Abstract
Purpose
Surgical simulation and 3D printing have both been gaining traction exclusively over the past decade, and now have started to appear simultaneously in current research. The opinion that surgical simulation should be part of surgery curricula is becoming ever more apparent. In this review, we highlight and briefly examine the 3D printing workflow, and each facet of the current body of literature using this technology in the augmentation of surgical training, in addition to the challenges currently faced.
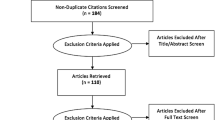
Methods
A broad literature search was conducted pertaining to the utilisation of 3D printing in urology, aiming to sample the majority of use-cases of this fairly novel technology. The 3D printing workflow, current use-cases of 3D printing as applied to urological training, and challenges faced have been described.
Results
A respectable number of surgical use-cases utilising 3D printing technology in their development were identified, including but not limited to percutaneous nephrolithotomy, partial nephrectomy, renal transplantation, laparoscopic pyeloplasty, prostate brachytherapy, transurethral resection of bladder tumours, urethrovesical anastomosis simulation devices, in addition to laparoscopic trainers and robotic surgery phantoms.
Conclusion
Over the last decade, urology has taken this cutting-edge technology in its stride; flaunting its efficacy in the augmentation of a number of procedural training applications. The number of use cases for this technology is only expected to rise as its virtues are demonstrated, the ease of use and availability of 3D printing units advances, and costs abated.

Similar content being viewed by others
References
Tan SSY, Sarker SK (2011) Simulation in surgery: a review. Scott Med J 56(2):104–109
Preece R (2015) The current role of simulation in urological training. Cent Eur J Urol 68(2). https://ceju.online/journal/2015/educational-models-simulation-training-urology-522.php
de Montbrun S, MacRae H (2012) Simulation in surgical education. Clin Colon Rectal Surg 25(03):156–165
Aydin A, Shafi AMA, Shamim Khan M, Dasgupta P, Ahmed K (2016) Current status of simulation and training models in urological surgery: a systematic review. J Urol 196(2):312–320
Turney BW (2014) A new model with an anatomically accurate human renal collecting system for training in fluoroscopy-guided percutaneous nephrolithotomy access. J Endourol 28(3):360–363
Christiansen AR, Shorti RM, Smith CD, Prows WC, Bishoff JT (2018) Intraoperative utilization of advanced imaging modalities in a complex kidney stone case: a pilot case study. World J Urol 36(5):733–743
Adams F, Qiu T, Mark A, Fritz B, Kramer L, Schlager D et al (2017) Soft 3D-printed phantom of the human kidney with collecting system. Ann Biomed Eng 45(4):963–972
Ghazi A, Campbell T, Melnyk R, Feng C, Andrusco A, Stone J et al (2017) Validation of a full-immersion simulation platform for percutaneous nephrolithotomy using three-dimensional printing technology. J Endourol 31(12):1314–1320
Bruyère F, Leroux C, Brunereau L, Lermusiaux P (2008) Rapid prototyping model for percutaneous nephrolithotomy training. J Endourol 2(1):91–96
Stone J, Bonamico R, Erturk E, Ghazi A (2017) PD41-01 improved surgical outcomes after preoperative rehearsal using 3D printed patient specific simulation for percutaneous nephrolithotomy (PCNL). J Urol 197(4):e807
Antonelli JA, Beardsley H, Faddegon S, Morgan MSC, Gahan JC, Pearle MS et al (2016) A novel device to prevent stone fragment migration during percutaneous lithotripsy: results from an in vitro kidney model. J Endourol 30(11):1239–1243
Veneziano D, Smith A, Reihsen T, Speich J, Sweet RM (2015) The SimPORTAL Fluoro-Less C-Arm Trainer: an innovative device for percutaneous kidney access. J Endourol 29(2):240–245
Knoedler M, Feibus AH, Lange A, Maddox MM, Ledet E, Thomas R et al (2015) Individualized physical 3-Dimensional kidney tumor models constructed from 3-Dimensional printers result in improved trainee anatomic understanding. Urology 85(6):1257–1262
Okada A, Tozawa K, Kobayashi D, Mizuno K, Umemoto Y, Kawai N et al (2016) MP34-02 printed three-dimensional elastic organ model to increase robot-assisted laparoscopic partial nephrectomy performance. J Urol 195(4):e471
Ng TL, Li CF, Kan WM, Ng CM, Kan CF, Ngai HY et al (2017) 3D printing of kidney models for urological surgeries: our initial experience. Int J Urol 24(Suppl 1):45
von Rundstedt F-C, Scovell JM, Agrawal S, Zaneveld J, Link RE (2017) Utility of patient-specific silicone renal models for planning and rehearsal of complex tumour resections prior to robot-assisted laparoscopic partial nephrectomy. BJU Int 119(4):598–604
