Abstract
Objective
To evaluate potential MRI-defined effect modifiers of amoxicillin treatment in patients with chronic low back pain and type 1 or 2 Modic changes (MCs) at the level of a previous lumbar disc herniation (index level).
Methods
In a prospective trial (AIM), 180 patients (25–64 years; mean age 45; 105 women) were randomised to receive amoxicillin or placebo for 3 months. Primary outcome was the Roland-Morris Disability Questionnaire (RMDQ) score (0–24 scale) at 1 year. Mean RMDQ score difference between the groups at 1 year defined the treatment effect; 4 RMDQ points defined the minimal clinically important effect. Predefined baseline MRI features of MCs at the index level(s) were investigated as potential effect modifiers. The predefined primary hypothesis was a better effect of amoxicillin when short tau inversion recovery (STIR) shows more MC-related high signal. To evaluate this hypothesis, we pre-constructed a composite variable with three categories (STIR1/2/3). STIR3 implied MC-related STIR signal increases with volume ≥ 25% and height > 50% of vertebral body and maximum intensity increase ≥ 25% and presence on both sides of the disc. As pre-planned, interaction with treatment was analysed using ANCOVA in the per protocol population (n = 155).
Results
The STIR3 composite group (n = 41) and STIR signal volume ≥ 25% alone (n = 45) modified the treatment effect of amoxicillin. As hypothesised, STIR3 patients reported the largest effect (− 5.1 RMDQ points; 95% CI − 8.2 to − 1.9; p for interaction = 0.008).
Conclusions
Predefined subgroups with abundant MC-related index-level oedema on STIR modified the effect of amoxicillin. This finding needs replication and further support.
Key Points
• In the primary analysis of the AIM trial, the effect of amoxicillin in patients with chronic low back pain and type 1 or 2 MCs did not reach the predefined cut-off for clinical importance.
• In the present MRI subgroup analysis of AIM, predefined subgroups with abundant MC-related oedema on STIR reported an effect of amoxicillin.
• This finding requires replication and further support.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Modic changes (MCs) are magnetic resonance imaging (MRI) findings of vertebral bone marrow changes extending from the endplate. MCs are defined as type 1 (oedema type), 2 (fatty type), and 3 (sclerotic type) based on their intensity on T1- and T2-weighted MRI [1, 2]. However, the MC intensity and type depend on MRI scanning parameters and magnetic field strength [3, 4], and different MC types may represent stages of a common biological process [5]. This process may involve inflammation, fibrosis, high bone turnover, fatty infiltration, and sclerosis [1, 5, 6]. MCs were related to low back pain (LBP) in some studies but not in others [7,8,9]. The evidence for an association between MCs and LBP is stronger for type 1 than for type 2 or 3 MCs [10,11,12,13,14,15]. Proposed explanations for MCs include endplate damage, autoimmunity, and occult discitis [5]. Vertebral bone oedema resembling type 1 MCs is a common MRI finding in spondylodiscitis [16], and one theory is that MCs develop adjacent to a low-grade discitis region caused by haematogenic spread of Cutibacterium acnes bacteria to a previously disrupted, neo-vascularised lumbar disc [17, 18].
A previous trial reported a substantial effect of antibiotic treatment for chronic LBP with type 1 MCs on 0.2-T MRI [19]. Some of these MCs might have appeared as type 2 on 1.5-T MRI [4]. The recent AIM (Antibiotics In Modic changes) trial applied 1.5-T MRI [20] and reported a small but not clinically important effect of amoxicillin in chronic LBP patients with type 1 MCs (− 2.3 points on the Roland-Morris Disability Questionnaire (RMDQ)) and no effect for type 2 MCs (− 0.1 RMDQ points) [21]. Thus, the type 1 (oedema type) group tended to have a larger effect. More bone marrow oedema may be associated with worse pain and disability [22,23,24] and might indicate more severe disease with a larger potential for improvement. Therefore, we hypothesised a larger effect of amoxicillin in subgroups with more versus less MC-related oedema. It is relevant to assess subgroup effects across both MC types because both can contain inflammatory changes [25] and oedema [26].
Short tau inversion recovery (STIR) series are ideal for highlighting oedema. STIR suppresses a high signal from fat and often shows oedema in MCs classified as type 2 on T1/T2 series without fat suppression [26]. Although STIR is more sensitive to bone marrow oedema than standard T1/T2 series [26, 27], STIR can likewise not separate infectious from non-infectious causes [28, 29]. This subgroup study of the AIM trial included both STIR and standard fast spin echo T1/T2 sequences. We aimed to evaluate potential MRI-defined effect modifiers of amoxicillin treatment in patients with chronic LBP and type 1 or 2 MCs at the level of a previous lumbar disc herniation.
