Abstract
Objectives
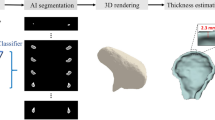
To develop an automated deep-learning algorithm for detection and 3D segmentation of incidental bone lesions in maxillofacial CBCT scans.
Methods
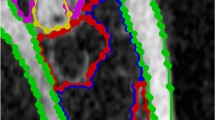
The dataset included 82 cone beam CT (CBCT) scans, 41 with histologically confirmed benign bone lesions (BL) and 41 control scans (without lesions), obtained using three CBCT devices with diverse imaging protocols. Lesions were marked in all axial slices by experienced maxillofacial radiologists. All cases were divided into sub-datasets: training (20,214 axial images), validation (4530 axial images), and testing (6795 axial images). A Mask-RCNN algorithm segmented the bone lesions in each axial slice. Analysis of sequential slices was used for improving the Mask-RCNN performance and classifying each CBCT scan as containing bone lesions or not. Finally, the algorithm generated 3D segmentations of the lesions and calculated their volumes.
Results
The algorithm correctly classified all CBCT cases as containing bone lesions or not, with an accuracy of 100%. The algorithm detected the bone lesion in axial images with high sensitivity (95.9%) and high precision (98.9%) with an average dice coefficient of 83.5%.
Conclusions
The developed algorithm detected and segmented bone lesions in CBCT scans with high accuracy and may serve as a computerized tool for detecting incidental bone lesions in CBCT imaging.
Clinical relevance
Our novel deep-learning algorithm detects incidental hypodense bone lesions in cone beam CT scans, using various imaging devices and protocols. This algorithm may reduce patients’ morbidity and mortality, particularly since currently, cone beam CT interpretation is not always preformed.
Key Points
• A deep learning algorithm was developed for automatic detection and 3D segmentation of various maxillofacial bone lesions in CBCT scans, irrespective of the CBCT device or the scanning protocol.
• The developed algorithm can detect incidental jaw lesions with high accuracy, generates a 3D segmentation of the lesion, and calculates the lesion volume.






Similar content being viewed by others
Abbreviations
- AF:
-
Ameloblastic fibroma
- AI:
-
Artificial intelligence
- AOT:
-
Adenomatoid odontogenic tumor
- BL:
-
Bone lesions
- CAm:
-
Cystic ameloblastoma
- CBCT:
-
Cone beam computerized tomography
- DC:
-
Dentigerous cyst
- Faster RCNN:
-
Faster region-based convolutional neural networks
- FOV:
-
Field of views
- FPN:
-
Feature pyramid network
- IAN:
-
Inferior alverolar nerve
- KOT:
-
Keratocystic odontogenic tumor
- LPC:
-
Lateral periodontal cyst
- N :
-
Number
- NC:
-
Nasopalatine cyst
- OF:
-
Ossifying fibroma
- RC:
-
Radicular cyst
- ROI:
-
Region of interest
- RPN:
-
Region proposal network
- SBC:
-
Simple bone cyst
- SGD:
-
Stochastic gradient descent
- VIA:
-
VGG Image Annotator
- w/o BL:
-
Without bone lesions
References
Gaêta-Araujo H, Alzoubi T, de Faria Vasconcelos K, et al (2020) Cone beam computed tomography in dentomaxillofacial radiology: a two-decade overview. Dentomaxillofac Radiol https://doi.org/10.1259/dmfr.20200145
Kaasalainen T, Ekholm M, Siiskonen T, Kortesniemi M (2021) Dental cone beam CT: an updated review. Phys Med. https://doi.org/10.1016/j.ejmp.2021.07.007
Pauwels R, Araki K, Siewerdsen JH, Thongvigitmanee SS (2015) Technical aspects of dental CBCT: state of the art. Dentomaxillofac Radiol https://doi.org/10.1259/dmfr.20140224
Liang X, Jacobs R, Hassan B, et al (2010) A comparative evaluation of cone beam computed tomography (CBCT) and multi-slice CT (MSCT) part I. On subjective image quality. Eur J Radiol https://doi.org/10.1016/j.ejrad.2009.03.042
Jacobs R, Salmon B, Codari M, Hassan B, Bornstein MM (2018) Cone beam computed tomography in implant dentistry: recommendations for clinical use. BMC Oral Healthhttps://doi.org/10.1186/s12903-018-0523-5
Dawood A, Patel S, Brown J (2009) Cone beam CT in dental practice. Br Dent J https://doi.org/10.1038/sj.bdj.2009.560
Warhekar S, Nagarajappa S, Dasar PL, et al (2015) Incidental findings on cone beam computed tomography and reasons for referral by dental practitioners in Indore city (M.P). J Clin Diagn Res https://doi.org/10.7860/JCDR/2015/11705.5555
Allareddy V, Vincent SD, Hellstein JW, Qian F, Smoker WR, Ruprecht A (2012) Incidental findings on cone beam computed tomography images. Int J Dent. https://doi.org/10.1155/2012/871532
