Abstract
Objective
To investigate the feasibility of using noninvasive neuroimaging methods in visualizing and evaluating the clearance of the glymphatic-meningeal lymphatic system (GMLS) in patients with arteriosclerotic cerebral small-vessel disease (CSVD) and controls.
Methods
This observational study recruited patients with high-burden CSVD and controls (age 50–80 years). At multiple time points before and after intravenous administration of a contrast agent, three-dimensional (3D) brain volume T1-weighted imaging and 3D Cube T2-fluid attenuated inversion recovery imaging were performed to visualize and assess the clearance of the glymphatics and meningeal lymphatic vessels (mLVs). We measured the signal intensity ratio (SIR) of four regions of interest representing the glymphatics and mLVs at each time point. The clearance rate at 24 h (CR24h) and changes in the SIR from baseline to 24 h (∆SIR) were defined as the clearance function. The analysis of variance was used to evaluate the group differences after adjusting for hypertension.
Results
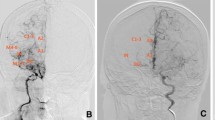
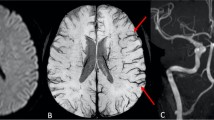
A total of 20 CSVD patients and 15 controls were included. Cortical periarterial enhancement and the enhancement of enlarged perivascular spaces in the basal ganglia were respectively observed in 11 (55.00%) and 16 (80.00%) CSVD patients, but in none of controls. All CSVD patients and most of controls (80.00%) showed cortical perivenous enhancement. Para-sinus enhancement was observed in all participants. CSVD patients showed lower CR24h and higher ∆SIR of the glymphatics and mLVs (all p < 0.05).
Conclusion
The impaired drainage of the GMLS in patients with high-burden CSVD could be visually evaluated using noninvasive neuroimaging methods with intravenous gadolinium-based contrast-enhancement.
Clinical relevance statement
Dynamic intravenous contrast-enhanced MRI could visually evaluate the impaired drainage of the glymphatic-meningeal lymphatic system in patients with high-burden cerebral small-vessel disease and could help to explore a new therapeutic target.
Key Points
• Signal intensity changes in regions representing the glymphatic-meningeal lymphatic system (GMLS) can reflect the drainage function based on contrast-enhanced 3D-FLAIR and 3D T1-weighted MRI.
• Impaired drainage of the GMLS in patients with high-burden CSVD can be visually evaluated using dynamic intravenous contrast-enhanced MRI.
• This direct, noninvasive technique could serve as a basis for further GMLS studies and could help to explore a new therapeutic target in CSVD patients.





Similar content being viewed by others
Abbreviations
- 3D:
-
Three-dimensional
- BBB:
-
Blood–brain barrier
- BG:
-
Basal ganglia
- BRAVO T1WI:
-
Brain volume T1-weighted imaging
- CSF:
-
Cerebrospinal fluid
- CSVD:
-
Cerebral small-vessel diseases
- DTI-ALPS:
-
Diffusion tensor image analysis along the perivascular spaces
- EPVSs:
-
Enlarged perivascular spaces
- GBCA:
-
Gadolinium-based contrast agent
- GMLS:
-
Glymphatic-meningeal lymphatic system
- mLVs:
-
Meningeal lymphatic vessels
- MMSE:
-
Mini-Mental State Examination
- MoCA:
-
Montreal Cognitive Assessment
- PSQI:
-
Pittsburgh Sleep Quality Index
- RCVS:
-
Reversible cerebral vasoconstriction syndrome
- ROI:
-
Region of interest
- SI:
-
Signal intensity
- SIR:
-
Signal intensity ratio
- SS:
-
Sigmoid sinus
- SSS:
-
Superior sagittal sinus
- T2-FLAIR:
-
T2-fluid attenuated inversion recovery imaging
- TI:
-
Inversion time
- TTP:
-
Time to peak enhancement
References
Rasmussen MK, Mestre H, Nedergaard M (2018) The glymphatic pathway in neurological disorders. Lancet Neurol 17:1016–1024