Materials and methods
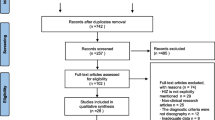
The AIM trial included 180 patients from six hospital outpatient clinics in Norway from June 2015 to September 2017 [20, 21]. All the eligibility criteria are detailed in the Appendix, Table A1. The inclusion criteria were age 18–65 years, LBP for more than 6 months with a mean intensity of at least 5 on three 0–10 numerical rating scales, lumbar disc herniation on MRI in the preceding 2 years, and type 1 or type 2 MCs (with height ≥ 10% of the vertebral height and diameter > 5 mm) at the previously herniated disc level. Trial flow chart, trial methods, and baseline characteristics are published [21]. The trial, this study, and statistical analysis plans are registered at ClinicalTrials.gov (identifier: NCT02323412).
Randomisation, treatment, and outcome measures
Patients were randomised to receive oral amoxicillin 750 mg or placebo (maize starch) three times daily for 3 months. The amoxicillin and placebo tablets had identical encapsulation, containers, and labelling. A third-party statistician used Stata 13 (StataCorp) to create randomisation lists. Allocation was stratified by prior disc surgery (yes/no) and MC type (type 1 (n = 118) or type 2 (n = 62) only) at the previously herniated disc level(s) with a 1:1:1:1 allocation and random block sizes of four and six [21]. The allocation sequence was concealed and centrally administered. Care providers gave patients a prescription with a computer-generated allocation number to be used at dedicated pharmacies. All care providers, research staff, statisticians, and patients were blinded to treatment allocation during data collection.
The primary endpoint was the RMDQ score (0–24 scale) at 1 year [30, 31]. The minimal clinically important difference in mean RMDQ score at 1 year between treatment groups (treatment effect) was predefined as 4 [20, 21]. The outcome at the end of the treatment period (3 months) was not primary because long-term improvement is desirable and the antibiotic group in the prior trial improved by 4.5 RMDQ points (0–23 scale) from the end of the treatment period to 1 year [19]. The Oswestry Disability Index (ODI) 2.0 (0–100 scale) [32] and LBP intensity (0–10 numeric rating scale) were secondary outcomes [21].
MRI assessment
Baseline MRI of the lumbar spine was performed at six centres using identical protocols and the same type of 1.5-T scanner with the same software version (Magnetom Avanto B19; Siemens). This MRI included sagittal T1- and T2-weighted fast spin echo (‘T1/T2’) and sagittal STIR images. The integrated spine array coil was used, but no surface coils. Echo time (ms)/repetition time (ms) was 11/575 for T1, 87/3700 for T2, and 70/5530 for STIR. Echo train length was 5 for T1, 17 for T2, and 20 for STIR. Matrix was 384 × 269 for T1/T2 and 320 × 224 for STIR. The inversion time for STIR was 160 ms. Slice thickness/spacing was 4 mm/0.4 mm and field of view was 300 mm × 300 mm for all three sequences. Other MRI parameters were also identical between centres [33].
Three radiologists (A.E., N.V., and P.M.K.) who were blinded to clinical outcomes and treatment allocation independently rated MRI findings [33]. All had > 10 years of experience in musculoskeletal MRI. The same three radiologists interpreted the MRIs from all study centres. On T1/T2, they rated primary (most extensive) and secondary MC types as type 1 (hypointense on T1, hyperintense on T2), type 2 (hyperintense on T1, iso- or hyperintense on T2), and type 3 (hypointense on T1 and T2) [33]. They evaluated the largest height and volume of MCs on T1/T2 and the largest height, volume and intensity of any MC-related STIR signal increase (Table 1), defined as a visible increase compared with normal vertebral bone marrow, located in or abutting a region with MC on T1/T2 or located and shaped as an MC [33].
We based the conclusive MRI findings on the radiologists’ majority rating or mean value of measurements made by two of them (A.E. and P.M.K. if all three agreed there was a lesion to measure). The inter-rater reliability of the MRI evaluations was previously reported [33]. Fleiss’ kappa values [34] for overall inter-rater agreement (mean values across four endplates L4-S1) were 0.88/0.81 for presence of any MCs/type 1 MCs, 0.64/0.69 for MC height/volume, 0.86 for presence of a STIR signal increase, and 0.51/0.56 (0.40/0.40 at L5/S1 inferior to disc) for STIR signal height/volume. For maximum MC-related STIR signal intensity on a 0–100% scale (0% = normal vertebral body; 100% = cerebrospinal fluid), largest mean of differences and widest 95% limits of agreement were 0.9% and ± 7.6%, respectively.