Golab A, Smektala T, Kaczmarek K, Stamirowski R, Hrab M, Slojewski M (2017) Laparoscopic partial nephrectomy supported by training involving personalized silicone replica poured in three-dimensional printed casting mold. J Laparoendosc Adv Surg Tech 27(4):420–422
Stone J, Melnyk R, Wu G, Rashid H, Joseph J, Ghazi A (2017) V4–01 patient specific rehearsal using 3D printing for complex partial nephrectomy cases. J Urol 197(4):e375
Maddox MM, Feibus A, Liu J, Wang J, Thomas R, Silberstein JL (2018) 3D-printed soft-tissue physical models of renal malignancies for individualized surgical simulation: a feasibility study. J Robot Surg 12(1):27–33
Shiga Y, Sugimoto M, Iwabuchi T, Kawano Y, Oiwa Y, Watanabe H et al (2014) 1124 Benefit of three-dimensional printing in robotic laparoscopic renal surgery: tangible surgical navigation using a patient-based three-dimensional printed kidney. Eur Urol Suppl 13(1):e1124
Kusaka M, Sugimoto M, Fukami N, Sasaki H, Takenaka M, Anraku T et al (2015) Initial experience with a tailor-made simulation and navigation program using a 3D printer model of kidney transplantation surgery. Transplant Proc 47(3):596–599
Uwechue R, Gogalniceanu P, Kessaris N, Byrne N, Chandak P, Olsburgh J, et al (2018) A novel 3D-printed hybrid simulation model for robotic-assisted kidney transplantation (RAKT). J Robot Surg. https://link.springer.com/10.1007/s11701-018-0780-y. Accessed 27 Jan 2018
Cheung CL, Looi T, Lendvay TS, Drake JM, Farhat WA (2014) Use of 3Dimensional printing technology and silicone modeling in surgical simulation: development and face validation in pediatric laparoscopic pyeloplasty. J Surg Educ 71(5):762–767
Poniatowski LH, Wolf JS, Nakada SY, Reihsen TE, Sainfort F, Sweet RM (2014) Validity and acceptability of a high-fidelity physical simulation model for training of laparoscopic pyeloplasty. J Endourol 28(4):393–398
Horn M, Reh B, Wenz F, Stallkamp J, Mombaur K (2016) Patient specific corotated FEM simulation and gelatin phantom for prostate brachytherapy. In: 2016 6th IEEE international conference on biomedical robotics and biomechatronics (BioRob). IEEE, pp 341–346. https://ieeexplore.ieee.org/document/7523649/
Ghazi A, Stone J, Park J, Candela B, Kukreja J, Rashid H et al (2016) V8–01 full procedural simulation for transurethral resection of bladder tumors (TURBT) using 3D printing technology. J Urol 195(4):e771
Wong NC, Hoogenes J, Guo Y, Quantz MA, Matsumoto ED (2017) Techniques: utility of a 3D printed bladder model for teaching minimally invasive urethrovesical anastomosis. Can Urol Assoc J 11(7):321
Parkhomenko E, Yoon R, Okhunov Z, Patel RM, Dolan B, Kaler K et al (2019) Multi-institutional evaluation of producing and testing a novel 3D-printed laparoscopic trainer. Urology 124:297–301
Yoon R, Okhunov Z, Dolan B, Schwartz MJ, Shah PH, Bierwiler H et al (2017) PD41-10 evaluation of the feasibility of remotely manufactured low-cost three-dimensionally printed laparoscopic trainers and comparison to standard laparoscopic trainers. J Urol 197(4):e810–e811
Opik R, Hunt A, Ristolainen A, Aubin PM, Kruusmaa M (2012) Development of high fidelity liver and kidney phantom organs for use with robotic surgical systems. In: 2012 4th IEEE RAS & EMBS International Conference on Biomedical Robotics and Biomechatronics (BioRob). IEEE, pp 425–430. https://ieeexplore.ieee.org/document/6290831/
Chandak P, Byrne N, Lynch H, Allen C, Rottenberg G, Chandra A et al (2018) Three-dimensional printing in robot-assisted radical prostatectomy—an idea, development, exploration, assessment, long-term follow-up (IDEAL) Phase 2a study. BJU Int 122(3):360–361
Porpiglia F, Bertolo R, Amparore D, Checcucci E, Artibani W, Dasgupta P et al (2018) Augmented reality during robot-assisted radical prostatectomy: expert robotic surgeons’ on-the-spot insights after live surgery. Minerva Urol e Nefrol 70(2):226–229
Manning TG, O’Brien JS, Christidis D, Perera M, Coles-Black J, Chuen J et al (2018) Three dimensional models in uro-oncology: a future built with additive fabrication. World J Urol 36(4):557–563
Author information
Authors and Affiliations
Contributions
BS: manuscript writing. PD: manuscript editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants and/or animals:
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Smith, B., Dasgupta, P. 3D printing technology and its role in urological training. World J Urol 38, 2385–2391 (2020). https://doi.org/10.1007/s00345-019-02995-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-019-02995-1