benign prostatic hyperplasia: AUA guideline amendment. J Urol 2020:799–804
Gravas S, Cornu J, Gacci M, et al. EAU Guidelines Edn presented at the EAU Annual Congress Milan 2021. EAU Guidel Off.
Barco-Castillo C, Plata M, Zuluaga L et al (2020) Functional outcomes and safety of GreenLight photovaporization of the prostate in the high-risk patient with lower urinary tract symptoms due to benign prostatic enlargement. Neurourol Urodyn 39(1):303–309. https://doi.org/10.1002/nau.24195
Sankar A, Johnson SR, Beattie WS et al (2014) Reliability of the American Society of Anesthesiologists physical status scale in clinical practice. Br J Anaesth 113(3):424–432. https://doi.org/10.1093/bja/aeu100
Funding
No funding or financial support was received for this study.
Author information
Authors and Affiliations
Contributions
DDN: protocol/project development, data analysis, manuscript writing. CD: protocol/project development, data analysis, manuscript writing. KL: data collection, manuscript writing/editing. NB: manuscript editing. DSE: manuscript editing. BC: data collection, manuscript editing. FB: data collection, manuscript editing. LC: data collection, manuscript editing. GF: data collection, manuscript editing. CV-L: data collection, manuscript editing. TB-B: data collection, manuscript editing. EFB: data collection, manuscript editing. HC: data collection, manuscript editing. MR: data collection, manuscript editing. ER: data collection, manuscript editing. VM: data collection, manuscript editing. KCZ: protocol/project development, data collection, manuscript editing.
Corresponding author
Ethics declarations
Conflict of interest
Consultants and proctors for Boston Scientific for Greenlight: Zorn, Elterman, Misrai, Rijo, Cash, Chughtai. Surgical tutors for Greenlight Xcelerated Performance System and received honoraria for their tutorship: Ferrari, Cindolo. Investigators and consultants for PROCEPT BioRobotics: Misrai, Borelli-Bovo, Bhojani, Zorn. All other authors do not have any relevant conflicts of interest. Furthered by Dr. Kevin Zorn INC.
Research involving human participants and/or animals
This is a study involving retrospective review of participants. IRB approval has been obtained.
Informed consent
The informed consent has been waived per IRB.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nguyen, DD., Deyirmendjian, C., Law, K. et al. GreenLight photovaporization of the prostate in high-medical-risk patients: an analysis of the Global GreenLight Group (GGG) database. World J Urol 40, 1755–1762 (2022). https://doi.org/10.1007/s00345-022-03986-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-022-03986-5