Abstract
Objectives
To examine the value of 3-T MRI for evaluating the difference between the pancreatic parenchyma of intraductal papillary mucinous neoplasm with a concomitant invasive carcinoma (IPMN-IC) and the pancreatic parenchyma of patients without an IPMN-IC.
Methods
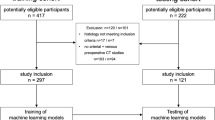
A total of 132 patients underwent abdominal 3-T MRI. Of the normal pancreatic parenchymal measurements, the pancreas-to-muscle signal intensity ratio in in-phase imaging (SIR-I), SIR in opposed-phase imaging (SIR-O), SIR in T2-weighted imaging (SIR-T2), ADC (×10−3 mm2/s) in DWI, and proton density fat fraction (PDFF [%]) in multi-echo 3D DIXON were calculated. The patients were divided into three groups (normal pancreas group: n = 60, intraductal papillary mucinous neoplasm (IPMN) group: n = 60, IPMN-IC group: n = 12).
Results
No significant differences were observed among the three groups in age, sex, body mass index, prevalence of diabetes mellitus, and hemoglobin A1c (p = 0.141 to p = 0.657). In comparisons among the three groups, the PDFF showed a significant difference (p < 0.001), and there were no significant differences among the three groups in SIR-I, SIR-O, SIR-T2, and ADC (p = 0.153 to p = 0.684). The PDFF of the pancreas was significantly higher in the IPMN-IC group than in the normal pancreas group or the IPMN group (p < 0.001 and p < 0.001, respectively), with no significant difference between the normal pancreas group and the IPMN group (p = 0.916).
Conclusions
These observations suggest that the PDFF of the pancreas is associated with the presence of IPMN-IC.
Key Points
• The cause and risk factors of IPMN with a concomitant invasive carcinoma have not yet been clarified.
• The PDFF of the pancreas was significantly higher in the IPMN-IC group than in the normal pancreas group or the IPMN group.
• Pancreatic PDFF may be a potential biomarker for the development of IPMN with a concomitant invasive carcinoma.




Similar content being viewed by others
Abbreviations
- BMI:
-
Body mass index
- DM:
-
Diabetes mellitus
- FOV:
-
Field of view
- HbA1c:
-
Hemoglobin A1c
- IPMN:
-
Intraductal papillary mucinous neoplasm
- IPMN-IC:
-
Intraductal papillary mucinous neoplasm with a concomitant invasive carcinoma
- PACS:
-
Picture archiving and communication system
- PDAC:
-
Pancreatic ductal adenocarcinoma
- PDFF:
-
Proton density fat fraction
- SIR:
-
Signal intensity ratio
- SIR-I:
-
Signal intensity ratio in in-phase imaging
- SIR-O:
-
Signal intensity ratio in opposed-phase imaging
- SIR-T2:
-
Signal intensity ratio in T2-weighted imaging
- T1WI:
-
T1-weighted imaging
- T2WI:
-
T2-weighted imaging
- TE:
-
Echo time
- TR:
-
Repetition time
- TSE:
-
Turbo spin echo
References
Kashiwagi K, Seino T, Fukuhara S et al (2018) Pancreatic fat content detected by computed tomography and its significant relationship with intraductal papillary mucinous neoplasm. Pancreas. 47(9):1087–1092
Yamaguchi K, Kanemitsu S, Hatori T et al (2011) Pancreatic ductal adenocarcinoma derived from IPMN and pancreatic ductal adenocarcinoma concomitant with IPMN. Pancreas. 40(4):571–580
Baiocchi GL, Molfino S, Frittoli B et al (2015) Increased risk of second malignancy in pancreatic intraductal papillary mucinous tumors: review of the literature. World J Gastroenterol. 21(23):7313–7319
Omori Y, Ono Y, Tanino M et al (2019) Pathways of progression from intraductal papillary mucinous neoplasm to pancreatic ductal adenocarcinoma based on molecular features. Gastroenterology 156(3):647–61.e2