Predefined hypotheses and potential effect modifiers
In the AIM trial protocol, we hypothesised a better effect of amoxicillin when:
-
STIR shows more MC-related high signal (primary hypothesis)
-
MCs contain more type 1 than type 2 or are larger (explorative hypothesis)
The nine variables described in Table 1 were predefined as potential effect modifiers in the statistical analysis plan. All concerned MCs at the index level(s) with prior disc herniation because this level was hypothesised to contain low-grade discitis that was the target for treatment. One composite and four underlying variables concerned STIR signal extent and intensity. The STIR composite variable had three categories (STIR1/2/3) and was used to assess the primary hypothesis. STIR3 implied MC-related STIR signal increase with volume ≥ 25% and height > 50% of the vertebral body, maximum intensity increase ≥ 25%, and presence on both sides of the disc. One composite and three underlying variables concerned MC extent and type 1 degree on T1/T2. We constructed each composite variable by clinically plausible grouping of the underlying variables [35]. We did so before analysing the effect of any MRI variable on the outcome but were not blinded to the distribution of the variables in our sample.
Analyses
The baseline properties of the randomised groups were characterised using descriptive methods.
All pre-planned analyses are described in Table 2. Each effect modifier was analysed using ANCOVA with the outcome (RMDQ, ODI, or LBP intensity) at 1 year as the dependent variable and the randomisation group, effect modifier, and their interaction as independent variables adjusted for the baseline values of the outcome. Additionally, we adjusted for age and prior disc surgery because contamination during surgery is a potential cause of discitis. Supporting the use of ANCOVA, Levene’s test indicated homogeneity of variances, and QQ plots indicated normally distributed residuals and outcome variables without extreme outliers. If one or both composite MRI variables modified the treatment effect, we would include both in the same model to assess their independence [36]. Post hoc analyses, marked as such throughout the manuscript, are also described in Table 2.
The primary analyses were performed on the predefined per protocol (PP) population described in the Appendix, page 2. The intention to treat (ITT) population was used for supportive analyses. Missing outcome values were imputed using multiple imputation (details in footnote, Table 2).
We used a Bonferroni-corrected alpha of 0.05/6 (0.008) when testing the primary hypothesis (ranked as hypothesis six in the trial protocol) [20]. Otherwise, an alpha of 0.05 was applied to minimise type 2 errors [37]. Analyses were performed using Stata 16 (StataCorp), and figures were made using MATLAB 9.5 (MathWorks) or Stata 16.
Power calculation
The AIM trial was designed with 90% power in each MC type group [20]; 80% power in the total sample would have required 50 patients or 200 patients in a subgroup study with two equally large subgroups [38]. In this study with three subgroup categories, 80% power would have required > 200 patients. Adding covariates in the analyses improved the power [39], but our sample was still small.
Results
The 180 patients were aged 25–64 years (mean age 45 years; standard deviation 9 years); 105 (58%) patients were women. Table 3 shows baseline MRI findings by treatment group. Of 360 baseline and 1-year outcome values, 13 were missing for RMDQ, 14 for ODI, and 13 for LBP intensity. The results for the effect modifiers were similar in PP analyses (n = 155) (Figs. 1, 2, and 3) and ITT analyses (n = 180) (Appendix, Figs. A1–A3).
Roland-Morris Disability Questionnaire (RMDQ) for all effect modifiers (per protocol). RMDQ scores range from 0 (no disability) to 24 (maximum disability). Observed difference between treatment groups (mean ± 95% CI) and estimated coefficients (with 95% CI) for interaction from the ANCOVA (per protocol) with p values. PP, per protocol; CI, confidence interval; STIR, short tau inversion recovery; MC, Modic change. MC variables are based on T1- and T2-weighted fast spin echo images, not STIR
Oswestry Disability Index (ODI) for all effect modifiers (per protocol). ODI scores range from 0 (no disability) to 100 (maximum disability). Observed difference between treatment groups (mean ± 95% CI) and estimated coefficients (with 95% CI) for interaction from the ANCOVA (per protocol) with p values. Missing value not imputed in one patient (excluded). PP, per protocol; CI, confidence interval; STIR, short tau inversion recovery; MC, Modic change. MC variables are based on T1- and T2-weighted fast spin echo images, not STIR
Low back pain intensity for all effect modifiers (per protocol). Pain intensity scores range from 0 (no pain) to 10 (worst possible pain). Observed difference between treatment groups (mean ± 95% CI) and estimated coefficients (with 95% CI) for interaction from the ANCOVA (per protocol) with p values. Missing value not imputed in one patient (excluded). PP, per protocol; CI, confidence interval; STIR, short tau inversion recovery; MC, Modic change. MC variables are based on T1- and T2-weighted fast spin echo images, not STIR
Primary hypothesis—STIR
As hypothesised, the STIR3 group (n = 41) reported the largest effect of amoxicillin; the difference in mean RMDQ score at 1 year between those receiving amoxicillin and those receiving placebo (PP analysis) was − 5.1 (95% CI − 8.2 to − 1.9, p for interaction = 0.008) (Fig. 1). The corresponding difference was − 0.7 (95% CI − 3.1 to 1.7) in the STIR2 group and 1.1 (95% CI − 2.1 to 4.4) in the STIR1 group. The treatment effect in the STIR3 group was − 4.8 points (95% CI − 7.9 to − 1.8; p for interaction = 0.014) in the ITT analysis and − 4.5 RMDQ points (95% CI − 7.9 to − 1.1, p for interaction = 0.14) in the PP model including both composite MRI variables.