Mestre H, Kostrikov S, Mehta RI, Nedergaard M (2017) Perivascular spaces, glymphatic dysfunction, and small vessel disease. Clin Sci (Lond) 131:2257–2274
Wardlaw JM, Benveniste H, Nedergaard M et al (2020) Perivascular spaces in the brain: anatomy, physiology and pathology. Nat Rev Neurol 16:137–153
Ahn JH, Cho H, Kim JH et al (2019) Meningeal lymphatic vessels at the skull base drain cerebrospinal fluid. Nature 572:62–66
Louveau A, Smirnov I, Keyes TJ et al (2015) Structural and functional features of central nervous system lymphatic vessels. Nature 523:337–341
Nedergaard M, Goldman SA (2020) Glymphatic failure as a final common pathway to dementia. Science 370:50–56
Gorelick PB, Scuteri A, Black SE et al (2011) Vascular contributions to cognitive impairment and dementia: a statement for healthcare professionals from the american heart association/american stroke association. Stroke 42:2672–2713
Wardlaw JM, Smith EE, Biessels GJ et al (2013) Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol 12:822–838
Pantoni L (2010) Cerebral small vessel disease: from pathogenesis and clinical characteristics to therapeutic challenges. Lancet Neurol 9:689–701
Xue Y, Liu N, Zhang M, Ren X, Tang J, Fu J (2020) Concomitant enlargement of perivascular spaces and decrease in glymphatic transport in an animal model of cerebral small vessel disease. Brain Res Bull 161:78–83
Zhou Y, Cai J, Zhang W et al (2020) Impairment of the glymphatic pathway and putative meningeal lymphatic vessels in the aging human. Ann Neurol 87:357–369
Ding XB, Wang XX, Xia DH et al (2021) Impaired meningeal lymphatic drainage in patients with idiopathic Parkinson’s disease. Nat Med 27:411–418
Mortensen KN, Sanggaard S, Mestre H et al (2019) Impaired glymphatic transport in spontaneously hypertensive rats. J Neurosci 39:6365–6377
Taoka T, Naganawa S (2020) Glymphatic imaging using MRI. J Magn Reson Imaging 51:11–24
Zhang W, Zhou Y, Wang J et al (2021) Glymphatic clearance function in patients with cerebral small vessel disease. Neuroimage 238:118257
Tang J, Zhang M, Liu N et al (2022) The association between glymphatic system dysfunction and cognitive impairment in cerebral small vessel disease. Front Aging Neurosci 14:916633
Wu CH, Lirng JF, Ling YH et al (2021) Noninvasive characterization of human glymphatics and meningeal lymphatics in an in vivo model of blood-brain barrier leakage. Ann Neurol 89:111–124
Naganawa S, Nakane T, Kawai H, Taoka T (2017) Gd-based contrast enhancement of the perivascular spaces in the basal ganglia. Magn Reson Med Sci 16:61–65
Absinta M, Ha SK, Nair G, et al (2017) Human and nonhuman primate meninges harbor lymphatic vessels that can be visualized noninvasively by MRI. Elife.6
Lee MK, Cho SJ, Bae YJ, Kim JM (2022) MRI-based demonstration of the normal glymphatic system in a human population: a systematic review. Front Neurol 13:827398
Lee S, Yoo RE, Choi SH et al (2021) Contrast-enhanced MRI T1 mapping for quantitative evaluation of putative dynamic glymphatic activity in the human brain in sleep-wake states. Radiology 300:661–668
Mijnders LS, Steup FW, Lindhout M, van der Kleij PA, Brink WM, van der Molen AJ (2021) Optimal sequences and sequence parameters for GBCA-enhanced MRI of the glymphatic system: a systematic literature review. Acta Radiol 62:1324–1332
Naganawa S, Taoka T (2022) The glymphatic system: a review of the challenges in visualizing its structure and function with MR imaging. Magn Reson Med Sci 21:182–194
Albayram MS, Smith G, Tufan F et al (2022) Non-invasive MR imaging of human brain lymphatic networks with connections to cervical lymph nodes. Nat Commun 13:203