Kanno A, Satoh K, Hirota M et al (2010) Prediction of invasive carcinoma in branch type intraductal papillary mucinous neoplasms of the pancreas. J Gastroenterol. 45(9):952–959
Yamaguchi K, Ohuchida J, Ohtsuka T, Nakano K, Tanaka M (2002) Intraductal papillary-mucinous tumor of the pancreas concomitant with ductal carcinoma of the pancreas. Pancreatology. 2(5):484–490
Kamisawa T, Tu Y, Egawa N, Nakajima H, Tsuruta K, Okamoto A (2005) Malignancies associated with intraductal papillary mucinous neoplasm of the pancreas. World J Gastroenterol. 11(36):5688–5690
Kawakami S, Fukasawa M, Shimizu T et al (2019) Diffusion-weighted image improves detectability of magnetic resonance cholangiopancreatography for pancreatic ductal adenocarcinoma concomitant with intraductal papillary mucinous neoplasm. Medicine (Baltimore). 98(47):e18039
Yagi Y, Masuda A, Zen Y et al (2018) Pancreatic inflammation and atrophy are not associated with pancreatic cancer concomitant with intraductal papillary mucinous neoplasm. Pancreatology. 18(1):54–60
Kawada N, Uehara H, Nagata S, Tsuchishima M, Tsutsumi M, Tomita Y (2015) Imaging morphological changes of intraductal papillary mucinous neoplasm of the pancreas was associated with its malignant transformation but not with development of pancreatic ductal adenocarcinoma. Pancreatology. 15(6):654–660
Ikegawa T, Masuda A, Sakai A et al (2018) Multifocal cysts and incidence of pancreatic cancer concomitant with intraductal papillary mucinous neoplasm. Pancreatology. 18(4):399–406
Ingkakul T, Sadakari Y, Ienaga J, Satoh N, Takahata S, Tanaka M (2010) Predictors of the presence of concomitant invasive ductal carcinoma in intraductal papillary mucinous neoplasm of the pancreas. Ann Surg. 251(1):70–75
Kobayashi G, Fujita N, Maguchi H et al (2014) Natural history of branch duct intraductal papillary mucinous neoplasm with mural nodules: a Japan Pancreas Society multicenter study. Pancreas. 43(4):532–538
Uehara H, Nakaizumi A, Ishikawa O et al (2008) Development of ductal carcinoma of the pancreas during follow-up of branch duct intraductal papillary mucinous neoplasm of the pancreas. Gut. 57(11):1561–1565
Tanaka M, Fernández-Del Castillo C, Kamisawa T et al (2017) Revisions of international consensus Fukuoka guidelines for the management of IPMN of the pancreas. Pancreatology. 17(5):738–753
Fukui H, Hori M, Fukuda Y et al (2019) Evaluation of fatty pancreas by proton density fat fraction using 3-T magnetic resonance imaging and its association with pancreatic cancer. Eur J Radiol. 118:25–31
Rebours V, Gaujoux S, d'Assignies G et al (2015) Obesity and fatty pancreatic infiltration are risk factors for pancreatic precancerous lesions (PanIN). Clin Cancer Res. 21(15):3522–3528
Hori M, Takahashi M, Hiraoka N et al (2014) Association of pancreatic fatty infiltration with pancreatic ductal adenocarcinoma. Clin Transl Gastroenterol 5(3):e53-e
Lesmana CRA, Gani RA, Lesmana LA (2018) Non-alcoholic fatty pancreas disease as a risk factor for pancreatic cancer based on endoscopic ultrasound examination among pancreatic cancer patients: a single-center experience. JGH Open. 2(1):4–7
Fukuda Y, Yamada D, Eguchi H et al (2017) CT Density in the pancreas is a promising imaging predictor for pancreatic ductal adenocarcinoma. Ann Surg Oncol. 24(9):2762–2769
