Abstract
Purpose
To evaluate the prevalence of nocturia/nocturnal voiding frequency and its impact on overall physical and mental health status in German community-dwelling men and determine which lower urinary tract symptom (LUTS) is responsible for medical consultations in the 2-year follow-up period.
Methods
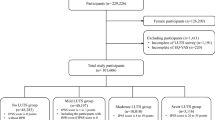
A sample of German men aged 50–80 years from a community-dwelling study was chosen for re-evaluation 2 years after initial assessment. Men were clinically investigated and completed the International Prostate Symptom Score, American Urology Association-Symptom Problem Index (AUA-SPI), and the Short-Form Health Survey (SF-12).
Results
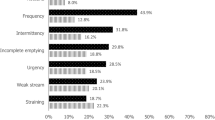
In total, 1,562 men were eligible for analysis. Mean nocturnal voiding frequency was 2.3 for all men and increased with ageing. SF-12 data indicated that physical but not mental health status was lower than in the average population. LUTS severity reduced both physical and mental health status (p < 0.001). Clinically relevant nocturia (≥2 voids/night) was present in 43 % of men and reduced both physical and mental health status (p < 0.001), whereas both HRQoL scales were not significantly reduced in men without or only one nocturnal void. In multivariate regression analysis using patient-reported bother (AUA-SPI) from LUTS, only bother from nocturnal voiding was significantly associated with medical consultations in the investigated 2-year follow-up period (odds ratio 2.6; 95 % confidence interval 1.6–4.2; p < 0.001).
Conclusions
Our study confirmed that nocturnal voiding is highly prevalent in community-dwelling men and reduce both physical and mental health status. Bother from nocturnal voiding is the most relevant component of LUTS responsible for medical consultations in German men.






Similar content being viewed by others
References
van Kerrebroeck P, Abrams P, Chaikin D, Donovan J, Fonda D, Jackson S et al (2002) The standardisation of terminology in nocturia: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn 21:179–183
Norgaard JP (2010) The role of nocturia in the quality of life of men with lower urinary tract symptoms. BJU Int 105:1016–1017
Tikkinen KA, Johnson TM 2nd, Tammela TL, Sintonen H, Haukka J, Huhtala H et al (2010) Nocturia frequency, bother, and quality of life: how often is too often? A population-based study in Finland. Eur Urol 57:488–496
Rodrigues P, Meller A, Campagnari JC, Alcantara D, D’Imperio M (2004) International prostate symptom score–IPSS-AUA as discriminat scale in 400 male patients with lower urinary tract symptoms (LUTS). Int Braz J Urol 30:135–141
Barry MJ, Fowler FJ Jr, O’Leary MP, Bruskewitz RC, Holtgrewe HL, Mebust WK (1995) Measuring disease-specific health status in men with benign prostatic hyperplasia: Measurement Committee of The American Urological Association. Med Care 33:AS145–AS155
Ware JE Jr, Kosinski M, Gandek B, Aaronson NK, Apolone G, Bech P et al (1998) The factor structure of the SF-36 health survey in 10 countries: results from the IQOLA Project. International Quality of Life Assessment. J Clin Epidemiol 51:1159–1165
Tengs TO, Wallace A (2000) One thousand health-related quality-of-life estimates. Med Care 38:583–637
Hernandez Fernandez C, Ristol Pont J, Estivill E, Batista Miranda JE, Lopez Aramburu MA (2007) Importance of nocturia and its impact on quality of sleep and quality of life in patient with benign prostatic hyperplasia. Actas Urol Esp 31:262–269
Berges RR, Pientka L, Hofner K, Senge T, Jonas U (2001) Male lower urinary tract symptoms and related health care seeking in Germany. Eur Urol 39:682–687
Berges RR, Pientka L (1999) Management of the BPH syndrome in Germany: who is treated and how? Eur Urol 36(Suppl 3):21–27
Berges R (2008) Epidemiology of benign prostatic syndrome. Associated risks and management data in German men over age 50. Urol A 47:141–148
