Abstract
Objectives
To study the results of chemotherapy combined with intravesical hyperthermia in patients with mainly BCG-failing carcinoma in situ (CIS).
Methods
Patients with histologically confirmed CIS were included retrospectively. Outpatient thermochemotherapy treatment was done with mitomycin-C (MMC) and the Synergo® system SB-TS 101 (temperature range between 41 and 44°C), weekly for 6–8 weeks, followed by 4–6 sessions every 6–8 weeks.
Results
Fifty-one patients were treated between 1997 and 2005 from 15 European centers. Thirty-four were pre-treated with BCG. Mean age was 69.9 years. Twenty-four patients had concomitant papillary tumors. The mean number of hyperthermia/MMC treatments per patient was 10.0. Of the 49 evaluable patients 45 had a biopsy and cytology proven complete response. In two patients CIS disappeared, but they had persistent papillary tumors. Follow-up of 45 complete responders showed 22 recurrences after a mean of 27 months (median 22): T2 (4), T1 (4), T1/CIS (1), CIS (5), Ta/CIS (2), Ta (5) and Tx (1). Side effects (bladder complaints) were generally mild and transient.
Conclusions
In patients with primary or BCG-failing CIS, treatment with intravesical hyperthermia and MMC appears a safe and effective treatment. The initial complete response rate is 92%, which remains approximately 50% after 2 years.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Carcinoma in situ (CIS) of the urinary bladder is defined as non-papillary high-grade non-invasive urothelial cell carcinoma (UCC). It is an aggressive form of non-muscle invasive bladder cancer (NMIBC) with a high progression rate and an even higher recurrence rate [1]. In case of concomitant high-grade pT1 tumors the prognosis is even worse [2]. Even when patients are treated with cystectomy, the presence of CIS is an adverse prognostic sign [3, 4]. Current standard therapy in case of CIS is intravesical Bacillus Calmette–Guérin (BCG). Although 30–40% of patients do not respond to one course of six instillations, half of these still achieve a complete response after an additional course of six instillations [5]. Consequently, the treatment guideline in CIS patients is maintenance BCG [6, 7]. The disadvantage of BCG in comparison with intravesical chemotherapy is the increased frequency and severity of side effects. Alternative therapies for BCG in primary CIS patients remain experimental or are insufficiently documented.
In case of BCG-refractory CIS, cystectomy is the treatment of choice [8]. Intravesical approaches have failed, such as valrubicin [9], are investigational, such as gemcitabine [10] and mycobacterial cell wall preparations [11], or efficacy should be confirmed, such as the combination of BCG and interferon-alpha 2b [12]. Device-assisted strategies for primary CIS include photodynamic therapy (PDT), electromotive drug administration (EMDA) and the combination of intravesical hyperthermia and chemotherapy (thermochemotherapy). PDT has some encouraging results [13] and sequential BCG with EMDA/mitomycin-C (MMC) is emerging [14].
Thermochemotherapy (MMC/hyperthermia) has proven to be more effective than MMC alone for patients with Ta-1 G1-3 NMIBC in comparative studies with ablative [15] as well as prophylactic intent [16]. Gofrit et al. [17] reported a beneficial prophylactic effect of thermochemotherapy in patients with G3 tumors, 15/24 (62.5%) patients were recurrence-free after a mean follow-up of 35.3 months. In addition, ablation of high-grade tumors was achieved in 21/28 (75%) patients, of whom 81% remained tumor free after a mean follow-up of 20 months. Van der Heijden et al. [18] reported the use of thermochemotherapy with prophylactic intent in 90 patients with intermediate and high risk NMIBC. After 1 and 2 years of follow-up, respectively, 14.3 and 24.6% of all patients experienced a recurrence. In 41 patients previously failing BCG treatment, the recurrence rates, respectively, were 23 and 41%.
In the current study, we report for the first time the efficacy of thermochemotherapy in patients with CIS, predominantly failing BCG.
Methods
Patient selection
Retrospectively, data of all patients treated with MMC in combination with hyperthermia were gathered from 15 centers. Of these, patients with biopsy proven and histologically confirmed CIS were eligible for analysis. Patients were included with a WHO performance status of 0–2 and a life expectancy of more than 24 months. Criteria for ineligibility were a limited bladder capacity (<150 ml), any concomitant malignancy, extravesical UCC and the presence of a diverticulum of the bladder. Patients without follow-up cystoscopy or with less than six treatments were excluded from the analysis.