Majumder S, Philip NA, Takahashi N, Levy MJ, Singh VP, Chari ST (2017) Fatty pancreas: should we be concerned? Pancreas. 46(10):1251–1258
Tomita Y, Azuma K, Nonaka Y et al (2014) Pancreatic fatty degeneration and fibrosis as predisposing factors for the development of pancreatic ductal adenocarcinoma. Pancreas. 43(7):1032–1041
Takahashi M, Hori M, Ishigamori R, Mutoh M, Imai T, Nakagama H (2018) Fatty pancreas: a possible risk factor for pancreatic cancer in animals and humans. Cancer Sci. 109(10):3013–3023
Murakami Y, Uemura K, Sudo T et al (2009) Invasive intraductal papillary-mucinous neoplasm of the pancreas: comparison with pancreatic ductal adenocarcinoma. J Surg Oncol. 100(1):13–18
Tanno S, Nakano Y, Koizumi K et al (2010) Pancreatic ductal adenocarcinomas in long-term follow-up patients with branch duct intraductal papillary mucinous neoplasms. Pancreas. 39(1):36–40
Ideno N, Ohtsuka T, Kono H et al (2013) Intraductal papillary mucinous neoplasms of the pancreas with distinct pancreatic ductal adenocarcinomas are frequently of gastric subtype. Ann Surg. 258(1):141–151
Beller E, Lorbeer R, Keeser D et al (2019) Hepatic fat is superior to BMI, visceral and pancreatic fat as a potential risk biomarker for neurodegenerative disease. Eur Radiol. 29(12):6662–6670
Kühn JP, Berthold F, Mayerle J et al (2015) Pancreatic steatosis demonstrated at mr imaging in the general population: clinical relevance. Radiology. 276(1):129–136
Kromrey ML, Friedrich N, Hoffmann RT et al (2019) Pancreatic steatosis is associated with impaired exocrine pancreatic function. Invest Radiol. 54(7):403–408
Aliyari Ghasabeh M, Shaghaghi M, Khoshpouri P et al (2020) Correlation between incidental fat deposition in the liver and pancreas in asymptomatic individuals. Abdom Radiol (NY). 45(1):203–210
Lesmana CR, Pakasi LS, Inggriani S, Aidawati ML, Lesmana LA (2015) Prevalence of non-alcoholic fatty pancreas disease (NAFPD) and its risk factors among adult medical check-up patients in a private hospital: a large cross sectional study. BMC Gastroenterol. 15:174
Zhang Y, Wang C, Duanmu Y et al (2018) Comparison of CT and magnetic resonance mDIXON-Quant sequence in the diagnosis of mild hepatic steatosis. Br J Radiol. 91(1091):20170587
Lee SS, Park SH (2014) Radiologic evaluation of nonalcoholic fatty liver disease. World J Gastroenterol. 20(23):7392–7402
Yokoo T, Bydder M, Hamilton G et al (2009) Nonalcoholic fatty liver disease: diagnostic and fat-grading accuracy of low-flip-angle multiecho gradient-recalled-echo MR imaging at 1.5 T. Radiology. 251(1):67–76
Hayashi T, Fukuzawa K, Yamazaki H et al (2018) Multicenter, multivendor phantom study to validate proton density fat fraction and T2* values calculated using vendor-provided 6-point DIXON methods. Clin Imaging. 51:38–42
Serai SD, Dillman JR, Trout AT (2017) Proton density fat fraction measurements at 1.5- and 3-T hepatic MR imaging: same-day agreement among readers and across two imager manufacturers. Radiology. 284(1):244–254
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Tsutomu Tamada.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• observational
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
About this article
Cite this article
Sotozono, H., Kanki, A., Yasokawa, K. et al. Value of 3-T MR imaging in intraductal papillary mucinous neoplasm with a concomitant invasive carcinoma. Eur Radiol 32, 8276–8284 (2022). https://doi.org/10.1007/s00330-022-08881-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-022-08881-6