Abstract
Objectives
To develop an artificial intelligence (AI) model for prostate segmentation and prostate cancer (PCa) detection, and explore the added value of AI-based computer-aided diagnosis (CAD) compared to conventional PI-RADS assessment.
Methods
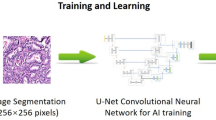
A retrospective study was performed on multi-centers and included patients who underwent prostate biopsies and multiparametric MRI. A convolutional-neural-network-based AI model was trained and validated; the reliability of different CAD methods (concurrent read and AI-first read) were tested in an internal/external cohort. The diagnostic performance, consistency and efficiency of radiologists and AI-based CAD were compared.
Results
The training/validation/internal test sets included 650 (400/100/150) cases from one center; the external test included 100 cases (25/25/50) from three centers. For diagnosis accuracy, AI-based CAD methods showed no significant differences and were equivalent to the radiologists in the internal test (127/150 vs. 130/150 vs. 125/150 for reader 1; 127/150 vs.132/150 vs. 131/150 for reader 2; all p > 0.05), whereas in the external test, concurrent-read methods were superior/equal to AI-first read (87/100 vs. 71/100, p < 0.001, for reader 2; 79/100 vs. 69/100, p = 0.076, for reader 1) and better than/equal to radiologists (79/100 vs. 72/100, p = 0.039, for reader 1; 87/100 vs. 86/100, p = 1.000, for reader 2). Moreover, AI-first read/concurrent read improved consistency in both internal test (κ = 1.000, 0.830) and external test (κ = 0.958, 0.713) compared to radiologists (κ = 0.747, 0.600); AI-first read method (8.54 s/7.66 s) was faster than readers (92.72 s/89.54 s) and concurrent-read method (29.15 s/28.92 s), respectively.
Conclusion
AI-based CAD could improve the consistency and efficiency for accurate diagnosis; the concurrent-read method could enhance the diagnostic capabilities of an inexperienced radiologist in unfamiliar situations.
Key Points
• For prostate cancer segmentation, the performance of multi-small Vnet displays optimal compared to small Vnet and Vnet (DSC msvnet vs. DSC svnet , p = 0.021; DSC msvnet vs. DSC vnet , p < 0.001).
• For prostate gland segmentation, the mean/median DSCs for fine and coarse segmentation were 0.91/0.91 and 0.88/0.89, respectively. Fine segmentation displays superior performance compared to coarse (DSC coarse vs. DSC fine , p < 0.001).
• For PCa diagnosis, AI-based CAD methods improve consistency in internal (κ = 1.000; 0.830) and external (κ = 0.958; 0.713) tests compared to radiologists (κ = 0.747; 0.600); the AI-first read (8.54 s/7.66 s) was faster than the readers (92.72 s/89.54 s) and the concurrent-read method (29.15 s/28.92 s).






Similar content being viewed by others
Data Availability
The data that support the findings of this study are available from the corresponding author, [Guangyu Wu], upon reasonable request.
