Abstract
Purpose
The primary aim of this study to comparison of reusable and disposable flexible ureterorenoscope (fURS) efficiency in lower pole renal stone disease management. In addition, the secondary goal of this study was to evaluate the factors affecting stone-free rates (SFR) in lower pole stones.
Materials and methods
A prospective case–control study utilizing data from 122 consecutive ureteroscopic cases. The patients were divided into two groups according to the ureterorenoscope employed in the surgical intervention as disposable fURS (Group1, n:52) and reusable fURS (Group 2, n:70). Demographic characteristics, stone size, infundibulopelvic angle (IPA), SFR, hospitalization time, intraoperative complication rate (CR), operative time, preoperative or postoperative JJ stenting, and postoperative CR were analyzed.
Results
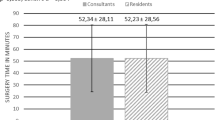
There was no statistical difference between the demographic and renal stone-related data between the groups. Likewise, no difference is observed in term of intraoperative and postoperative outcomes such as fluoroscopy time, CR, and hospitalization time between the groups. Although SFR was higher in the disposable fURS group, there was no difference statistically. However, the operative time was longer in reusable fURS Group (47.02 ± 9.91 min in Group 1, and it was 57.97 ± 14.28 in Group 2) (p: 0.001). The multivariate regression analysis result to evaluate the factors of effect to operative time; the use of disposable fURS was associated with a 10.95-min decrease in procedure duration (p < 0.001).
Conclusions
Disposable fURS and reusable fURS have similar clinical efficiency and complication rates in the treatment of lower calyceal stones with RIRS. Nevertheless, disposable fURS is a useful treatment option for increased stone volume due to the advantages such as shorter operative time.


Similar content being viewed by others
Availability of data and material
Data are available on request.
References
Türk C, Petřík A, Sarica K, Seitz C, Skolarikos A, Straub M et al (2016) EAU guidelines on interventional treatment for urolithiasis. EurUrol 69(3):475–482
Doizi S, Traxer O (2018) Flexible ureteroscopy: technique, tips and tricks. Urolithiasis 46(1):47–58
Elbahnasy AM, Clayman RV, Shalhav AL, Hoenig DM, Chandhoke P, Lingeman JE et al (1998) Lower-pole caliceal stone clearance after shockwave lithotripsy, percutaneous nephrolithotomy, and flexible ureteroscopy: impact of radiographic spatial anatomy. J Endourol 12(2):113–119
Fan J, Zhang T, Zhu W, Gurioli A, Ketegwe IR, Zeng G (2019) The role of super-mini percutaneous nephrolithotomy (SMP) in the treatment of symptomatic lower pole renal stones (LPSs) after the failure of shockwave lithotripsy (SWL) or retrograde intrarenal surgery (RIRS). Urolithiasis 47(3):297–301
Karim SS, Hanna L, Geraghty R, Somani BK (2019) Role of pelvicalyceal anatomy in the outcomes of retrograde intrarenal surgery (RIRS) for lower pole stones: outcomes with a systematic review of literature. Urolithiasis 48(3):263–270
Salvadó JA, Cabello JM, Moreno S, Cabello R, Olivares R, Velasco A (2019) Endoscopic treatment of lower pole stones: is a disposable ureteroscope preferable? Results of a prospective case-control study. Cent Eur J Urol 72(3):280
Davis N, Quinlan M, Browne C, Bhatt N, Manecksha RP, D’Arcy F et al (2018) Single-use flexible ureteropyeloscopy: a systematic review. World J Urol 36(4):529–536
Mager R, Kurosch M, Höfner T, Frees S, Haferkamp A, Neisius A (2018) Clinical outcomes and costs of reusable and single-use flexible ureterorenoscopes: a prospective cohort study. Urolithiasis 46(6):587–593
Ozimek T, Schneider MH, Hupe MC, Wiessmeyer JR, Cordes J, Chlosta PL et al (2017) Retrospective cost analysis of a single-center reusable flexible ureterorenoscopy program: a comparative cost simulation of disposable fURS as an alternative. J Endourol 31(12):1226–1230
Doizi S, Kamphuis G, Giusti G, Andreassen KH, Knoll T, Osther PJ et al (2017) First clinical evaluation of a new single-use flexible ureteroscope (LithoVueTM): a European prospective multicentric feasibility study. World J Urol 35(5):809–818
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205
Donaldson JF, Lardas M, Scrimgeour D, Stewart F, MacLennan S, Lam TB et al (2015) Systematic review and meta-analysis of the clinical effectiveness of shock wave lithotripsy, retrograde intrarenal surgery, and percutaneous nephrolithotomy for lower-pole renal stones. EurUrol 67(4):612–616
Junbo L, Yugen L, Guo J, Jing H, Ruichao Y, Tao W (2019) Retrograde intrarenal surgery vs. percutaneous nephrolithotomy vs. extracorporeal shock wave lithotripsy for lower pole renal stones 10–20 mm: a meta-analysis and systematic review. Urol J. 16(2):97–106
Singh BP, Prakash J, Sankhwar SN, Dhakad U, Sankhwar PL, Goel A et al (2014) Retrograde intrarenal surgery vs extracorporeal shock wave lithotripsy for intermediate size inferior pole calculi: a prospective assessment of objective and subjective outcomes. Urology 83(5):1016–1022
Jessen JP, Honeck P, Knoll T, Wendt-Nordahl G (2014) Flexible ureterorenoscopy for lower pole stones: influence of the collecting system’s anatomy. J Endourol 28(2):146–151
Knudsen B, Miyaoka R, Shah K, Holden T, Turk TM, Pedro RN et al (2010) Durability of the next-generation flexible fiberopticureteroscopes: a randomized prospective multi-institutional clinical trial. Urology 75(3):534–538
Somani BK, Al-Qahtani SM, de Medina SDG, Traxer O (2013) Outcomes of flexible ureterorenoscopy and laser fragmentation for renal stones: comparison between digital and conventional ureteroscope. Urology 82(5):1017–1019
