Abstract
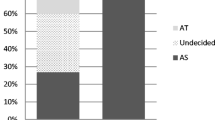
Locally confined prostate cancer (PCa) can be treated by various treatment options (e.g. radical prostatectomy or radiation therapy) with comparable results but different possible side effects. Therefore, treatment recommendations can vary between urologists and radiation oncologists. In 2001 the Charité-Campus Benjamin Franklin (CBF, Berlin), established the first interdisciplinary consulting service for prostate cancer patients in Germany. The aim was to offer a comprehensive and neutral consultation on all treatment options and to make treatment recommendations. The study examines what benefits may be derived from this type of consultation. A total of 362 patients presented to the consulting service between May 2001 and April 2003. Two questionnaires were used. The first one contained epidemiological questions as well as questions covering information already available on PCa. It also examined feelings and fears about the disease and possible treatment options. The second questionnaire was completed 2 weeks after the consultation to evaluate the treatment decision, determine the patient’s satisfaction with the consultation and trace the development of feelings and fears. Of the patients, 334 (92.2%) were completely assessable. All patients had already obtained information about the disease and possible treatment options and wished to be involved in the decision-making process through objective and neutral consultation. Nearly all of them had a great fear of the possible side effects of therapy. Such a comprehensive consultation is time-consuming (average of 35 min) but largely received a very positive assessment in that a total of 66% found it either helpful (n=74, 22%) or very helpful (n=147, 44%). Patients felt they had been completely informed in 92% of the cases. Only 22 (9.7%) had still failed to make a decision after 2 weeks, 115 patients had stage T1c, PSA <10 ng/ml and a Gleason score ≤7. In these cases an equivalent recommendation for radical prostatectomy, percutaneous radiotherapy or permanent seed implantation was given. Of these, 49 (43.4%) decided on the surgical intervention, 48 (42.5%) on a type of radiotherapy and only 18 (15.6%) remained undecided. The histological examination of prostatectomy specimens from patients who had decided to undergo radical surgery at CBF showed a significant decrease in the rate of extracapsular disease extension (≥T3) from 38% to 20% during the observation period. The interdisciplinary approach has made the process of deciding on an appropriate treatment much easier for the patient. The time-consuming consultation enables better selection of individual treatment modalities and their possible side effects from the point of view of both the patients and the attending physicians. In this study, patients chose either radical surgery or radiotherapy with equal frequency.





Similar content being viewed by others
References
D’Amico AV, Whittington R, Malkowicz SB et al. (2002) Biochemical outcome after radical prostatectomy or external beam radiation therapy for patients with clinically localized prostate carcinoma in the prostate specific antigen era. Cancer 95:281–286
Graefen M, Ohori M, Karakiewicz PI et al. (2004) Assessment of the enhancement in predictive accuracy provided by systematic biopsy in predicting outcome for clinically localized prostate cancer. J Urol 171:200–203
Haese A, Chaudhari M, Miller MC et al. (2003) Quantitative biopsy pathology for the prediction of pathologically organ-confined prostate carcinoma: a multiinstitutional validation study. Cancer 97:969–978
Harlan L, Brawley O, Pommerenke F et al. (1995) Geographic, age, and racial variation in the treatment of local/regional carcinoma of the prostate. J Clin Oncol 13:93–100
Kattan MW, Eastham JA, Stapleton AM, Wheeler TM, Scardino PT (1998) A preoperative nomogram for disease recurrence following radical prostatectomy for prostate cancer. J Natl Cancer Inst 90:766–771
Kattan MW, Wheeler TM, Scardino PT (1999) Postoperative nomogram for disease recurrence after radical prostatectomy for prostate cancer. J Clin Oncol 17:1499–1507
Kattan MW, Potters L, Blasko JC et al. (2001) Pretreatment nomogram for predicting freedom from recurrence after permanent prostate brachytherapy in prostate cancer. Urology 58:393
Kattan MW, Eastham JA, Wheeler TM et al. (2003) Counseling men with prostate cancer: a nomogram for predicting the presence of small, moderately differentiated, confined tumors. J Urol 170:1792–1797
Moul JW (2002) Radical prostatectomy versus radiation therapy for clinically localized prostate carcinoma: the butcher and the baker selling their wares. Cancer 95:211–214
Partin AW, Mangold LA, Lamm DM, Walsh PC, Epstein JI, Pearson JD (2001) Contemporary update of prostate cancer staging nomograms (Partin Tables) for the new millennium. Urology 58:843–848
Post PN, Kil PJ, Coebergh JW (1999) Trends in survival of prostate cancer in southeastern Netherlands, 1971–1989. Int J Cancer 81:551–554
Schwartz K, Bunner S, Bearer R, Severson RK (2002) Complications from treatment for prostate carcinoma among men in the Detroit area. Cancer 95:82–89
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schostak, M., Wiegel, T., Müller, M. et al. Shared decision-making—Results from an interdisciplinary consulting service for prostate cancer. World J Urol 22, 441–448 (2004). https://doi.org/10.1007/s00345-004-0447-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-004-0447-3