STIR volume ≥ 25% of the vertebral body (n = 45) also significantly modified the treatment effect (Fig. 1). In the STIR3 and STIR volume ≥ 25% groups, the effect of amoxicillin was > 4 RMDQ points (cut-off for clinical importance) and also evident for ODI (Fig. 2) but not for LBP intensity (Fig. 3).
Explorative hypothesis—T1/T2
The results for the composite MC variable based on T1/T2 did not reach statistical significance or clinical importance (Fig. 1). Two underlying subgroups significantly modified the treatment effect in favour of amoxicillin: MC volume ≥ 25% and MC height > 50% of the vertebral body (Fig. 1). The treatment effect within these subgroups did not exceed the threshold for clinical importance.
Post hoc analyses of STIR3
The baseline characteristics of the STIR3 patients were similar in both treatment groups (Appendix, Table A5). The STIR3 patients and total sample had similar mean baseline RMDQ scores (amoxicillin/placebo 12.8/12.6 vs. 12.7/12.8) and prior disc surgery rates (16% vs. 21%).
The number of STIR3 patients needed to be treated to achieve > 30% improved RMDQ score at 1 year was 3.1 (95% CI 1.7 to 27) (Appendix, Tables A2–A3). Among patients receiving amoxicillin, 6 of 22 STIR3 patients (27%) improved > 75% compared with 9 of 41 (22%) STIR2 patients and no STIR1 patients.
The treatment effect of amoxicillin in the STIR3 group was present at 3 months and remained until the end of the study at 1 year (Fig. 4), but the change in RMDQ score varied considerably between patients (Fig. 5).
Treatment effect over time for STIR3 patients (per protocol). Roland-Morris Disability Questionnaire score (0–24 scale), Oswestry Disability Index score (0–100 scale), and low back pain intensity (0–10 numerical rating scale) from baseline to 1 year in each treatment group. Higher scores imply worse disability/pain. The results are from post hoc analyses
Change in the Roland-Morris Disability Questionnaire (RMDQ) score (per protocol). The change in the RMDQ score (0–24 scale) from baseline to 1 year in each treatment group is plotted for STIR1, STIR2, and STIR3 patients; negative values denote improvement. The results are from post hoc analyses. STIR, short tau inversion recovery
Bangs blinding index for STIR3 patients was − 0.01 in the amoxicillin group, indicating perfect blinding, and 0.61 in the placebo group, indicating un-blinding (Appendix, Table A4).
Discussion
To our knowledge, this was the first study to investigate STIR-based effect modifiers of a treatment for chronic LBP with MCs. These effect modifiers were defined by MC-related high signal on STIR at the previously herniated index level(s) hypothesised to contain a low-grade discitis. The STIR3 and STIR volume ≥ 25% groups with abundant high signal modified the treatment effect of amoxicillin. STIR3 patients reported the largest effect (− 5.1 RMDQ points; 95% CI − 8.2 to − 1.9; p for interaction = 0.008). Subgroups based on T1/T2 features of MCs did not report a clinically important effect of amoxicillin. All subgroups were small, and the findings must be interpreted with caution.
Credibility of results
We consider the subgroup effect of STIR3 to have overall moderate credibility based on the criteria predefined in the statistical analysis plan [36] and the results of the post hoc analyses, but some criteria were not fulfilled (Table 4). The interaction of STIR3 and STIR volume ≥ 25% with treatment was found for the related outcomes RMDQ and ODI but not for LBP, and the finding has not yet been replicated in other studies. No tissue samples were taken, and STIR findings alone are not diagnostic for infection [28, 29]. Further data are needed to link extensive oedema on STIR to low-grade disc infection.
Post hoc responder analyses supported an effect of amoxicillin in the STIR3 group, but the estimates showed wide CIs (Appendix, Tables A2–A3). Similar to patients with verified Cutibacterium acnes discitis [40], STIR3 patients improved most during antibiotic treatment (Fig. 4). The clinical course in the STIR3 placebo group is difficult to evaluate for credibility because the natural course in untreated groups with abundant MC-related oedema on STIR is unknown. The STIR3 placebo group reported almost no improvement during the 1-year follow-up (Fig. 4). Placebo groups and sick-listed patients with persistent LBP and type 1 MCs also reported little improvement over 1 year in some studies: 0.5–1.4 points for RMDQ [19, 41, 42], 1.9 points for ODI [43], and 0–2.2 points for LBP [19, 41,42,43].
