Abstract
Purpose
To analyse the surgical margins status of prostatic glands, resected by laparoscopic radical prostatectomy (LRP) for prostate cancer, and to correlate it with biochemical free survival rate (BFSR).
Methods
Data were collected prospectively from 405 patients undergoing LRP from 2000 to 2009 at a single institution. Patients undergoing neoadjuvant and/or adjuvant therapy were excluded from the study. Three hundred patients matched all the criteria: 232 of these had negative surgical margins (NSM) and 68 positive surgical margins (PSM). The median follow-up was 62 months. PSM were classified based on the following: (a) the number of margins, monofocal and multifocal, (b) the location, apical or non-apical and (c) the extension, ≤2.8 mm or >2.8 mm. These data were then entered into a multivariate analysis.
Results
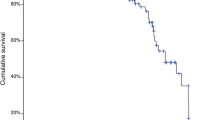
Overall BFSR rate was 67.6% in PSM group and 88.8% in NSM group (P < 0.001). We registered a HR of 3.78 in multivariate analysis (P < 0.001). In terms of the extension, BFSR in univariate survival analysis was 77.8% in ≤2.8 mm PSM and 38.9% in >2.8 mm PSM (P = 0.003), with a HR of 5.68 (P = 0.011) in multivariate analysis. BFSR was 59% for apical margins and 77% for non-apical margins (P = 0.038). In monofocal margins, BFSR was 73%, while 53% in multifocal (P = 0.014).
Conclusions
We recommend careful evaluation of patients with PSM following LRP, especially if they are more than 2.8 mm, and in these cases, adjuvant therapy should be considered after radical surgery.

Similar content being viewed by others
References
Wright JL, Dalkin BL, True LD et al (2010) Positive surgical margins at radical prostatectomy predict prostate cancer specific mortality. J Urol 183(6):2213–2218
Grossfeld GD, Chang JJ, Broering JM et al (2000) Impact of positive surgical margins on prostate cancer recurrence and the use of secondary cancer treatment: data from the CaPSURE database. Urology 163(4):1171–1177
Blute ML, Bostwick DG, Bergstralh EJ et al (1997) Anatomic site-specific positive margins in organ-confined prostate cancer and its impact on outcome after radical prostatectomy. Urology 50(5):733–739
Karakiewicz PI, Eastham JA, Graefen M et al (2005) Prognostic impact of positive surgical margins in surgically treated prostate cancer: multi-institutional assessment of 5831 patients. Urology 66(6):1245–1250
Swindle P, Eastham JA, Ohori M et al (2005) Do margins matter? The prognostic significance of positive surgical margins in radical prostatectomy specimens. J Urol 174(3):903–907
Fesseha T, Sakr W, Grignon D et al (1997) Prognostic implications of a positive apical margin in radical prostatectomy specimens. J Urol 158(6):2176–2179
Stamey TA, McNeal JE, Yemoto CM, Sigal BM, Johnstone IM (1999) Biological determinants of cancer progression in men with prostate cancer. JAMA 281(15):1395–1400
Vis AN, Schröder FH, van der Kwast TH (2006) The actual value of the surgical margin status as a predictor of disease progression in men with early prostate cancer. Eur Urol 50(2):258–265
Porpiglia F, Terrone C, Tarabuzzi R et al (2006) Transperitoneal versus extraperitoneal laparoscopic radical prostatectomy: experience of a single center. Urology 68(2):376–380
Montironi R, Mazzucchelli R, Kwast T (2003) Morphological assessment of radical prostatectomy specimens. A protocol with clinical relevance. Virchows Arch 442(3):211–217
Cookson MS, Aus G, Burnett AL et al (2007) Variation in the definition of biochemical recurrence in patients treated for localized prostate cancer: the American urological association prostate guidelines for localized prostate cancer update panel report and recommendations for a standard in the reporting of surgical outcomes. J Urol 177(2):540–544
Stephenson AJ, Wood DP, Kattan MW et al (2009) Location, extent and number of positive surgical margins do not improve accuracy of predicting prostate cancer recurrence after radical prostatectomy. J Urol 182(4):1357–1363
Salomon L, Anastasiadis A, Evrel O et al (2003) Location of positive surgical margins after retropubic, perineal, and laparoscopic radical prostatectomy for organ-confined prostate cancer. Urology 61(2):386–390
Kausik SJ, Blute ML, Sebo TJ et al (2002) Prognostic significance of positive surgical margins in patients with extraprostatic carcinoma after radical prostatectomy cancer. Cancer 95(6):1215–1219
Ochiai A, Sotelo T, Troncoso P, Bhadkamkar V, Babaian RJ (2008) Natural history of biochemical progression after radical prostatectomy based on length of a positive margin. Urology 71(2):308–312
Kordan Y, Salem S, Chang SS et al (2009) Impact of positive apical surgical margins on likelihood of biochemical recurrence after radical prostatectomy. J Urol 182(6):2695–2701
van Oort IM, Bruins HM, Kiemeney LALM, Knipscheer BC, Witjes JA, Hulsbergen-van de Kaa CA (2010) The length of positive surgical margins correlates with biochemical recurrence after radical prostatectomy. Histopathology 56(4):464–471
Babaian RJ, Troncoso P, Bhadkamkar V, Johnston DA (2001) Analysis of clinicopathologic factors predicting outcome after radical prostatectomy. Cancer 91(8):1414–1422
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Porpiglia, F., Fiori, C., Manfredi, M. et al. Surgical margin status of specimen and oncological outcomes after laparoscopic radical prostatectomy: experience after 400 procedures. World J Urol 30, 245–250 (2012). https://doi.org/10.1007/s00345-011-0711-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-011-0711-2