Treatment
The treatment set up has been described in detail before [19]. In short, the Synergo® system SB-TS 101 is used to deliver local microwave induced hyperthermia and intravesical chemotherapy simultaneously. This system consists of a 915 MHz intravesical microwave applicator that delivers hyperthermia to the bladder wall via direct irradiation. The hyperthermia range is between 41 and 44°C, controlled by five thermocouples integrated in a specially designed 20°F treatment catheter. To avoid urethral overheating and disintegration of MMC, the solution is continuously pumped out of the bladder and re-instilled after being cooled. Treatment was done with 20 mg MMC (Kyowa Hakko Kogyo Co., Tokyo, Japan) in 50 ml sterile water, replaced by a fresh identical solution after 30 min (a total of 40 mg MMC in 1 h), on an outpatient basis weekly for 6 weeks (prophylactic schedule), followed by six maintenance instillations (one instillation every 6 weeks). Patients whose concomitant papillary tumors were not or could not be completely resected, or patients with wide areas of CIS, were treated with a higher dose of MMC (twice 40 mg, a total of 80 mg in 1 h), weekly for 8 weeks (ablative schedule), followed by six maintenance instillations of twice 20 mg MMC (one instillation every 6 weeks). In case of bacterial cystitis or significant hematuria, treatment delay was recommended.
Follow-up
Cystoscopy and urine cytology were repeated every 3 months for a follow-up period of 24 months. Biopsies from suspicious lesions were performed. The primary end-point of the study was eradication of CIS, proven by cystoscopy, biopsy and cytology. Secondary end-point was either a pathology proven tumor recurrence, or a clear cystoscopical recurrence indicated by the investigator. Side effects and adverse events were noted in the patient’s file. Data were collected during treatment and follow-up.
For statistical analysis the Epi-Info for Windows version 3.3.2 was used.
Results
Patients
In total 51 patients with CIS were included between March 1997 and June 2005 from centers in Israel, Italy, Germany, Switzerland, Austria and the Netherlands. Mean age was 69.9 years (50–87), with a male-to-female ratio of 4:1 (42 vs. 9). On an average, the patients had 3.2 previous TUR procedures (1–8). Previous “worst” histology revealed CIS in 33 patients, grade 3 in 24 patients, and T1 in 20 patients (some patients had more than one of these histopathologic characteristics). Previous intravesical treatments included BCG (n = 34), MMC (n = 11), epirubicin (n = 4), gemcitabine (n = 3), Keyhole–Limpet hemocyanin (KLH) (n = 1), valrubicin (n = 1) and radiation therapy (n = 1). Of the 34 patients previously treated with BCG, 17 were BCG refractory, 2 BCG intolerant and 15 patients relapsed (3 patients within 12 months, 6 patients between 12 and 24 months, and 6 patients after 24 months). Twenty-four patients had concomitant papillary tumors: TaG1 (n = 1), TaG2 (n = 6), TaG3 (n = 8), T1G2 (n = 4) and T1G3 (n = 5).
Eighteen patients received the prophylactic schedule (twice 20 mg MMC), and 33 patients received the ablative schedule (twice 40 mg MMC) together with intravesical hyperthermia. Apart form the MMC dose, all patients in all centers were treated according to the same treatment protocol. The mean total number of hyperthermia treatments was 10.0 (2–21). Two patients dropped out during initial treatment (1 patient with hematuria after the second treatment, and one patient with a false route after the fourth treatment) and did not receive the initial six instillations. These two patients were not considered for efficacy.