Incomplete blinding may have contributed to lack of improvement in our placebo group and an overestimated effect of amoxicillin. All patients were blinded to treatment allocation, but placebo patients still tended to suspect they were not on active treatment (Table A4). This might be due to a lack of treatment effect or lack of side effects [44]. AIM patients with little improvement at 3 months and no side effects were less likely to report at 1 year that they had received antibiotics [21]. The precise impact of incomplete blinding on outcome is unclear [45].
As hypothesised, amoxicillin had the largest effect on RMDQ and ODI in the assumed ‘worst’ category of all STIR variables (Figs. 1 and 2). This was not the case in the type 1 major category on T1/T2, and the effect of placebo in the group ‘MC volume <10%’ is difficult to explain and may be spurious (Fig. 1). Thus, the results for STIR variables appear more credible than the explorative T1/T2 results. Below, we further discuss the STIR3 results that correspond to our predefined primary hypothesis.
STIR3 results—interpretation and implications
The effect of amoxicillin was larger for STIR3 patients than for the original type 1 and type 2 only MC groups (− 2.3 and − 0.1 RMDQ points, respectively) in the primary analysis of AIM [19]. The disability at baseline was similar, not worse in the STIR3 group as expected, and cannot explain the difference. These findings make it relevant to examine patients with extensive MC-related oedema on STIR as a separate subgroup in future treatment studies.
It remains unclear why the treatment effect (RMDQ difference) at 1 year was smaller in the STIR3 group (5.1; 0–24 scale) than in the prior cohort with type 1 MCs (8.3; 0–23 scale) [19]. Baseline MC oedema cannot be compared because the prior trial applied 0.2-T MRI without STIR. Both cohorts had MCs at the level of a prior disc herniation. STIR3 patients had slightly lower baseline RMDQ scores than the previous cohort, less than 13 vs. 15 [19]; baseline LBP scores were similar, above 6.
The STIR3 results were consistent with the hypothesis that some MCs with abundant oedema on STIR might represent low-grade discitis. Importantly, spondylodiscitis was an exclusion criterion and was not suspected on MRI. The STIR3 findings were credible by most of the predefined criteria (Table 4) and the treatment course mirrored that of Cutibacterium acnes discitis.
However, replication of our findings is essential. The effect of amoxicillin in the STIR3 group varied greatly (Fig. 5) and was not evident for LBP intensity. The CI overlapped with the cut-off for clinical importance, bacterial infection was not verified, and un-blinding may have occurred. Additionally, adverse events and antibiotic resistance are potential harms [21].
The present findings support the use of STIR to evaluate MCs. They also motivate further studies of MC-related oedema on STIR in relation to possible biological markers of infection that are currently being investigated by our research group. To achieve an optimal classification of MCs for potential clinical use, MC characteristics not studied here, such as diffusion parameters [46], contrast enhancement, and bone turnover [6], should also be investigated.
Further work is needed to quantify STIR findings. The composite STIR variable was based on both visual assessments and several time-consuming manual measurements. The visually estimated STIR signal volume alone yielded similar results and might be more applicable in a clinical setting. However, precise measurements are preferable in research and may become more feasible with advanced automated techniques [47, 48]. To date, few studies have quantified spinal oedema on MRI [29, 49,50,51].
Strengths and limitations
The strengths of this study include predefined hypotheses, standardised MRI techniques, and MRI ratings by three experienced radiologists [52]. Additionally, potential effect modifiers were defined and categorised before analysing their modifying impact.
Subgroup studies of clinical trials often have limited statistical power and generalisability [36, 53, 54]. This phenomenon also applies to our study. Our pre-decision in the statistical analysis plan to perform primary PP analyses is debatable, although we also present secondary ITT results. The decision implied that we focused primarily on the effect of amoxicillin and secondarily on the effect of allocating patients to receive amoxicillin [55, 56]. The impact of MRI findings on the treatment effect in patients who did not follow their assigned treatment seemed less relevant to study. PP analyses can create prognostic differences between the treatment groups [55]. However, ITT analyses supported the PP findings.
We evaluated the MRIs at inclusion before defining the subgroups, and the definitions of the MRI subgroups were partly dependent on the MRI data [57]. Furthermore, the composite MRI variables had not been validated. The ratings of STIR signal height and volume were less reliable at L5/S1 inferior to the disc [33]. However, the conclusive rating based on multiple observers’ evaluations was likely more reliable than each observer’s rating [52]. When an MC contained both type 1 and another type, we classified the type 1 part as primary or secondary, but we did not measure its exact size or intensity. Our results may not apply to low-field or 3-T MRI. However, they are likely valid with similar 1.5-T MRI protocols [3] and STIR works well with both low- and high-field scanners [58, 59].
Conclusion
Predefined subgroups with chronic LBP, an index level with prior disc herniation, and abundant MC-related index-level oedema on STIR modified the treatment effect of amoxicillin. This finding shows moderate credibility based on published criteria and post hoc analyses and requires replication.