Deng W, Lin X, Su Y, Cai Y, Zhong J, Ou Y (2022) Comparison between 3D-FLAIR and 3D-real IR MRI sequences with visual classification method in the imaging of endolymphatic hydrops in Meniere’s disease. Am J Otolaryngol 43:103557
Li Y, Li M, Zuo L et al (2018) Compromised blood-brain barrier integrity is associated with total magnetic resonance imaging burden of cerebral small vessel disease. Front Neurol 9:221
Xiao YD, Paudel R, Liu J, Ma C, Zhang ZS, Zhou SK (2016) MRI contrast agents: classification and application (Review). Int J Mol Med 38:1319–1326
Zhang CE, Wong SM, van de Haar HJ et al (2017) Blood-brain barrier leakage is more widespread in patients with cerebral small vessel disease. Neurology 88:426–432
Yang L, Kress BT, Weber HJ et al (2013) Evaluating glymphatic pathway function utilizing clinically relevant intrathecal infusion of CSF tracer. J Transl Med 11:107
Naganawa S, Nakane T, Kawai H, Taoka T (2019) Age dependence of gadolinium leakage from the cortical veins into the cerebrospinal fluid assessed with whole brain 3D-real inversion recovery mr imaging. Magn Reson Med Sci 18:163–169
Naganawa S, Ito R, Kawai H, Taoka T, Yoshida T, Sone M (2020) Confirmation of age-dependence in the leakage of contrast medium around the cortical veins into cerebrospinal fluid after intravenous administration of gadolinium-based contrast agent. Magn Reson Med Sci 19:375–381
Freeze WM, Schnerr RS, Palm WM et al (2017) Pericortical enhancement on delayed postgadolinium fluid-attenuated inversion recovery images in normal aging, mild cognitive impairment, and Alzheimer disease. AJNR Am J Neuroradiol 38:1742–1747
Naganawa S, Ito R, Taoka T, Yoshida T, Sone M (2020) The space between the pial sheath and the cortical venous wall may connect to the meningeal lymphatics. Magn Reson Med Sci 19:1–4
Olate-Briones A, Escalona E, Salazar C et al (2022) The meningeal lymphatic vasculature in neuroinflammation. FASEB J 36:e22276
Da Mesquita S, Louveau A, Vaccari A et al (2018) Functional aspects of meningeal lymphatics in ageing and Alzheimer’s disease. Nature 560:185–191
Liu N, Xue Y, Tang J, Zhang M, Ren X, Fu J (2021) The dynamic change of phenotypic markers of smooth muscle cells in an animal model of cerebral small vessel disease. Microvasc Res 133:104061
Forsberg KME, Zhang Y, Reiners J et al (2018) Endothelial damage, vascular bagging and remodeling of the microvascular bed in human microangiopathy with deep white matter lesions. Acta Neuropathol Commun 6:128
Acknowledgements
We thank Prof. Ding Ding for her help with the statistical analyses in this manuscript.
Funding
This study has received funding by the National Natural Science Foundation of China (81901179).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Jianhui Fu.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
Prof. Ding Ding kindly provided statistical advice for this manuscript.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
The enrolled patients with arteriosclerotic CSVD in the current study were recruited from our registered prospective cohort (registration number: ChiCTR1800017902). The inclusion and exclusion criteria of this cohort have been reported previously (Front Aging Neurosci 2022;14:916633). The methodology in the current study has not been published before.
Methodology
• observational
• performed at one institution
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Miaoyi Zhang and Jie Tang are co-first authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, M., Tang, J., Xia, D. et al. Evaluation of glymphatic-meningeal lymphatic system with intravenous gadolinium-based contrast-enhancement in cerebral small-vessel disease. Eur Radiol 33, 6096–6106 (2023). https://doi.org/10.1007/s00330-023-09796-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-09796-6