Abstract
Objectives
To investigate useful MRI features in pancreatic neuroendocrine tumor (PNET) patients for predicting recurrence and its timing after surgery.
Methods
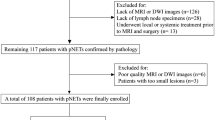
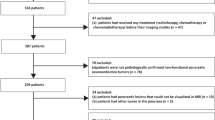
A total of 99 patients with PNET who underwent MRI and surgery from 2000 to 2018 were enrolled. Two radiologists independently assessed MRI findings, including size, location, margin, T1 and T2 signal intensity, enhancement patterns, common bile duct (CBD) or main pancreatic duct (MPD) dilatation, vascular invasion, lymph node enlargement, DWI, and ADC value. Imaging findings associated with recurrence and disease-free survival (DFS) were assessed using logistic regression analysis and Cox proportional hazard regression analysis.
Results
The median follow-up period was 40.4 months, and recurrence after surgery occurred in 12.1% (12/99). Among them, 6 patients experienced recurrence within 1 year, and 9 patients experienced recurrence within 2 years after surgery. In multivariate analysis, major venous invasion (OR 10.76 [1.14–101.85], p = 0.04) was associated with recurrence within 1 year, and portal phase iso- to hypoenhancement (OR 51.89 [1.73–1557.89], p = 0.02), CBD or MPD dilatation (OR 10.49 [1.35–81.64], p = 0.03) and larger size (OR 1.05 [1.00–1.10], p = 0.046) were associated with recurrence within 2 years. The mean DFS was 116.4 ± 18.5 months, and the 5-year DFS rate was 85.7%. In multivariate analysis, portal phase iso- to hypoenhancement (HR 21.36 [2.01–197.77], p = 0.01), ductal dilatation (HR 5.22 [1.46–18.68], p = 0.01), major arterial invasion (HR 42.90 [3.66–502.48], p = 0.003), and larger size (HR 1.04 [1.01–1.06], p = 0.01) showed a significant effect on poor DFS.
Conclusion
MRI features, including size, enhancement pattern, vascular invasion, and ductal dilatation, are useful in predicting recurrence and poor DFS after surgery in PNET.
Key Points
• MRI features are useful for predicting prognosis in patients with PNET after surgery.
• PV or SMV invasion (OR 10.49 [1.35–81.64], p = 0.04) was significantly associated with 1-year recurrence.
• Portal phase iso- to hypoenhancement (HR 21.36), CBD or MPD dilatation (HR 5.22), arterial invasion (HR 42.90), and larger size (HR 1.04) had significant effects on poor DFS (p < 0.05).




Similar content being viewed by others
Abbreviations
- CA:
-
Celiac axis
- CBD:
-
Common bile duct
- CI:
-
Confidence interval
- DFS:
-
Disease-free survival
- HR:
-
Hazard ratio
- LN:
-
Lymph node
- MPD:
-
Main pancreatic duct
- OR:
-
Odds ratio
- PNET:
-
Pancreatic neuroendocrine tumor
- PV:
-
Portal vein
- SMA:
-
Superior mesenteric artery
- SMV:
-
Superior mesenteric vein
References
Fraenkel M, Kim MK, Faggiano A, Valk GD (2012) Epidemiology of gastroenteropancreatic neuroendocrine tumours. Best Pract Res Clin Gastroenterol 26:691–703
Lawrence B, Gustafsson BI, Chan A, Svejda B, Kidd M, Modlin IM (2011) The epidemiology of gastroenteropancreatic neuroendocrine tumors. Endocrinol Metab Clin North Am 40(1–18):vii
Dasari A, Shen C, Halperin D et al (2017) Trends in the incidence, prevalence, and survival outcomes in patients with neuroendocrine tumors in the United States. JAMA Oncol 3:1335–1342
Shah M, Goldner W, Halfdanarson T et al (2018) NCCN clinical practice guidelines in oncology: neuroendocrine and adrenal tumors. J Natl Compr Cancer Netw 16:693–702
Kunz PL, Reidy-Lagunes D, Anthony LB et al (2013) Consensus guidelines for the management and treatment of neuroendocrine tumors. Pancreas 42:557–577
Rindi G, Falconi M, Klersy C et al (2012) TNM staging of neoplasms of the endocrine pancreas: results from a large international cohort study. J Natl Cancer Inst 104:764–777
Genç CG, Falconi M, Partelli S et al (2018) Recurrence of pancreatic neuroendocrine tumors and survival predicted by Ki67. Ann Surg Oncol 25:2467–2474
Kim H, Song KB, Hwang DW, Lee JH, Alshammary S, Kim SC (2019) Time-trend and recurrence analysis of pancreatic neuroendocrine tumors. Endocr Connect 8:1052–1060
Canellas R, Lo G, Bhowmik S, Ferrone C, Sahani D (2018) Pancreatic neuroendocrine tumor: correlations between MRI features, tumor biology, and clinical outcome after surgery. J Magn Reson Imaging 47:425–432
Guo C, Chen X, Xiao W, Wang Q, Sun K, Wang Z (2017) Pancreatic neuroendocrine neoplasms at magnetic resonance imaging: comparison between grade 3 and grade 1/2 tumors. Onco Targets Ther 10:1465–1474
Kang J, Ryu JK, Son JH et al (2018) Association between pathologic grade and multiphase computed tomography enhancement in pancreatic neuroendocrine neoplasm. J Gastroenterol Hepatol. https://doi.org/10.1111/jgh.14139