Abbreviations
- AIM:
-
Antibiotics in Modic changes
- CI:
-
Confidence interval
- ITT:
-
Intention to treat
- LBP:
-
Low back pain
- MCs:
-
Modic changes
- MRI:
-
Magnetic resonance imaging
- ODI:
-
Oswestry Disability Index
- PP:
-
Per protocol
- RMDQ:
-
Roland-Morris Disability Questionnaire
- STIR:
-
Short tau inversion recovery
- T1/T2:
-
T1- and T2-weighted fast spin echo images
References
Modic MT, Steinberg PM, Ross JS, Masaryk TJ, Carter JR (1988) Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Radiology 166:193–199
Modic MT, Masaryk TJ, Ross JS, Carter JR (1988) Imaging of degenerative disk disease. Radiology 168:177–186
Fields AJ, Battie MC, Herzog RJ et al (2019) Measuring and reporting of vertebral endplate bone marrow lesions as seen on MRI (Modic changes): recommendations from the ISSLS Degenerative Spinal Phenotypes Group. Eur Spine J 28:2266–2274
Bendix T, Sorensen JS, Henriksson GA, Bolstad JE, Narvestad EK, Jensen TS (2012) Lumbar Modic changes-a comparison between findings at low- and high-field magnetic resonance imaging. Spine (Phila Pa 1976) 37:1756–1762
Dudli S, Fields AJ, Samartzis D, Karppinen J, Lotz JC (2016) Pathobiology of Modic changes. Eur Spine J 25:3723–3734
Jarvinen J, Niinimaki J, Karppinen J, Takalo R, Haapea M, Tervonen O (2020) Does bone scintigraphy show Modic changes associated with increased bone turnover? Eur J Radiol Open 7:100222
Herlin C, Kjaer P, Espeland A et al (2018) Modic changes-their associations with low back pain and activity limitation: a systematic literature review and meta-analysis. PLoS One 13:e0200677
Jensen TS, Karppinen J, Sorensen JS, Niinimaki J, Leboeuf-Yde C (2008) Vertebral endplate signal changes (Modic change): a systematic literature review of prevalence and association with non-specific low back pain. Eur Spine J 17:1407–1422
Mok FP, Samartzis D, Karppinen J, Fong DY, Luk KD, Cheung KM (2016) Modic changes of the lumbar spine: prevalence, risk factors, and association with disc degeneration and low back pain in a large-scale population-based cohort. Spine J 16:32–41
Brinjikji W, Diehn FE, Jarvik JG et al (2015) MRI findings of disc degeneration are more prevalent in adults with low back pain than in asymptomatic controls: a systematic review and meta-analysis. AJNR Am J Neuroradiol 36:2394–2399
Hanimoglu H, Cevik S, Yilmaz H et al (2019) Effects of Modic type 1 changes in the vertebrae on low back pain. World Neurosurg 121:e426–e432
Maatta JH, Karppinen J, Paananen M et al (2016) Refined phenotyping of Modic changes: imaging biomarkers of prolonged severe low back pain and disability. Medicine (Baltimore) 95:e3495
Splendiani A, Bruno F, Marsecano C et al (2019) Modic I changes size increase from supine to standing MRI correlates with increase in pain intensity in standing position: uncovering the “biomechanical stress” and “active discopathy” theories in low back pain. Eur Spine J 28:983–992
Jensen RK, Leboeuf-Yde C, Wedderkopp N, Sorensen JS, Jensen TS, Manniche C (2012) Is the development of Modic changes associated with clinical symptoms? A 14-month cohort study with MRI. Eur Spine J 21:2271–2279
Saukkonen J, Maatta J, Oura P et al (2020) Association between Modic changes and low back pain in middle age: a northern Finland birth cohort study. Spine (Phila Pa 1976) 45:1360–1367
Mavrogenis AF, Megaloikonomos PD, Igoumenou VG et al (2017) Spondylodiscitis revisited. EFORT Open Rev 2:447–461
Albert HB, Lambert P, Rollason J et al (2013) Does nuclear tissue infected with bacteria following disc herniations lead to Modic changes in the adjacent vertebrae? Eur Spine J 22:690–696
Capoor MN, Birkenmaier C, Wang JC et al (2019) A review of microscopy-based evidence for the association of Propionibacterium acnes biofilms in degenerative disc disease and other diseased human tissue. Eur Spine J 28:2951–2971
Albert HB, Sorensen JS, Christensen BS, Manniche C (2013) Antibiotic treatment in patients with chronic low back pain and vertebral bone edema (Modic type 1 changes): a double-blind randomized clinical controlled trial of efficacy. Eur Spine J 22:697–707
Storheim K, Espeland A, Grovle L et al (2017) Antibiotic treatment in patients with chronic low back pain and Modic changes (the AIM study): study protocol for a randomised controlled trial. Trials 18:596
Braten LCH, Rolfsen MP, Espeland A et al (2019) Efficacy of antibiotic treatment in patients with chronic low back pain and Modic changes (the AIM study): double blind, randomised, placebo controlled, multicentre trial. BMJ 367:l5654