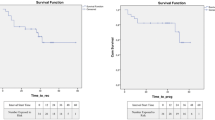
Efficacy
In total, 49 patients remained available for treatment response analysis. Of these patients, 45 (92%) had a complete biopsy and cytology proven disappearance of CIS at 3 months. In two additional patients CIS disappeared but the concomitant papillary tumor persisted. There was no difference in response between patients with and without concomitant papillary tumors (P = 0.94, data not shown), irrespective whether the papillary tumor was pTa or pT1. There was also no difference in response between patients who were of were not BCG failures, irrespective of the type of BCG failure (BCG resistant or early or late BCG failures, P = 0.63, data not shown). Since the 2-year results of the 20 mg (prophylactic, n = 19) and 40 mg (ablative, n = 26) regimens are also not significantly different (P = 0.10, data not shown) these groups are analyzed together. Of all 45 complete responders additional follow-up is available with a mean follow-up of 27 (3–77, median 22) months. Of these 45 patients, 22 (49%) had a recurrence. Five of the patients had a cystectomy because of recurrent T1 (n = 1) or >T1 (n = 4) tumor, after, respectively, 11 and, 12 and 13 and, 18 months. One patient had a cystectomy due to a contracted bladder, but he was tumor free. The other 17 patients recurred with pure CIS (n = 5), T1 + CIS (n = 1), Ta + CIS (n = 2), pT1 (n = 3), pTa (n = 5) and pTx (n = 1). These patients were treated conservatively.
Safety
Safety of chemotherapy treatment combined with microwave hyperthermia was previously published [18]. Side effects in this study also were generally mild and transient, and included mainly pain and bladder spasms during treatment and irritative bladder symptoms for 1–2 days thereafter. Side effects had virtually no influence on the treatment plan: as mentioned above, one patient stopped treatment due to hematuria, one treatment session was delayed for 1 week and one session was shortened. Adverse events could not be graded according to the common toxicity criteria retrospectively. Frequency of events is given in Table 1.
Discussion
As indicated in the introduction international guidelines advise to treat CIS patients with maintenance intravesical BCG, since it appears to be able to prevent or delay disease progression. However, the possibilities in case of BCG-refractory CIS are limited.
Intravesical chemotherapy has been studied. Valrubicin is the only FDA approved drug for patients with CIS-failing intravesical therapy such as BCG. This was based on a phase-II study with 90 patients [9]. After a year of follow-up 21% had a complete response, which decreased to 8% after 2 years. A marker lesion study in refractory patients confirmed initial potential of valrubicin, since 18/39 (46%) patients were free of disease after 3 months [20]. However, due to several reasons, valrubicin is not used currently. Intravesical gemcitabine was also used in BCG-refractory patients resulting in three small series. In one study with 18 patients (of whom 12 had pure CIS, 2 T1 + CIS), 11 patients showed negative biopsies after treatment, of whom 7 also had negative cytology [10]. In another recent phase-II study 7 of 16 high-risk patients (not specified) remained recurrence-free at 12 months [21]. Fifteen of 30 patients (23 CIS, 4 Ta high grade, 3 T1) with NMIBC that were BCG refractory (27) or BCG intolerant (3) had a complete response in a study by Dalbagni et al. [22]. The 1-year recurrence-free survival rate for patients with a complete response was 21%.
Immunotherapy in BCG failures is also reported. Bropirimine, an oral immunomodulator, was studied in BCG-resistant CIS in a phase-II trial [23]. Fourteen out of 47 BCG-resistant patients showed a complete response with a median duration of more than 12 months. Unfortunately, no further evaluation of the drug has been done. The combination of interferon (IFN)-alpha and BCG for BCG failures has been the subject of a large multi-center phase-II trial [24]. In all, 467 patients failing BCG were treated with low-dose BCG plus IFN. Twenty-seven percent of these patients had isolated or concomitant CIS. With a median follow-up of 24 months, 45% remained tumor-free, compared with 59% of the 536 patients in the BCG naïve group. Although there was no sub-analysis for CIS patients, CIS did not significantly affect outcome in a multivariate analysis. Patients treated with two or more courses of BCG did not respond well to BCG plus IFN, suggesting that this group of patients should go on to cystectomy.