Drage N, Rogers S, Greenall C, Playle R (2013) Incidental findings on cone beam computed tomography in orthodontic patients. J Orthod https://doi.org/10.1179/1465313312Y.0000000027
Lopes IA, Tucunduva RMA, Handem RH, Capelozza ALA (2016) Study of the frequency and location of incidental findings of the maxillofacial region in different fields of view in CBCT scans. Dentomaxillofac Radiol https://doi.org/10.1259/dmfr.20160215
Fiaschetti V, Fanucci E, Rascioni M, Ottria L, Barlattani A, Simonetti G (2010) Jaw expansive lesions: population incidence and CT dentalscan role. Oral Implantol (Rome) 3:2-10
Flaitz CM, Hicks J (2001) Delayed tooth eruption associated with an ameloblastic fibro-odontoma. Pediatr Dent 23:253–254
Araújo JP, Kowalski LP, Rodrigues ML, de Almeida OP, Lopes Pinto CA, Alves FA (2014) Malignant transformation of an odontogenic cyst in a period of 10 years. Case Rep Dent https://doi.org/10.1155/2014/762969
Scarfe WC, Toghyani S, Azevedo B (2018) Imaging of benign odontogenic lesions. Radiol Clin North Am https://doi.org/10.1016/j.rcl.2017.08.004
Yang H, Jo E, Kim HJ, et al (2020) Deep learning for automated detection of cyst and tumors of the jaw in panoramic radiographs. J Clin Med https://doi.org/10.3390/jcm9061839
Jacobs R (2011) Dental cone beam CT and its justified use in oral health care. JBR-BTR. https://doi.org/10.5334/jbr-btr.662
Abdalla-Aslan R, Friedlander-Barenboim S, Aframian DJ, Maly A, Nadler C (2018) Ameloblastoma incidentally detected in cone-beam computed tomography sialography: a case report and review of the literature. J Am Dent Assoc https://doi.org/10.1016/j.adaj.2018.09.003
Heo MS, Kim JE, Hwang JJ, et al (2021) Artificial intelligence in oral and maxillofacial radiology: what is currently possible? Dentomaxillofac Radiol https://doi.org/10.1259/dmfr.20200375
Hung K, Montalvao C, Tanaka R, Kawai T, Bornstein MM (2019) The use and performance of artificial intelligence applications in dental and maxillofacial radiology: a systematic review. Dentomaxillofac Radiol https://doi.org/10.1259/dmfr.20190107
McBee MP, Awan OA, Colucci AT, et al (2018) Deep learning in radiology. Acad Radiol https://doi.org/10.1016/j.acra.2018.02.018
Hwang JJ, Jung YH, Cho BH, Heo MS (2019) An overview of deep learning in the field of dentistry. Imaging Sci Dent https://doi.org/10.5624/isd.2019.49.1.1
Carrillo-Perez F, Pecho OE, Morales JC, et al (2022) Applications of artificial intelligence in dentistry: a comprehensive review. J EsthetRestor Dent https://doi.org/10.1111/jerd.12844
Long J, Shelhamer E, Darrell T (2015) Fully convolutional networks for semantic segmentation. In: 2015 IEEE Conference on Computer Vision and Pattern Recognition (CVPR) https://doi.org/10.1109/CVPR.2015.7298965
Ronneberger O, Fischer P, Brox T (2015) U-net: convolutional networks for biomedical image segmentation. In: Medical image computing and computer-assisted intervention – MICCAI 2015 https://doi.org/10.1007/978-3-319-24574-4_28
Li S, Dong M, Du G, Mu X (2019) Attention Dense-U-Net for automatic breast mass segmentation in digital mammogram. IEEE Access https://doi.org/10.1109/ACCESS.2019.2914873
He K, Gkioxari G, Dollar P, Girshick R (2017) Mask R-CNN. In: Proceedings of the IEEE international conference on computer vision https://doi.org/10.1109/ICCV.2017.322
Kipf TN, Welling M (2016) Semi-supervised classification with graph convolutional networks. arXiv preprint arXiv:1609.02907
Balki I, Amirabadi A, Levman J, et al (2019) Sample-size determination methodologies for machine learning in medical imaging research: a systematic review. Can Assoc Radiol J https://doi.org/10.1016/j.carj.2019.06.002
Dutta A, Zisserman A (2019) The VIA annotation software for images, audio and video. In: Proceedings of the 27th ACM international conference on multimedia https://doi.org/10.1145/3343031.3350535
Ren S, He K, Girshick R, Sun J (2017) Faster R-CNN: towards real-time object detection with region proposal networks. In: IEEE Trans Pattern Anal Mach Intell https://doi.org/10.1109/TPAMI.2016.2577031
Almubarak H, Bazi Y, Alajlan N (2020) Two-stage mask-RCNN approach for detecting and segmenting the optic nerve head, optic disc, and optic cup in fundus images. Appl Sci https://doi.org/10.3390/app10113833
Lin TY, Maire M, Belongie S, et al (2014) In: Computer vision – ECCV 2014. Lecture Notes in Computer Science, https://doi.org/10.1007/978-3-319-10602-1_48