Homagk L, Marmelstein D, Homagk N, Hofmann GO (2019) SponDT (spondylodiscitis diagnosis and treatment): spondylodiscitis scoring system. J Orthop Surg Res 14:100
Tonbul M, Guzelant AY, Gonen A, Baca E, Ozbaydar MU (2011) Relationship between the size of bone marrow edema of the talus and ankle pain. J Am Podiatr Med Assoc 101:430–436
Unay K, Poyanli O, Akan K, Guven M, Demircay C (2009) The relationship between bone marrow edema size and knee pain. Knee Surg Sports Traumatol Arthrosc 17:1298–1304
Dudli S, Sing DC, Hu SS et al (2017) Intervertebral disc/bone marrow cross-talk with Modic changes. Eur Spine J. https://doi.org/10.1007/s00586-017-4955-4
Finkenstaedt T, Del Grande F, Bolog N et al (2017) Modic type 1 changes: detection performance of fat-suppressed fluid-sensitive MRI sequences. Rofo 190:152–160
Jimenez-Boj E, Nobauer-Huhmann I, Hanslik-Schnabel B et al (2007) Bone erosions and bone marrow edema as defined by magnetic resonance imaging reflect true bone marrow inflammation in rheumatoid arthritis. Arthritis Rheum 56:1118–1124
Shrot S, Sayah A, Berkowitz F (2017) Can the pattern of vertebral marrow oedema differentiate intervertebral disc infection from degenerative changes? Clin Radiol 72:613.e7–613.e11
Schwarz-Nemec U, Friedrich KM, Stihsen C et al (2020) Vertebral bone marrow and endplate assessment on MR imaging for the differentiation of Modic type 1 endplate changes and infectious spondylodiscitis. J Clin Med 9:826
Roland M, Fairbank J (2000) The Roland-Morris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine (Phila Pa 1976) 25:3115–3124
Grotle M, Brox JI, Vollestad NK (2003) Cross-cultural adaptation of the Norwegian versions of the Roland-Morris Disability Questionnaire and the Oswestry Disability Index. J Rehabil Med 35:241–247
Fairbank JC, Pynsent PB (2000) The Oswestry Disability Index. Spine (Phila Pa 1976) 25:2940–2952
Kristoffersen PM, Vetti N, Storheim K et al (2020) Short tau inversion recovery MRI of Modic changes: a reliability study. Acta Radiol Open 9:2058460120902402
Fleiss JL (1981) Statistical methods for rates and proportions. 2nd ed. John Wiley, New York, pp. 38–46
Song MK, Lin FC, Ward SE, Fine JP (2013) Composite variables: when and how. Nurs Res 62:45–49
Sun X, Briel M, Walter SD, Guyatt GH (2010) Is a subgroup effect believable? Updating criteria to evaluate the credibility of subgroup analyses. BMJ 340:c117
Kent P, Keating JL, Leboeuf-Yde C (2010) Research methods for subgrouping low back pain. BMC Med Res Methodol 10:62
Brookes ST, Whitely E, Egger M, Smith GD, Mulheran PA, Peters TJ (2004) Subgroup analyses in randomized trials: risks of subgroup-specific analyses; power and sample size for the interaction test. J Clin Epidemiol 57:229–236
Lingsma H, Roozenbeek B, Steyerberg E, IMPACT investigators (2010) Covariate adjustment increases statistical power in randomized controlled trials. J Clin Epidemiol 63:1391
Uckay I, Dinh A, Vauthey L et al (2010) Spondylodiscitis due to Propionibacterium acnes: report of twenty-nine cases and a review of the literature. Clin Microbiol Infect 16:353–358
Jensen OK, Nielsen CV, Sorensen JS, Stengaard-Pedersen K (2014) Type 1 Modic changes was a significant risk factor for 1-year outcome in sick-listed low back pain patients: a nested cohort study using magnetic resonance imaging of the lumbar spine. Spine J 14:2568–2581
Jensen OK, Andersen MH, Ostgard RD, Andersen NT, Rolving N (2019) Probiotics for chronic low back pain with type 1 Modic changes: a randomized double-blind, placebo-controlled trial with 1-year follow-up using Lactobacillus Rhamnosis GG. Eur Spine J 28:2478–2248
Koivisto K, Kyllonen E, Haapea M et al (2014) Efficacy of zoledronic acid for chronic low back pain associated with Modic changes in magnetic resonance imaging. BMC Musculoskelet Disord 15:64
Schulz KF, Grimes DA (2002) Blinding in randomised trials: hiding who got what. Lancet 359:696–700
Moustgaard H, Clayton GL, Jones HE et al (2020) Impact of blinding on estimated treatment effects in randomised clinical trials: meta-epidemiological study. BMJ 368:l6802
Bray TJP, Sakai N, Dudek A et al (2020) Histographic analysis of oedema and fat in inflamed bone marrow based on quantitative MRI. Eur Radiol 30:5099–5109
Griffith JF, Wang D, Shi L, Yeung DK, Lee R, Shan TL (2015) Computer-aided assessment of spinal inflammation on magnetic resonance images in patients with spondyloarthritis. Arthritis Rheumatol 67:1789–1797