A recent method of device-assisted intravesical therapy is PDT, which combines photo sensitizers that selectively bind to tumors and a powerful intravesical light source to destroy tumors. Waidelich et al. [25] used PDT with oral 5-aminolevulinic acid (5-ALA) in five BCG-failing CIS patients, and found three patients recurrence-free after a median follow-up of 36 months. Intravesical 5-ALA was studied in 10 BCG failures (presence of CIS not specified) of which four remained tumor-free after an average follow-up of 11.8 months [13]. EMDA is based on the concept of temporarily breaching the urothelial barrier of the bladder and enhancing penetration of drugs, among which MMC, in a controllable manner [26]. Di Stasi et al. [14] performed a randomized controlled trial in 212 patients with stage T1 NMIBC, comparing BCG alone (105 patients, 28 with concomitant CIS) with sequential BCG and MMC/EMDA (107 patients, 29 with concomitant CIS), with maintenance therapy in both arms. This study found a significantly higher disease-free interval, lower recurrence rate, lower progression rate and lower disease-specific mortality in favor of sequential BCG and MMC/EMDA. Although not designed to assess complete response rates of patients with CIS, 12/28 (42.9%) patients treated with BCG alone and 16/28 (55.2%) patients treated with sequential BCG and EMDA/MMC obtained a complete response at 3 months, and respectively 16/28 (57.1%) patients and 20/29 (69.0%) patients at 6 months.
Limited and disappointing information is available on the use of intravesical MMC in BCG failures. The Swedish-Norwegian bladder cancer group compared MMC and BCG in NMIBC patients and treatment failures were allowed to cross over [27]. Twenty-one BCG failures changed to MMC therapy, but only four remained recurrence-free with a median follow-up of 64 months.
In all, conservative therapy in patients with BCG-refractory CIS remains largely experimental, and indeed guidelines advise cystectomy as a treatment of choice for CIS failing adequate BCG. On the other hand, cystectomy remains major surgery with mortality and morbidity. Prostate sparing cystectomy improves outcome of erectile function, but oncological outcome might be hampered [28]. Another approach is an attempt to improve the efficacy of intravesical MMC with devices such as EMDA or intravesical bladder wall hyperthermia (Synergo®). In patients with papillary tumors failing BCG thermochemotherapy showed promising results [18]. In a group of 41 BCG-failing patients the 1 and 2 years recurrence rates after a year of thermochemotherapy were 23 and 41%, respectively. In this study, 34 of the 51 patients with CIS were BCG pretreated, with an initial CR rate after 3 months of 92%, which was still more than 50% after 2 years of follow-up.
Conclusions
The current report specifically looked at the results of the combination of intravesical hyperthermia and chemotherapy in patients with (mainly BCG failing) CIS of the urinary bladder. Side effects were mild and transient as expected and reported earlier [18]. The initial response rate was 92% (45/49), and in two additional patients CIS disappeared, whereas papillary tumors did not. Although numbers are small, the risk of tumor progression is low during this conservative treatment, suggesting that this approach could be suggested to a patient before considering cystectomy. Limitations are obviously the retrospective nature of the study and the sample size. It took several years and a number of centers to collect these (BCG failing) CIS patients. Not only CIS patients are not very common, also the hyperthermia equipment is still not commonly available. This is predominantly a cost issue, not a logistical issue or patients acceptance. Another limitation is the lack of review pathology. CIS, on the other hand, is a disease with a high inter-observer agreement [29], so the influence of review pathology for this group of patients seems small. In all, although CIS is an infrequent disease, considering the limited existing of conservative alternatives in these patients and the impact of radical surgery, thermochemotherapy definitely deserves further study as conservative alternative in these patients.