Hutchison A, Farmer R, Verhamme K, Berges R, Navarrete RV. The efficacy of drugs for the treatment of LUTS/BPH, a study in 6 European countries. Eur Urol. 2007;51:207-15; discussion 15-6
Lowe FC, Batista J, Berges R, Chartier-Kastler E, Conti G, Desgrandchamps F et al (2005) Risk factors for disease progression in patients with lower urinary tract symptoms/benign prostatic hyperplasia (LUTS/BPH): a systematic analysis of expert opinion. Prostate Cancer Prostatic Dis 8:206–209
Speakman M, Batista J, Berges R, Chartier-Kastler E, Conti G, Desgrandchamps F et al (2005) Integrating risk profiles for disease progression in the treatment choice for patients with lower urinary tract symptoms/benign prostatic hyperplasia: a combined analysis of external evidence and clinical expertise. Prostate Cancer Prostatic Dis 8:369–374
Berges R, Dreikorn K, Hofner K, Madersbacher S, Michel MC, Muschter R et al (2009) Diagnostic and differential diagnosis of benign prostate syndrome (BPS): guidelines of the German Urologists. Urol A 48:1356–1360 62–64
Berges R, Oelke M (2011) Age-stratified normal values for prostate volume, PSA, maximum urinary flow rate, IPSS, and other LUTS/BPH indicators in the German male community-dwelling population aged 50 years or older. World J Urol 29:171–178
Koyanagi T, Artibani W, Correa R, Desgranchamps F, DeReijke TM, Govier F et al (1997) Initial diagnostic evaluation of men with lower urinary tract symptoms. 1989:258–60. In: Benign Prostatic Hyperplasia (BPH), 4th International Consultation on benign prostatic hyperplasia (BPH), Paris, July 2–5, 1997, Griffiths K, Denis L, Khoury S, Cockett ATK, McConnell J, Chatelain C, Murphy G, Yoshida O, Plymbridge Distributors, Plymouth
Ware J Jr, Kosinski M, Keller SD (1996) A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 34:220–233
Ware JE, Kosinski M, Turner-Bowker DM, Gandek B (2002) How to Score Version 2 of the SF-12v2® Health Survey (With a Supplement Documenting SF-12® Health Survey). QualityMetric Incorporated, Lincoln
German Federal Statistics Office (Statistisches Bundesamt) 2012. http://www.bpb.de/wissen/X39RH6,0,0,Bev%F6lkerung_nach_Altersgruppen_und_Geschlecht.html. Assessed 8 June 2014
Bosch JL, Weiss JP (2013) The prevalence and causes of nocturia. J Urol 189:S86–S92
Clark JA, Inui TS, Silliman RA, Bokhour BG, Krasnow SH, Robinson RA et al (2003) Patients’ perceptions of quality of life after treatment for early prostate cancer. J Clin Oncol 21:3777–3784
Homma Y, Yamaguchi T, Kondo Y, Horie S, Takahashi S, Kitamura T (2002) Significance of nocturia in the International prostate symptom score for benign prostatic hyperplasia. J Urol 167:172–176
Chen FY, Dai YT, Liu CK, Yu HJ, Liu CY, Chen TH (2007) Perception of nocturia and medical consulting behavior among community-dwelling women. Int Urogynecol J 18:431–436
Acknowledgments
The authors thank the German Working Group on BPH of the German Society of Urology for sponsoring the study from 1999 to 2005. The analyses shown in this article originate from data obtained in the follow-up visits of the original study.
Conflict of interest
Matthias Oelke is a consultant, speaker, and/or trial investigator in the field of LUTS/BPH for Apogepha, Astellas, Ferring, GlaxoSmithKline, Lilly, Mundipharma, Pfizer, and Recordati. Birgitt Wiese has no conflicts of interests. Richard Berges is consultant, speaker, and/or trial investigator in the field of LUTS/BPH for Astellas, Ferring, GlaxoSmithKline, Lilly, Pfizer, and Recordati.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Oelke, M., Wiese, B. & Berges, R. Nocturia and its impact on health-related quality of life and health care seeking behaviour in German community-dwelling men aged 50 years or older. World J Urol 32, 1155–1162 (2014). https://doi.org/10.1007/s00345-014-1374-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-014-1374-6