Jamaludin A, Lootus M, Kadir T et al (2017) ISSLS PRIZE IN BIOENGINEERING SCIENCE 2017: automation of reading of radiological features from magnetic resonance images (MRIs) of the lumbar spine without human intervention is comparable with an expert radiologist. Eur Spine J 26:1374–1383
Chronaiou I, Thomsen RS, Huuse EM et al (2017) Quantifying bone marrow inflammatory edema in the spine and sacroiliac joints with thresholding. BMC Musculoskelet Disord 18:497
Tibiletti M, Ciavarro C, Bari V et al (2017) Semi-quantitative evaluation of signal intensity and contrast-enhancement in Modic changes. Eur Radiol Exp 1:5
Wang Y, Videman T, Niemelainen R, Battie MC (2011) Quantitative measures of Modic changes in lumbar spine magnetic resonance imaging: intra- and inter-rater reliability. Spine (Phila Pa 1976) 36:1236–1243
Espeland A, Vetti N, Krakenes J (2013) Are two readers more reliable than one? A study of upper neck ligament scoring on magnetic resonance images. BMC Med Imaging 13:4
Assmann SF, Pocock SJ, Enos LE, Kasten LE (2000) Subgroup analysis and other (mis)uses of baseline data in clinical trials. Lancet 355:1064–1069
Cuzick J (2005) Forest plots and the interpretation of subgroups. Lancet 365:1308
Gupta SK (2011) Intention-to-treat concept: a review. Perspect Clin Res 2:109–112
Shrier I, Steele RJ, Verhagen E, Herbert R, Riddell CA, Kaufman JS (2014) Beyond intention to treat: what is the right question? Clin Trials 11:28–37
Rothwell PM (2005) Treating individuals 2. Subgroup analysis in randomised controlled trials: importance, indications, and interpretation. Lancet 365:176–186
Del Grande F, Santini F, Herzka DA et al (2014) Fat-suppression techniques for 3-T MR imaging of the musculoskeletal system. Radiographics 34:217–233
Delfaut EM, Beltran J, Johnson G, Rousseau J, Marchandise X, Cotten A (1999) Fat suppression in MR imaging: techniques and pitfalls. Radiographics 19:373–382
Acknowledgements
The authors thank their collaborators in the AIM study group for their contributions.
Funding
This study has received funding by the South East Norway Regional Health Authority (grant no. 2015-090) and the Western Norway Regional Health Authority (grant nos. HV 911891 and HV 911938), which had no part in the planning, performing, or reporting of the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Per Martin Kristoffersen.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was obtained from all patients in this study.
Ethical approval
Institutional Review Board approval was obtained from the Regional Committee for Medical Research Ethics – South East Norway (reference no. 2014/158).
Study subjects or cohorts overlap
Some study subjects or cohorts have been previously reported in (a) Braten LCH et al Efficacy of antibiotic treatment in patients with chronic low back pain and Modic changes (the AIM study): double blind, randomised, placebo controlled, multicentre trial. BMJ 2019;367:l5654, (b) Kristoffersen PM et al Short tau inversion recovery MRI of Modic changes: a reliability study. Acta Radiol Open 2020;9(1):2058460120902402, (c) Braten LCH et al Association of Modic change types and their short tau inversion recovery signals with clinical characteristics- a cross sectional study of chronic low back pain patients in the AIM study. BMC Musculoskelet Disord 2020;21(1):368, (d) Grotle M et al Cost-utility analysis of antibiotic treatment in patients with chronic low back pain and Modic changes: results from a randomised, placebo-controlled trial in Norway (the AIM study). BMJ Open 2020;10(6):e035461, and (e) Braten LCH et al Clinical effect modifiers of antibiotic treatment in patients with chronic low back pain and Modic changes - Secondary analyses of a randomised, placebo-controlled trial (the AIM study) (accepted, BMC Musculoskelet Disord).
Methodology
• prospective
• randomised controlled trial (subgroup analysis)
• multicentre study
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 683 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kristoffersen, P.M., Bråten, L.C.H., Vetti, N. et al. Oedema on STIR modified the effect of amoxicillin as treatment for chronic low back pain with Modic changes—subgroup analysis of a randomized trial. Eur Radiol 31, 4285–4297 (2021). https://doi.org/10.1007/s00330-020-07542-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-07542-w