References
Park J, Song C, Hong JH, Park BH, Cho YM, Kim CS, Ahn H (2009) Prognostic significance of non-papillary tumor morphology as a predictor of cancer progression and survival in patients with primary T1G3 bladder cancer. World J Urol. doi:10.1007/s00345-008-0350-4
Sylvester RJ, van der Meijden AP, Oosterlinck W et al (2006) Predicting recurrence and progression in individual patients with stage Ta T1 bladder cancer using EORTC risk tables: a combined analysis of 2596 patients from seven EORTC trials. Eur Urol 49:466–5. doi:10.1016/j.eururo.2005.12.031
Denzinger S, Fritsche HM, Otto W, Blana A, Wieland WF, Burger M (2008) Early versus deferred cystectomy for initial high-risk pT1G3 urothelial carcinoma of the bladder: do risk factors define feasibility of bladder-sparing approach? Eur Urol 53:146–152. doi:10.1016/j.eururo.2007.06.030
Shariat SF, Palapattu GS, Karakiewicz PI, Rogers CG, Vazina A, Bastian PJ, Schoenberg MP, Lerner SP, Sagalowsky AI, Lotan Y (2007) Concomitant carcinoma in situ is a feature of aggressive disease in patients with organ-confined TCC at radical cystectomy. Eur Urol 51:152–160. doi:10.1016/j.eururo.2006.08.037
Griffiths TR, Charlton M, Neal DE, Powell PH (2002) Treatment of carcinoma in situ with intravesical bacillus Calmette–Guerin without maintenance. J Urol 167:2408–2412. doi:10.1016/S0022-5347(05)64994-4
van der Meijden AP, Sylvester R, Oosterlinck W et al (2005) EAU guidelines on the diagnosis and treatment of urothelial carcinoma in situ. Eur Urol 48:363–371
Hall MC, Chang SS, Dalbagni G, Pruthi RS, Seigne JD, Skinner EC, Wolf JS Jr, Schellhammer PF (2007) Guideline for the management of nonmuscle invasive bladder cancer (stages Ta, T1, and Tis): 2007 update. J Urol 178:2314–2330. doi:10.1016/j.juro.2007.09.003
Witjes JA (2006) Management of BCG failures in superficial bladder cancer: a review. Eur Urol 49:790–797. doi:10.1016/j.eururo.2006.01.017
Steinberg G, Bahnson R, Brosman S, Middleton R, Wajsman Z, Wehle M (2000) Efficacy and safety of valrubicin for the treatment of Bacillus Calmette–Guerin refractory carcinoma in situ of the bladder. The valrubicin study group. J Urol 163:761–767. doi:10.1016/S0022-5347(05)67799-3
Dalbagni G, Russo P, Sheinfeld J et al (2002) Phase I trial of intravesical gemcitabine in bacillus Calmette–Guerin-refractory transitional-cell carcinoma of the bladder. J Clin Oncol 20:3193–3198. doi:10.1200/JCO.2002.02.066
Morales A (2008) Evolution of intravesical immunotherapy for bladder cancer: mycobacterial cell wall preparation as a promising agent. Expert Opin Investig Drugs 17:1067–1073. doi:10.1517/13543784.17.7.1067
O’Donnell MA, Krohn J, DeWolf WC (2001) Salvage intravesical therapy with interferon-alpha 2b plus low dose bacillus Calmette–Guerin is effective in patients with superficial bladder cancer in whom bacillus Calmette–Guerin alone previously failed. J Urol 166:1300–1304. doi:10.1016/S0022-5347(05)65757-6 (discussion)
Berger AP, Steiner H, Stenzl A, Akkad T, Bartsch G, Holtl L (2003) Photodynamic therapy with intravesical instillation of 5-aminolevulinic acid for patients with recurrent superficial bladder cancer: a single-center study. Urology 61:338–341. doi:10.1016/S0090-4295(02)02123-4
Di Stasi SM, Giannantoni A, Giurioli A et al (2006) Sequential BCG and electromotive mitomycin versus BCG alone for high-risk superficial bladder cancer: a randomised controlled trial. Lancet Oncol 7:43–51. doi:10.1016/S1470-2045(05)70472-1
Colombo R, Da Pozzo LF, Lev A, Freschi M, Gallus G, Rigatti P (1996) Neoadjuvant combined microwave induced local hyperthermia and topical chemotherapy versus chemotherapy alone for superficial bladder cancer. J Urol 155:1227–1232. doi:10.1016/S0022-5347(01)66225-6
Colombo R, Da Pozzo LF, Salonia A et al (2003) Multicentric study comparing intravesical chemotherapy alone and with local microwave hyperthermia for prophylaxis of recurrence of superficial transitional cell carcinoma. J Clin Oncol 21:4270–4276. doi:10.1200/JCO.2003.01.089