Abbreviations
- AI:
-
Artificial intelligence
- CAD:
-
Computer-aided diagnosis
- csPCa:
-
Clinically significant prostate cancer
- DSC:
-
Dice similarity coefficient
- FNR:
-
False-negative rate
- FPR:
-
False-positive rate
- GS:
-
Gleason score
- msVnet:
-
Multi-small Vnet
- PCa:
-
Prostate cancer
- PI-RADS:
-
Prostate Imaging Reporting and Data System
- sVnet:
-
Small Vnet
References
van der Leest M, Cornel E, Israël B et al (2019) Head-to-head comparison of transrectal ultrasound-guided prostate biopsy versus multiparametric prostate resonance imaging with subsequent magnetic resonance-guided biopsy in biopsy-naïve men with elevated prostate-specific antigen: a large prospective multicenter clinical study. Eur Urol 75(4):570–578
Turkbey B, Rosenkrantz AB, Haider MA (2019) Prostate Imaging Reporting and Data System Version 2.1, et al (2019) update of Prostate Imaging Reporting and Data System Version 2. Eur Urol 76(3):340–351
Smith CP, Harmon SA, Barrett T et al (2019) Intra- and interreader reproducibility of PI-RADSv2: a multireader study. J Magn Reson Imaging 49(6):1694–1703
Westphalen AC, McCulloch CE, Anaokar JM et al (2020) Variability of the positive predictive value of PI-RADS for prostate MRI across 26 centers: experience of the Society of Abdominal Radiology Prostate Cancer disease-focused panel. Radiology 296(1):76–84
Sathianathen NJ, Omer A, Harriss E et al (2020) Negative predictive value of multiparametric magnetic resonance imaging in the detection of clinically significant prostate cancer in the Prostate Imaging Reporting and Data System era: a systematic review and meta-analysis. Eur Urol 78(3):402–414
Cuocolo R, Cipullo MB, Stanzione A et al (2020) Machine learning for the identification of clinically significant prostate cancer on MRI: a meta-analysis. Eur Radiol 30(12):6877–6887
Cao R, Mohammadian Bajgiran A, Afshari Mirak S et al (2019) Joint prostate cancer detection and Gleason score prediction in mp-MRI via FocalNet. IEEE Trans Med Imaging 38(11):2496–2506
Bhattacharya A, Seetharaman W, Shao R, et al (2020) CorrSigNet: learning CORRelated Prostate Cancer SIGnatures from radiology and pathology images for improved computer aided diagnosis, MICCAI
Arif M, Schoots IG, Castillo Tovar J et al (2020) Clinically significant prostate cancer detection and segmentation in low-risk patients using a convolutional neural network on multi-parametric MRI. Eur Radiol 30(12):6582–6592
Netzer N, Weißer C, Schelb P et al (2021) Fully automatic deep learning in bi-institutional prostate magnetic resonance imaging: effects of cohort size and heterogeneity. Invest Radiol. https://doi.org/10.1097/RLI.0000000000000791
Seetharaman A, Bhattacharya I, Chen LC et al (2021) Automated detection of aggressive and indolent prostate cancer on magnetic resonance imaging. Med Phys 48(6):2960–2972
Greer MD, Lay N, Shih JH et al (2018) Computer-aided diagnosis prior to conventional interpretation of prostate mpMRI: an international multi-reader study. Eur Radiol 28(10):4407–4417
Fujita H (2020) AI-based computer-aided diagnosis (AI-CAD): the latest review to read first. Radiol Phys Technol 13(1):6–19
Mottet N, Van den Bergh R, Briers EJEU (2019) EAU guidelines: prostate cancer 2019. Eur Urol 76:868–873
Milletari, Fausto, Nassir Navab, Seyed-Ahmad Ahmadi (2016) Vnet: fully convolutional neural networks for volumetric medical image segmentation. 2016 Fourth International Conference on 3D Vision (3DV), Stanford CA USA
Klein S, Staring M, Murphy K, Viergever MA, Pluim JP (2010) Elastix: a toolbox for intensity-based medical image registration. IEEE Trans Med Imaging 29:196–205
Kingma D , Ba J (2014) Adam: a method for stochastic optimization. CoRR, abs/1412.6980
Deal M, Bardet F, Walker PM, et al (2021) Three-dimensional nuclear magnetic resonance spectroscopy: a complementary tool to multiparametric magnetic resonance imaging in the identification of aggressive prostate cancer at 3.0T. Quant Imaging Med Surg 1(8):3749–3766
Huebner NA, Korn S, Resch I et al (2021) Visibility of significant prostate cancer on multiparametric magnetic resonance imaging (MRI)-do we still need contrast media? Eur Radiol 31(6):3754–3764