Ketkar N (2017) Stochastic gradient descent. In: Deep learning with Python. Apress, Berkeley, CA https://doi.org/10.1007/978-1-4842-2766-4_8
Shamir RR, Duchin Y, Kim J, Sapiro G, Harel N (2019) Continuous dice coefficient: a method for evaluating probabilistic segmentations. BioRxivhttps://doi.org/10.1101/306977
Ariji Y, Yanashita Y, Kutsuna S, et al (2019) Automatic detection and classification of radiolucent lesions in the mandible on panoramic radiographs using a deep learning object detection technique. Oral Surg Oral Med Oral Pathol Oral Radiol https://doi.org/10.1016/j.oooo.2019.05.014
Yilmaz E, Kayikcioglu T, Kayipmaz S (2017) Computer-aided diagnosis of periapical cyst and keratocystic odontogenic tumor on cone beam computed tomography. Comput Methods Programs Biomed https://doi.org/10.1016/j.cmpb.2017.05.012
Okada K, Rysavy S, Flores A, Linguraru MG (2015) Noninvasive differential diagnosis of dental periapical lesions in cone-beam CT scans. Med Phys https://doi.org/10.1118/1.4914418
Lee JH, Kim DH, Jeong SN (2020) Diagnosis of cystic lesions using panoramic and cone beam computed tomographic images based on deep learning neural network. Oral Dis https://doi.org/10.1111/odi.13223
Setzer FC, Shi KJ, Zhang Z, et al (2020) Artificial intelligence for the computer-aided detection of periapical lesions in cone-beam computed tomographic images. J Endod https://doi.org/10.1016/j.joen.2020.03.025
Orhan K, Bayrakdar IS, Ezhov M, Kravtsov A, Özyürek T (2020) Evaluation of artificial intelligence for detecting periapical pathosis on cone-beam computed tomography scans. Int Endod J https://doi.org/10.1111/iej.13265
Ezhov M, Gusarev M, Golitsyna M, et al (2021) Clinically applicable artificial intelligence system for dental diagnosis with CBCT. Sci Rep https://doi.org/10.1038/s41598-021-94093-9
Kirnbauer B, Hadzic A, Jakse N, Bischof H, Stern D (2022) Automatic detection of periapical osteolytic lesions on cone-beam computed tomography using deep convolutional neuronal networks. J Endod https://doi.org/10.1016/j.joen.2022.07.013
Abdolali F, Zoroofi RA, Otake Y, Sato Y (2017) Automated classification of maxillofacial cysts in cone beam CT images using contourlet transformation and Spherical Harmonics. Comput Methods Programs Biomed. https://doi.org/10.1016/j.cmpb.2016.10.024
Abdolali F, Zoroofi RA, Otake Y, Sato Y (2016) Automatic segmentation of maxillofacial cysts in cone beam CT images. Comput Biol Med. https://doi.org/10.1016/j.compbiomed.2016.03.014
Brown J, Jacobs R, LevringJäghagen E, et al (2014) Basic training requirements for the use of dental CBCT by dentists: a position paper prepared by the European Academy of Dento Maxillo Facial Radiology. Dentomaxillofac Radiol https://doi.org/10.1259/dmfr.20130291
Pohlenz P, Gröbe A, Petersik A, et al (2010) Virtual dental surgery as a new educational tool in dental school. J Craniomaxillofac Surg. https://doi.org/10.1016/j.jcms.2010.02.011
Acknowledgements
We would like to acknowledge the late Prof. Isaac Leichter, who has left us unexpectedly, while still in his productive years. Prof. Leichter was a great medical physicist, researcher, and one-of-a-kind teacher and mentor. He had numerous projects throughout his lifetime, some of which are now being completed by his colleagues, in his spirit. Above all, he was kind and modest.
May he rest in peace.
Funding
This study has received only internal funding by The Jerusalem College of Technology.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dr. Nadler Chen.
Conflict of Interest
The authors declare no competing interests.
Statistics and Biometry
One of the authors (Dr. Talia Yeshua) has significant statistical expertise.
Informed Consent
Written informed consent was waived by the Institutional Review Board.
Ethical Approval
Institutional Review Board approval was obtained (HMO-0297-21).
Methodology
• This is a retrospective
• case-control observational AI study
• preformed in one institute.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This work has been part of the DMD research study of the student, Amal Abu-Nasser, in the Hadassah Faculty of Dental Medicine, Jerusalem, Israel.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yeshua, T., Ladyzhensky, S., Abu-Nasser, A. et al. Deep learning for detection and 3D segmentation of maxillofacial bone lesions in cone beam CT. Eur Radiol 33, 7507–7518 (2023). https://doi.org/10.1007/s00330-023-09726-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-09726-6