Takumi K, Fukukura Y, Higashi M et al (2015) Pancreatic neuroendocrine tumors: correlation between the contrast-enhanced computed tomography features and the pathological tumor grade. Eur J Radiol 84:1436–1443
Toshima F, Inoue D, Komori T et al (2017) Is the combination of MR and CT findings useful in determining the tumor grade of pancreatic neuroendocrine tumors? Jpn J Radiol 35:242–253
Kim DW, Kim DW, Kim HJ et al (2015) Neuroendocrine neoplasms of the pancreas at dynamic enhanced CT: comparison between grade 3 neuroendocrine carcinoma and grade 1/2 neuroendocrine tumour. Eur Radiol 25:1375–1383
Lewis RB, Lattin GE Jr, Paal E (2010) Pancreatic endocrine tumors: radiologic-clinicopathologic correlation. Radiographics 30:1445–1464
d’Assignies G, Couvelard A, Bahrami S et al (2009) Pancreatic endocrine tumors: tumor blood flow assessed with perfusion CT reflects angiogenesis and correlates with prognostic factors
Kim JH, Eun HW, Kim YJ, Lee JM, Han JK, Choi BI (2016) Pancreatic neuroendocrine tumour (PNET): staging accuracy of MDCT and its diagnostic performance for the differentiation of PNET with uncommon CT findings from pancreatic adenocarcinoma. Eur Radiol 26:1338–1347
Worhunsky DJ, Krampitz GW, Poullos PD et al (2014) Pancreatic neuroendocrine tumours: hypoenhancement on arterial phase computed tomography predicts biological aggressiveness. HPB (Oxford) 16:304–311
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Dioguardi Burgio M, Cros J, Panvini N et al (2021) Serotonin immunoreactive pancreatic neuroendocrine neoplasm associated with main pancreatic duct dilation: a recognizable entity with excellent long-term outcome. Eur Radiol. https://doi.org/10.1007/s00330-021-08007-4
Kawamoto S, Shi C, Hruban RH et al (2011) Small serotonin-producing neuroendocrine tumor of the pancreas associated with pancreatic duct obstruction. AJR Am J Roentgenol 197:W482-488
Zandee WT, van Adrichem RC, Kamp K, Feelders RA, van Velthuysen MF, de Herder WW (2017) Incidence and prognostic value of serotonin secretion in pancreatic neuroendocrine tumours. Clin Endocrinol (Oxf) 87:165–170
Kim C, Byun JH, Hong SM et al (2017) A comparison of enhancement patterns on dynamic enhanced CT and survival between patients with pancreatic neuroendocrine tumors with and without intratumoral fibrosis. Abdom Radiol (NY) 42:2835–2842
Marion-Audibert AM, Barel C, Gouysse G et al (2003) Low microvessel density is an unfavorable histoprognostic factor in pancreatic endocrine tumors. Gastroenterology 125:1094–1104
Rodallec M, Vilgrain V, Couvelard A et al (2006) Endocrine pancreatic tumours and helical CT: contrast enhancement is correlated with microvascular density, histoprognostic factors and survival. Pancreatology 6:77–85
Guo C, Zhuge X, Chen X, Wang Z, Xiao W, Wang Q (2017) Value of diffusion-weighted magnetic resonance imaging in predicting World Health Organization grade in G1/G2 pancreatic neuroendocrine tumors. Oncol Lett 13:4141–4146
Bettini R, Partelli S, Boninsegna L et al (2011) Tumor size correlates with malignancy in nonfunctioning pancreatic endocrine tumor. Surgery 150:75–82
Manfredi R, Bonatti M, Mantovani W et al (2013) Non-hyperfunctioning neuroendocrine tumours of the pancreas: MR imaging appearance and correlation with their biological behaviour. Eur Radiol 23:3029–3039
Canellas R, Burk KS, Parakh A, Sahani DV (2018) Prediction of pancreatic neuroendocrine tumor grade based on CT features and texture analysis. AJR Am J Roentgenol 210:341–346
Chun YS, Pawlik TM, Vauthey JN (2018) 8th edition of the AJCC cancer staging manual: pancreas and hepatobiliary cancers. Ann Surg Oncol 25:845–847
Rindi G (2010) The ENETS guidelines: the new TNM classification system. Tumori 96:806–809
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Jung Hoon Kim, M.D.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
Seungchul Han M.D. has significant statistical expertise, and no complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board. This study was approved by our Institutional Review Board, and informed patient consent was waived due to the retrospective nature of our study.
Ethical approval
Institutional Review Board approval was obtained (IRB; No. 1808–146-967).
Methodology
• retrospective
• diagnostic or prognostic study
• performed at one institution
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Han, S., Kim, J.H., Yoo, J. et al. Prediction of recurrence after surgery based on preoperative MRI features in patients with pancreatic neuroendocrine tumors. Eur Radiol 32, 2506–2517 (2022). https://doi.org/10.1007/s00330-021-08316-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-021-08316-8