Yao W, Zheng J, Han C et al (2021) Integration of quantitative diffusion kurtosis imaging and prostate specific antigen in differential diagnostic of prostate cancer. Medicine (Baltimore) 100(35):e27144
Zech JR, Badgeley MA, Liu M, Costa AB, Titano JJ, Oermann EK (2018) Variable generalization performance of a deep learning model to detect pneumonia in chest radiographs: a cross-sectional study. PLoS Med 15(11):e1002683. Published 2018 Nov 6
Christ PF, Elshaer MEA, Ettlinger F, et al (2016) Automatic liver and lesion segmentation in CT using cascaded fully convolutional neural networks and 3D conditional random fields. Paper presented at: International Conference on Medical Image Computing and Computer-Assisted Intervention 415–423. https://doi.org/10.1007/978-3-319-46723-8_48
Zhou ZH (2012) Ensemble methods: foundations and algorithms. CRC Press, Boca Raton
Sheng VS, Provost FJ, Ipeirotis PG (2008) Get another label? Improving data quality and data mining using multiple, noisy labelers. In 14th ACM SIGKDD International Conference on Knowledge Discovery and Data Mining, Las Vegas, NV, 614–622
Snow R, O’Connor B, Jurafsky D et al (2008) Cheap and fast - but is it good? Evaluating non-expert annotations for natural language tasks. In 2008 Conference on Empirical Methods in Natural Language Processing, Honolulu, HI, 254–263
Chakraborty DP (2013) A brief history of free-response receiver operating characteristic paradigm data analysis. Acad Radiol 20(7):915–919
Zou KH, Liu A, Bandos AI, Ohno-Machado L, Rockette HE (2012) Statistical evaluation of diagnostic performance: topics in ROC analysis. Boca Raton, FL: Chapman & Hall 54(4):509–510
Gur D, Rockette HE (2018) Performance assessments of diagnostic systems under the FROC paradigm: experimental, analytical, and results interpretation issues. Acad Radio 15(10):1312–1315
Esses SJ, Taneja SS, Rosenkrantz AB (2018) Imaging facilities’ adherence to PI-RADS v2 minimum technical standards for the performance of prostate MRI. Acad Radiol 25(2):188–195
Cuocolo R, Stanzione A, Ponsiglione A, et al (2019) Prostate MRI technical parameters standardization: a systematic review on adherence to PI-RADSv2 acquisition protocol. Eur J Radiol. 120:108662. https://doi.org/10.1016/j.ejrad.2019.108662.
Acknowledgements
The authors thank Dr. Yinjie Zhu for his clinical contribution to the study and Dr. Zizhou Zhao, Li Zhu for sharing their expertise.
Funding
This study was supported by the National Natural Science Foundation of China (grant numbers 81601487, 81601453), the Shanghai Jiao Tong University Medical Engineering Cross Fund (grant number YG2021QN27), the Shanghai Municipal Commission of Economy and Informatization (grant number 2019-RGZN-01094), Transverse Project from Renji Hospital, School of Medicine, Shanghai Jiao Tong University (grant number RJKY22-004), the Science and Technology Commission of Shanghai Municipality (grant number 18DZ1930104), and the Shanghai Pujiang Program (grant number 19PJ1431900).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Guangyu Wu, PhD.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the institutional review boards.
Ethical approval
This study was approved by the Ethics Committee of Renji Hospital (approval number: KY2018-212); the Ethics Committee of Huangpu Branch, Shanghai Ninth People’s Hospital (approval number: 2020-KYXM-134); the Ethics Committee of Putuo Hospital, Shanghai University of Traditional Chinese Medicine (approval number: 2019FYJ011); and the Ethics Committee of Affiliated Hospital of Nanjing University of Chinese Medicine (approval number: 2019NL-178-22).
Methodology
• retrospective
• diagnostic or prognostic study
• multicenter study
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, G., Pan, S., Zhao, R. et al. The added value of AI-based computer-aided diagnosis in classification of cancer at prostate MRI. Eur Radiol 33, 5118–5130 (2023). https://doi.org/10.1007/s00330-023-09433-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-09433-2