Tosoian JJ, Ludwig W, Sopko N, Mullins JK, Matlaga BR (2015) The effect of repair costs on the profitability of a ureteroscopy program. J Endourol 29(4):406–409
Legemate JD, Kamphuis GM, Freund JE, Baard J, Zanetti SP, Catellani M et al (2019) Durability of flexible ureteroscopes: a prospective evaluation of longevity, the factors that affect it, and damage mechanisms. Euro Urol focus 5(6):1105–1111
Usawachintachit M, Isaacson DS, Taguchi K, Tzou DT, Hsi RS, Sherer BA et al (2017) A prospective case–control study comparing LithoVue, a single-use, flexible disposable ureteroscope, with flexible, reusable fiber-optic ureteroscopes. J Endourol 31(5):468–475
Martin CJ, McAdams SB, Abdul-Muhsin H, Lim VM, Nunez-Nateras R, Tyson MD et al (2017) The economic implications of a reusable flexible digital ureteroscope: a cost-benefit analysis. J Urol 197(3):730–735
Salvadó JA, Olivares R, Cabello JM, Cabello R, Moreno S, Pfeifer J et al (2018) Retrograde intrarenal surgery using the single–use flexible ureteroscopeUscope 3022 (PusenTM): evaluation of clinical results. Cent Eur J Urol 71(2):202
Deininger S, Haberstock L, Kruck S, Neumann E, da Costa IA, Todenhöfer T et al (2018) Single-use versus reusable ureterorenoscopes for retrograde intrarenal surgery (RIRS): systematic comparative analysis of physical and optical properties in three different devices. World J Urol 36(12):2059–2063
Traxer O, Thomas A (2013) Prospective evaluation and classification of ureteral wall injuries resulting from insertion of a ureteral access sheath during retrograde intrarenal surgery. J Urol 189(2):580–584
Donaldson JF, Ruhayel Y, Skolarikos A, MacLennan S, Yuan Y, Shepherd R et al (2019) Treatment of bladder stones in adults and children: a systematic review and meta-analysis on behalf of the European Association of Urology Urolithiasis Guideline Panel. EurUrol 76(3):352–367
Miernik A, Wilhelm K, Ardelt PU, Adams F, Kuehhas FE, Schoenthaler M (2012) Standardized flexible ureteroscopic technique to improve stone-free rates. Urology 80(6):1198–1202
Lildal SK, Sørensen FB, Andreassen KH, Christiansen FE, Jung H, Pedersen MR et al (2017) Histopathological correlations to ureteral lesions visualized during ureteroscopy. World J Urol 35(10):1489–1496
De Coninck V, Keller EX, Rodríguez-Monsalve M, Audouin M, Doizi S, Traxer O (2018) Systematic review of ureteral access sheaths: facts and myths. BJU Int 122(6):959–969
Carlos EC, Li J, Young BJ, Radvak D, Wollin DA, Winship BB et al (2019) Let’s get to the point: comparing insertion characteristics and scope damage of flat-tip and ball-tip holmium laser fibers. J Endourol 33(1):22–26
Enikeev D, Shariat SF, Taratkin M, Glybochko P (2020) The changing role of lasers in urologic surgery. CurrOpinUrol 30(1):24–29
Dymov A, Rapoport L, Enikeev D, Tsarichenko D, Sorokin N, Proskura A et al (2019) Prospective clinical study on superpulse thulium fiber laser: Initial analysis of optimal laser settings. EurUrolSuppl 18(1):e500
Aldoukhi AH, Black KM, Hall TL, Roberts WW, Ghani KR (2020) Frequency threshold for ablation during holmium laser lithotripsy: how high can you go? J Endourol 34(10):1075–1081
Funding
The authors declare that this work has not received any funding.
Author information
Authors and Affiliations
Contributions
YEG: Protocol/project development; data collection or management; manuscript writing/editing; critical revision of the manuscript; supervision; approval of the final manuscript. MSO: Protocol/project development; data collection or management; data analysis; manuscript writing/editing; critical revision of the manuscript; supervision; approval of the final manuscript. MTK: data collection or management; manuscript writing/editing; critical revision of the manuscript; administrative, technical, or material support; approval of the final manuscript. HHT: data collection or management; manuscript writing/editing; critical revision of the manuscript; administrative, technical, or material support; approval of the final manuscript. EG: data collection or management; manuscript writing/editing; critical revision of the manuscript; administrative, technical, or material support; and approval of the final manuscript. AA: data collection or management; manuscript writing/editing; critical revision of the manuscript; administrative, technical, or material support; approval of the final manuscript. MGS: protocol/project development; data collection or management; data analysis; manuscript writing/editing; critical revision of the manuscript; approval of the final manuscript. GK: protocol/project development; data collection or management; data analysis; manuscript writing/editing; critical revision of the manuscript; approval of the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval and informed consent
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The analysis and data collection were performed following the written informed consent was obtained from all patients. The institutional human research ethics committee approved the protocol enumareted as 2020/2657 (Necmettin Erbakan University, Meram Medical Faculty Ethics Committee).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Göger, Y.E., Özkent, M.S., Kılınç, M.T. et al. Efficiency of retrograde intrarenal surgery in lower pole stones: disposable flexible ureterorenoscope or reusable flexible ureterorenoscope?. World J Urol 39, 3643–3650 (2021). https://doi.org/10.1007/s00345-021-03656-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-021-03656-y