Gofrit ON, Shapiro A, Pode D et al (2004) Combined local bladder hyperthermia and intravesical chemotherapy for the treatment of high-grade superficial bladder cancer. Urology 63:466–471. doi:10.1016/j.urology.2003.10.036
van der Heijden AG, Kiemeney LA, Gofrit ON et al (2004) Preliminary European results of local microwave hyperthermia and chemotherapy treatment in intermediate or high risk superficial transitional cell carcinoma of the bladder. Eur Urol 46:65–71. doi:10.1016/j.eururo.2004.01.019
Colombo R, Lev A, Da Pozzo LF, Freschi M, Gallus G, Rigatti P (1995) A new approach using local combined microwave hyperthermia and chemotherapy in superficial transitional bladder carcinoma treatment. J Urol 153:959–963. doi:10.1016/S0022-5347(01)67613-4
Newling DW, Hetherington J, Sundaram SK, Robinson MR, Kisbenedek L (2001) The use of valrubicin for the chemoresection of superficial bladder cancer—a marker lesion study. Eur Urol 39:643–647. doi:10.1159/000052521
Bartoletti R, Cai T, Gacci M et al (2005) Intravesical gemcitabine therapy for superficial transitional cell carcinoma: results of a phase II prospective multicenter study. Urology 66:726–731. doi:10.1016/j.urology.2005.04.062
Dalbagni G, Russo P, Bochner B et al (2006) Phase II trial of intravesical gemcitabine in bacille Calmette–Guerin-refractory transitional cell carcinoma of the bladder. J Clin Oncol 24:2729–2734. doi:10.1200/JCO.2005.05.2720
Sarosdy MF, Manyak MJ, Sagalowsky AI et al (1998) Oral bropirimine immunotherapy of bladder carcinoma in situ after prior intravesical bacille Calmette-Guerin. Urology 51:226–231. doi:10.1016/S0090-4295(97)00510-4
Joudi FN, Smith BJ, O’Donnell MA (2006) Final results from a national multicenter phase II trial of combination bacillus Calmette–Guerin plus interferon alpha-2B for reducing recurrence of superficial bladder cancer. Urol Oncol 24:344–348. doi:10.1016/j.urolonc.2005.11.026
Waidelich R, Stepp H, Baumgartner R, Weninger E, Hofstetter A, Kriegmair M (2001) Clinical experience with 5-aminolevulinic acid and photodynamic therapy for refractory superficial bladder cancer. J Urol 165:1904–1907. doi:10.1016/S0022-5347(05)66239-8
Colombo R, Brausi M, Da PL et al (2001) Thermo-chemotherapy and electromotive drug administration of mitomycin C in superficial bladder cancer eradication: a pilot study on marker lesion. Eur Urol 39:95–100. doi:10.1159/000052419
Malmstrom PU, Wijkstrom H, Lundholm C, Wester K, Busch C, Norlen BJ (1999) 5-year followup of a randomized prospective study comparing mitomycin C and bacillus Calmette–Guerin in patients with superficial bladder carcinoma. Swedish-Norwegian bladder cancer study group. J Urol 161:1124–1127. doi:10.1016/S0022-5347(01)61607-0
Hautmann RE, Stein JP (2005) Neobladder with prostatic capsule and seminal-sparing cystectomy for bladder cancer: a step in the wrong direction. Urol Clin North Am 32:177–185. doi:10.1016/j.ucl.2005.02.001
Witjes JA, Kiemeney LA, Schaafsma HE, Debruyne FM (1994) The influence of review pathology on study outcome of a randomized multicentre superficial bladder cancer trial. Br J Urol 73:172–176. doi:10.1111/j.1464-410X.1994.tb07487.x
Acknowledgments
The additional members of the European Synergo® working party (in alphabetical order): T. Akkad (Innsbruck, Austria), R. Colombo (Milan, Italy), D. Englstein (Petah-Tikva, Israel), R. Hurle (Bergamo, Italy), I. Leibovich (Kfar-Saba, Israel), G. Luedecke (Giessen, Germany), M. Maffezzini (Genova, Italy), S. Sandri (Magenta, Italy), A. Stein (Haifa, Israel), G. Thalmann (Bern, Switzerland), F. Verweij (Milan, Italy)
Conflict of interest statement
Witjes had received an honorarium as advisor to MEL in the FDA Synergo registration procedure. The other authors have nothing to disclose.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Alfred Witjes, J., Hendricksen, K., Gofrit, O. et al. Intravesical hyperthermia and mitomycin-C for carcinoma in situ of the urinary bladder: experience of the European Synergo® working party. World J Urol 27, 319–324 (2009). https://doi.org/10.1007/s00345-009-0384-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-009-0384-2